Abstract
Background
Studies indicate that low graft-to-recipient weight ratio (GRWR) affect graft survival in adult-to-adult living donor liver transplantation. However, the potential role of GRWR in the prognosis of patients following living donor liver transplantation according to patient characteristics remains controversial. This study aimed to update the role of GRWR in patients following living donor liver transplantation.
Methods
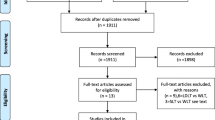
PubMed, Embase, and Cochrane Library were comprehensively searched for studies comparing low GRWR (< 0.8%) with normal GRWR (≥ 0.8%) in the prognosis following living donor liver transplantation from inception to March 2019. The 1-, 3-, and 5-year summary survival rates, small-for-size syndrome (SFSS), perioperative mortality, biliary complications, postoperative bleeding, and acute rejection were calculated using the random-effects model.
Results
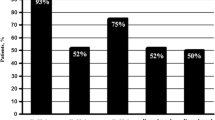
Eighteen studies comprising 4001 patients were included. Patients with low GRWR were associated with lower 1-year and 3-year survival rates compared to patients with normal GRWR, while no significant difference was found in the association of 5-year survival rate with low and normal GRWRs. Moreover, the risk of SFSS significantly increased in patients with low GRWR. Finally, no significant differences were observed in the association of low and normal GRWRs with the risk of perioperative mortality, biliary complications, postoperative bleeding, and acute rejection.
Conclusion
The results of this study indicated that low GRWR was associated with poor prognosis for patients following living donor liver transplantation, especially in terms of 1- and 3-year survival rates and SFSS.









Similar content being viewed by others
References
Broelsch CE, Emond JC, Whitington PF, Thistlethwaite JR, Baker AL, Lichtor JL. Application of reduced-size liver transplants as split grafts, auxiliary orthotopic grafts, and living related segmental transplants. Ann Surg 1990;212:368-375; discussion 375-367.
Lo CM, Fan ST, Liu CL, Wei WI, Lo RJ, Lai CL, Chan JK, Ng IO, Fung A, Wong J. Adult-to-adult living donor liver transplantation using extended right lobe grafts. Ann Surg 1997;226:261-269; discussion 269-270.
Humar A, Ganesh S, Jorgensen D, Tevar A, Ganoza A, Molinari M, Hughes C. Adult living donor versus deceased donor liver transplant (LDLT versus DDLT) at a single center: time to change our paradigm for liver transplant. Annals Surg 2019; 270:444-451.
Kiuchi T, Kasahara M, Uryuhara K, Inomata Y, Uemoto S, Asonuma K, Egawa H, Fujita S, Hayashi M, Tanaka K. Impact of graft size mismatching on graft prognosis in liver transplantation from living donors. Transplantation 1999;67:321-327.
Dahm F, Georgiev P, Clavien PA. Small-for-size syndrome after partial liver transplantation: definition, mechanisms of disease and clinical implications. Am J Transplant 2005;5:2605-2610.
Hill MJ, Hughes M, Jie T, Cohen M, Lake J, Payne WD, Humar A. Graft weight/recipient weight ratio: how well does it predict outcome after partial liver transplants? Liver Transpl 2009;15:1056-1062.
Nishizaki T, Ikegami T, Hiroshige S, Hashimoto K, Uchiyama H, Yoshizumi T, Kishikawa K, Shimada M, Sugimachi K. Small graft for living donor liver transplantation. Ann Surg 2001;233:575-580.
Yagi S, Uemoto S. Small-for-size syndrome in living donor liver transplantation. Hepatobiliary Pancreat Dis Int 2012;11:570-576.
Umeda Y, Yagi T, Sadamori H, Matsukawa H, Matsuda H, Shinoura S, Mizuno K, Yoshida R, Iwamoto T, Satoh D, Tanaka N. Effects of prophylactic splenic artery modulation on portal overperfusion and liver regeneration in small-for-size graft. Transplantation 2008;86:673-680.
