Abstract
Clostridium difficile infection remains a common nosocomial illness with a significant impact on health care delivery. As molecular phenotyping of this organism has changed our understanding of its transmission and virulence, so too have diagnostic methods and treatment strategies evolved in recent years. The burden of this infection falls predominantly on elderly patients with comorbidities who have recently received antibiotics. Oral or enteral vancomycin is now preferred for first-line antimicrobial treatment across the disease spectrum, including mild-moderate initial cases. Fidaxomicin (a novel macrolide antibiotic), bezlotoxumab (a monoclonal antibody against toxin TcdB), and fecal microbiota transplantation expand the therapeutic armamentarium, particularly for recurrent infection. Operative treatment should be reserved for patients with fulminant infection, and early identification of patients who would benefit from an operation remains a challenge. Less invasive surgical options—such as laparoscopic diverting ileostomy with colonic irrigation—may improve survival and other outcomes relative to total abdominal colectomy and represent an attractive alternative particularly for frail patients.

Similar content being viewed by others
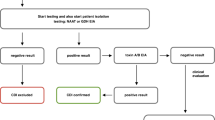
Abbreviations
- CDI:
-
Clostridium difficile infection
- PPI:
-
Proton pump inhibitor
- rCDI:
-
Recurrent Clostridium difficile infection
- NAAT:
-
Nucleic acid amplification test
- FMT:
-
Fecal microbiota transplant
- NSQIP:
-
National Surgical Quality Improvement Program
- GIL:
-
Gastrointestinal lavage
References
Lessa FC, Winston LG, McDonald LC. Burden of Clostridium difficile infection in the United States. N Engl J Med 2015;372: 2369-70.
McGlone SM, Bailey RR, Zimmer SM, Popovich MJ, Tian Y, Ufberg P, et al. The economic burden of Clostridium difficile. Clin Microbiol Infect 2012;18: 282-9.
Zimlichman E, Henderson D, Tamir O, Franz C, Song P, Yamin CK, et al. Health care-associated infections: a meta-analysis of costs and financial impact on the US health care system. JAMA Intern Med 2013;173: 2039-46.
McDonald LC, Gerding DN, Johnson S, Bakken JS, Carroll KC, Coffin SE, et al. Clinical practice guidelines for Clostridium difficile infection in adults and children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Clin Infect Dis 2018;66: e1-e48.
Poutanen SM, Simor AE. Clostridium difficile-associated diarrhea in adults. CMAJ 2004;171: 51-8.
Carchman EH, Peitzman AB, Simmons RL, Zuckerbraun BS. The role of acute care surgery in the treatment of severe, complicated Clostridium difficile-associated disease. J Trauma Acute Care Surg 2012;73: 789-800.
See I, Mu Y, Cohen J, Beldavs ZG, Winston LG, Dumyati G, et al. NAP1 strain type predicts outcomes from Clostridium difficile infection. Clin Infect Dis 2014;58: 1394-400.
Leffler DA, Lamont JT. Clostridium difficile infection. N Engl J Med 2015;372: 1539-48.
Baur D, Gladstone BP, Burkert F, Carrara E, Foschi F, Dobele S, et al. Effect of antibiotic stewardship on the incidence of infection and colonisation with antibiotic-resistant bacteria and Clostridium difficile infection: a systematic review and meta-analysis. Lancet Infect Dis 2017;17: 990-1001.
McFarland LV. Probiotics for the primary and secondary prevention of C. difficile infections: A meta-analysis and systematic review. Antibiotics (Basel) 2015;4: 160-78.
Shaughnessy MK, Micielli RL, DePestel DD, Arndt J, Strachan CL, Welch KB, et al. Evaluation of hospital room assignment and acquisition of Clostridium difficile infection. Infect Control Hosp Epidemiol 2011;32: 201-6.
Curry SR, Muto CA, Schlackman JL, Pasculle AW, Shutt KA, Marsh JW, et al. Use of multilocus variable number of tandem repeats analysis genotyping to determine the role of asymptomatic carriers in Clostridium difficile transmission. Clin Infect Dis 2013;57: 1094-102.
Kwok CS, Arthur AK, Anibueze CI, Singh S, Cavallazzi R, Loke YK. Risk of Clostridium difficile infection with acid suppressing drugs and antibiotics: meta-analysis. Am J Gastroenterol 2012;107: 1011-9.
Novack L, Kogan S, Gimpelevich L, Howell M, Borer A, Kelly CP, et al. Acid suppression therapy does not predispose to Clostridium difficile infection: the case of the potential bias. PLoS One 2014;9: e110790.
Cornely OA, Miller MA, Louie TJ, Crook DW, Gorbach SL. Treatment of first recurrence of Clostridium difficile infection: fidaxomicin versus vancomycin. Clin Infect Dis 2012;55 Suppl 2: S154-61.
Reveles KR, Lawson KA, Mortensen EM, Pugh MJV, Koeller JM, Argamany JR, et al. National epidemiology of initial and recurrent Clostridium difficile infection in the Veterans Health Administration from 2003 to 2014. PLoS One 2017;12: e0189227.
Abou Chakra CN, Pepin J, Sirard S, Valiquette L. Risk factors for recurrence, complications and mortality in Clostridium difficile infection: a systematic review. PLoS One 2014;9: e98400.
