Abstract
Purpose
Our aim was to compare postoperative outcomes of laparoscopic and open appendectomies for acute appendicitis in children under the circumstance of widespread use of laparoscopic surgery.
Method
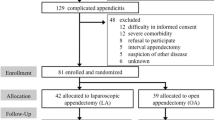
This study included data on laparoscopic and open appendectomies in children with acute appendicitis from the National Clinical Database, which is a Japanese nationwide surgical database, in 2015. The occurrence rates of complications within 30 days after the surgery and postoperative hospital stay were compared by univariate and multivariate analyses. p < 0.05 was considered statistically significant.
Results
This study included 4489 appendectomies, of which 3166 surgeries (70.5%) were performed laparoscopically. Appendectomy was performed for complicated and uncomplicated appendicitis in 1765 (39.3%) and 2724 cases (60.7%), respectively. Postoperative complications within 30 days were observed in 246 operations (5.5%). Organ-space surgical site infection (SSI), deep wound SSIs, and superficial wound SSIs were observed in 2.3%, 1.0%, and 2.4% of operations, respectively. On multivariate analysis, the incidence of postoperative complications (odds ratio 1.21, 95% CI 0.90–1.64, p = 0.207) and the length of hospital stay (median 4 days in both groups, p = 0.835) were not significantly different between patients who underwent laparoscopic or open appendectomy. Subgroup analysis in complicated and uncomplicated appendicitis cases also demonstrated no significant differences in the incidence of postoperative complications between those who underwent laparoscopic or open appendectomy.
Conclusion
This study suggested that the occurrence of postoperative complication and the length of hospital stay in pediatric patients who underwent laparoscopic appendectomy are similar with those in pediatric patients who underwent open appendectomy for acute appendicitis.


Similar content being viewed by others

References
Canty TG, Sr., Collins D, Losasso B, Lynch F, Brown C. Laparoscopic appendectomy for simple and perforated appendicitis in children: the procedure of choice? J Pediatr Surg. 2000;35:1582–5.
McKinlay R, Neeleman S, Klein R, Stevens K, Greenfeld J, Ghory M et al. Intraabdominal abscess following open and laparoscopic appendectomy in the pediatric population. Surg Endosc. 2003;17:730–3.
Varlet F, Tardieu D, Limonne B, Metafiot H, Chavrier Y. Laparoscopic versus open appendectomy in children--comparative study of 403 cases. Eur J Pediatr Surg. 1994;4:333–7.
Dai L, Shuai J. Laparoscopic versus open appendectomy in adults and children: A meta-analysis of randomized controlled trials. United European Gastroenterol J. 2017;5:542–53.
Page AJ, Pollock JD, Perez S, Davis SS, Lin E, Sweeney JF. Laparoscopic versus open appendectomy: an analysis of outcomes in 17,199 patients using ACS/NSQIP. J Gastrointest Surg. 2010;14:1955–62.
Aziz O, Athanasiou T, Tekkis PP, Purkayastha S, Haddow J, Malinovski V et al. Laparoscopic versus open appendectomy in children: a meta-analysis. Ann Surg. 2006;243:17–27.
Gotoh M, Miyata H, Hashimoto H, Wakabayashi G, Konno H, Miyakawa S et al. National Clinical Database feedback implementation for quality improvement of cancer treatment in Japan: from good to great through transparency. Surg Today. 2016;46:38–47.
The National Clnical Database http://www.ncd.or.jp/. 2018. Accessed 2/21/2018 2018.
Markar SR, Blackburn S, Cobb R, Karthikesalingam A, Evans J, Kinross J et al. Laparoscopic versus open appendectomy for complicated and uncomplicated appendicitis in children. J Gastrointest Surg. 2012;16:1993–2004.
Gosemann JH, Lange A, Zeidler J, Blaser J, Dingemann C, Ure BM et al. Appendectomy in the pediatric population-a German nationwide cohort analysis. Langenbecks Arch Surg. 2016;401:651–9.
Sauerland S, Jaschinski T, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2010;6.
Jen HC, Shew SB. Laparoscopic versus open appendectomy in children: outcomes comparison based on a statewide analysis. J Surg Res. 2010;161:13–7.
Kelly KN, Fleming FJ, Aquina CT, Probst CP, Noyes K, Pegoli W et al. Disease severity, not operative approach, drives organ space infection after pediatric appendectomy. Ann Surg. 2014;260:466–71.
Masoomi H, Mills S, Dolich MO, Ketana N, Carmichael JC, Nguyen NT et al. Comparison of outcomes of laparoscopic versus open appendectomy in children: data from the Nationwide Inpatient Sample (NIS), 2006-2008. World J Surg. 2012;36:573–8.
Murata A, Mayumi T, Muramatsu K, Ohtani M, Matsuda S. Effect of hospital volume on outcomes of laparoscopic appendectomy for acute appendicitis: an observational study. J Gastrointest Surg. 2015;19:897–904.
Smink DS, Finkelstein JA, Kleinman K, Fishman SJ. The effect of hospital volume of pediatric appendectomies on the misdiagnosis of appendicitis in children. Pediatrics. 2004;113:18–23.
Smink DS, Fishman SJ, Kleinman K, Finkelstein JA. Effects of race, insurance status, and hospital volume on perforated appendicitis in children. Pediatrics. 2005;115:920–5.
Wei PL, Liu SP, Keller JJ, Lin HC. Volume-outcome relation for acute appendicitis: evidence from a nationwide population-based study. PLoS One. 2012;7:26.
Presentation at a Scientific Meeting
This paper was based on an abstract presented at the 51st annual scientific meeting of the Pacific Association of Pediatric Surgeons, May 13–17, 2018, in Sapporo, Japan.
Funding
This work was supported by JSPS KAKENHI (Grant-in-Aid for Scientific Research (C) Grant Number JP16K11340).
Author information
Authors and Affiliations
Contributions
Conception of the study: JF, EW, TI. Analysis and interpretation: JF, EW, NH, KT, HT, HM. Drafting the manuscript: JF. Reviewing the manuscript: JF, EW, NH, KT, HT, TI, HM.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Fujishiro, J., Watanabe, E., Hirahara, N. et al. Laparoscopic Versus Open Appendectomy for Acute Appendicitis in Children: a Nationwide Retrospective Study on Postoperative Outcomes. J Gastrointest Surg 25, 1036–1044 (2021). https://doi.org/10.1007/s11605-020-04544-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-020-04544-3