Ogura Y, Hori T, El Moghazy WM, Yoshizawa A, Oike F, Mori A, Kaido T, Takada Y, Uemoto S. Portal pressure <15 mm Hg is a key for successful adult living donor liver transplantation utilizing smaller grafts than before. Liver Transpl 2010;16:718-728.
Troisi R, Ricciardi S, Smeets P, Petrovic M, Van Maele G, Colle I, Van Vlierberghe H, de Hemptinne B. Effects of hemi-portocaval shunts for inflow modulation on the outcome of small-for-size grafts in living donor liver transplantation. Am J Transplant 2005;5:1397-1404.
Miller CM, Durand F, Heimbach JK, Kim-Schluger L, Lee SG, Lerut J, Lo CM, Quintini C, Pomfret EA. The international liver transplant society guideline on living liver donation. Transplantation 2016;100: 1238-1243.
Miller CM, Quintini C, Dhawan A, Durand F, Heimbach JK, Kim-Schluger HL, Kyrana E, Lee SG, Lerut J, Lo CM, Pomfret EA. The international liver transplantation society living donor liver transplant recipient guideline. Transplantation 2017;101:938–944
Wakade VA and Mathur SK. Donor Safety in Live-Related Liver Transplantation. Indian J Surg 2012;74: 118–126.
Uemura T, Wada S, Kaido T, Mori A, Ogura Y, Yagi S, Fujimoto Y, Ogawa K, Hata K, Yoshizawa A, Okajima H, Uemoto S. How far can we lower graft-to-recipient weight ratio for living donor liver transplantation under modulation of portal venous pressure? Surgery 2016;159: 1623-30.
Agarwal S, Selvakumar N, Rajasekhar K, Dey R, Verma S, Gupta S. Minimum absolute graft weight of 650 g predicts a good outcome in living donor liver transplant despite a graft recipient body weight ratio of less than 0.8. Clinical transplantation. 2019;33:e13705.
Moher D, Liberati A, Tetzlaff J, Altman DG, Group P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097.
Wells G, Shea B, O’Connell D. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa: Ottawa Hospital Research Institute 2009 http://www.ohri.ca/programs/clinical_epidemiology/oxford.htm.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials 1986;7:177-188.
Ades AE, Lu G, Higgins JP. The interpretation of random-effects meta-analysis in decision models. Med Decis Making 2005;25:646-654.
Deeks J, Higgins J, Altman D. Analyzing data and undertaking meta-analyses. In: Higgins J, Green S, eds. Cochrane Handbook for Systematic Reviews of Interventions 501 Oxford: The Cochrane Collaboration, 2008; chap 9.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ 2003;327:557-560.
Tobias A. Assessing the influence of a single study in meta-analysis. Stata Tech Bull 1999;47:15–17.
Altman DG, Bland JM. Interaction revisited: the difference between two estimates. BMJ 2003;326:219.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997;315:629-634.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics 1994;50:1088-1101.
Lee HH, Joh JW, Lee KW, Kim SJ, Lee DS, Park JH, Choi SH, Heo JS, Hyon WS, Kwak MS, Lee SK. Small-for-size graft in adult living-donor liver transplantation. Transplant Proc 2004;36:2274-2276.
Selzner M, Kashfi A, Cattral MS, Selzner N, Greig PD, Lilly L, McGilvray ID, Therapondos G, Adcock LE, Ghanekar A, Levy GA, Renner EL, Grant DR. A graft to body weight ratio less than 0.8 does not exclude adult-to-adult right-lobe living donor liver transplantation. Liver Transpl 2009;15:1776-1782.
Moon JI, Kwon CH, Joh JW, Jung GO, Choi GS, Park JB, Kim JM, Shin M, Kim SJ, Lee SK. Safety of small-for-size grafts in adult-to-adult living donor liver transplantation using the right lobe. Liver Transpl 2010;16:864-869.
Gyoten K, Mizuno S, Tanemura A. Impact of the regulation of portal venous pressure on the small-for-size graft in adult living donor liver transplantation. Am J Transpl 2010;10:101-102.
Kaido T, Mori A, Ogura Y, Hata K, Yoshizawa A, Iida T, Yagi S, Uemoto S. Lower limit of the graft-to-recipient weight ratio can be safely reduced to 0.6% in adult-to-adult living donor liver transplantation in combination with portal pressure control. Transplant Proc 2011;43:2391-2393.
Lei JY, Yan LN, Li B, Wen TF, Wang WT, Xu MQ, Yang JY. Graft size alone should not affect donors selection and be used to predict the prognosis of recipients after living donor liver transplantation. Hepatogastroenterology 2012;59:224-227.
Ishizaki Y, Kawasaki S, Sugo H, Yoshimoto J, Fujiwara N, Imamura H. Left lobe adult-to-adult living donor liver transplantation: Should portal inflow modulation be added? Liver Transpl 2012;18:305-314.
Lee SD, Kim SH, Kim YK, Lee SA, Park SJ. Graft-to-recipient weight ratio lower to 0.7% is safe without portal pressure modulation in right-lobe living donor liver transplantation with favorable conditions. Hepatobiliary Pancreat Dis Int 2014;13:18-24.
Vasavada B, Chen CL, Zakaria M. Using low graft/recipient’s body weight ratio graft with portal flow modulation an effective way to prevent small-for-size syndrome in living-donor liver transplant: a retrospective analysis. Exp Clin Transplant 2014;12:437-442.
Chen PX, Yan LN, Wang WT. Outcome of patients undergoing right lobe living donor liver transplantation with small-for-size grafts. World J Gastroenterol 2014;20:282-289.
Hu Z, Zhong X, Zhou J, Xiang J, Li Z, Zhang M, Wu J, Jiang W, Zheng S. Smaller grafts do not imply early recurrence in recipients transplanted for hepatocellular carcinoma: A Chinese experience. Sci Rep 2016;6:26487.
Klair T, Przybyszewski E, Samstein B. Outcomes of small-for-size grafts in adult living donor liver transplantation. Am J Transplant 2016;16:71-72.
Matsuyama T, Iida T, Masuda K. Clinical outcome of adult living donor liver transplantation using small for size grafts. J Hepatobiliary Pancreat Sci 2017;24:A372.
Sethi P, Thillai M, Thankamonyamma BS, Mallick S, Gopalakrishnan U, Balakrishnan D, Menon RN, Surendran S, Dhar P, Othiyil Vayoth S. Living Donor Liver Transplantation Using Small-for-Size Grafts: Does Size Really Matter? J Clin Exp Hepatol 2018;8:125-131.
Lee EC, Kim SH, Shim JR, Park SJ. Small-for-size grafts increase recurrence of hepatocellular carcinoma in liver transplantation beyond milan criteria. Liver Transpl 2018;24:35-43.
Goja S, Kumar Yadav S, Singh Soin A. Readdressing the Middle Hepatic Vein in Right Lobe Liver Donation: Triangle of Safety. Liver Transpl 2018;24:1363-1376.
Iesari S, Inostroza Nunez ME, Rico Juri JM, Ciccarelli O, Bonaccorsi-Riani E, Coubeau L, Laterre PF, Goffette P, De Reyck C, Lengele B, Gianello P, Lerut J. Adult-to-adult living-donor liver transplantation: The experience of the Universite catholique de Louvain. Hepatobiliary Pancreat Dis Int 2019;18:132-142.
Duvall S, Tweedie R. A nonparametric “trim and fill” method for assessing publication bias in meta-analysis. J Am Stat Assoc 2000;95:89–98.
Bell R, Pandanaboyana S, Upasani V, Prasad R. Impact of graft-to-recipient weight ratio on small-for-size syndrome following living donor liver transplantation. ANZ J Surg 2018;88:415-420.
Yan Y, Zheng DF, Pu JL, Wu ZJ. Outcomes of adult patients adopting small-for-size grafts in living donor liver transplantation: A systematic review and meta-analysis. Hepatobiliary Pancreat Dis Int 2019.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Feng, Y., Han, Z., Wang, X. et al. Association of Graft-to-Recipient Weight Ratio with the Prognosis Following Liver Transplantation: a Meta-analysis. J Gastrointest Surg 24, 1869–1879 (2020). https://doi.org/10.1007/s11605-020-04598-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04598-3