Sartelli M, Malangoni MA, Abu-Zidan FM, Griffiths EA, Di Bella S, McFarland LV, et al. WSES guidelines for management of Clostridium difficile infection in surgical patients. World J Emerg Surg 2015;10: 38.
Surawicz CM, Brandt LJ, Binion DG, Ananthakrishnan AN, Curry SR, Gilligan PH, et al. Guidelines for diagnosis, treatment, and prevention of Clostridium difficile infections. Am J Gastroenterol 2013;108: 478-98; quiz 499.
Polage CR, Gyorke CE, Kennedy MA, Leslie JL, Chin DL, Wang S, et al. Overdiagnosis of Clostridium difficile infection in the molecular test era. JAMA Intern Med 2015;175: 1792-801.
Cohen SH, Gerding DN, Johnson S, Kelly CP, Loo VG, McDonald LC, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the Society for Healthcare Epidemiology of America (SHEA) and the Infectious Diseases Society of America (IDSA). Infect Control Hosp Epidemiol 2010;31: 431-55.
Felder SI, Larson B, Balzer B, Wachsman A, Haker K, Fleshner P, et al. Fulminant clostridium difficile colitis: comparing computed tomography with histopathology: are they concordant? Am Surg 2014;80: 1064-8.
Hensgens MP, Dekkers OM, Goorhuis A, LeCessie S, Kuijper EJ. Predicting a complicated course of Clostridium difficile infection at the bedside. Clin Microbiol Infect 2014;20: O301-8.
Na X, Martin AJ, Sethi S, Kyne L, Garey KW, Flores SW, et al. A multi-center prospective derivation and validation of a clinical prediction tool for severe Clostridium difficile infection. PLoS One 2015;10: e0123405.
van Beurden YH, Hensgens MPM, Dekkers OM, Le Cessie S, Mulder CJJ, Vandenbroucke-Grauls C. External validation of three prediction tools for patients at risk of a complicated course of Clostridium difficile infection: Disappointing in an outbreak setting. Infect Control Hosp Epidemiol 2017;38: 897-905.
Neal MD, Alverdy JC, Hall DE, Simmons RL, Zuckerbraun BS. Diverting loop ileostomy and colonic lavage: an alternative to total abdominal colectomy for the treatment of severe, complicated Clostridium difficile associated disease. Ann Surg 2011;254: 423-7; discussion 427-9.
Johnson S, Louie TJ, Gerding DN, Cornely OA, Chasan-Taber S, Fitts D, et al. Vancomycin, metronidazole, or tolevamer for Clostridium difficile infection: results from two multinational, randomized, controlled trials. Clin Infect Dis 2014;59: 345-54.
Zar FA, Bakkanagari SR, Moorthi KM, Davis MB. A comparison of vancomycin and metronidazole for the treatment of Clostridium difficile-associated diarrhea, stratified by disease severity. Clin Infect Dis 2007;45: 302-7.
Cornely OA, Crook DW, Esposito R, Poirier A, Somero MS, Weiss K, et al. Fidaxomicin versus vancomycin for infection with Clostridium difficile in Europe, Canada, and the USA: a double-blind, non-inferiority, randomised controlled trial. Lancet Infect Dis 2012;12: 281-9.
Crook DW, Walker AS, Kean Y, Weiss K, Cornely OA, Miller MA, et al. Fidaxomicin versus vancomycin for Clostridium difficile infection: meta-analysis of pivotal randomized controlled trials. Clin Infect Dis 2012;55 Suppl 2: S93-103.
Nathwani D, Cornely OA, Van Engen AK, Odufowora-Sita O, Retsa P, Odeyemi IA. Cost-effectiveness analysis of fidaxomicin versus vancomycin in Clostridium difficile infection. J Antimicrob Chemother 2014;69: 2901-12.
Wilcox MH, Gerding DN, Poxton IR, Kelly C, Nathan R, Birch T, et al. Bezlotoxumab for prevention of recurrent Clostridium difficile infection. N Engl J Med 2017;376: 305-317.
Asempa TE, Nicolau DP. Clostridium difficile infection in the elderly: an update on management. Clin Interv Aging 2017;12: 1799-1809.
van Beurden YH, de Groot PF, van Nood E, Nieuwdorp M, Keller JJ, Goorhuis A. Complications, effectiveness, and long term follow-up of fecal microbiota transfer by nasoduodenal tube for treatment of recurrent Clostridium difficile infection. United European Gastroenterol J 2017;5: 868-879.
Kao D, Roach B, Silva M, Beck P, Rioux K, Kaplan GG, et al. Effect of oral capsule- vs colonoscopy-delivered fecal microbiota transplantation on recurrent Clostridium difficile infection: A randomized clinical trial. JAMA 2017;318: 1985-1993.
Drekonja D, Reich J, Gezahegn S, Greer N, Shaukat A, MacDonald R, et al. Fecal microbiota transplantation for Clostridium difficile infection: A systematic review. Ann Intern Med 2015;162: 630-8.
Fischer M, Sipe B, Cheng YW, Phelps E, Rogers N, Sagi S, et al. Fecal microbiota transplant in severe and severe-complicated Clostridium difficile: A promising treatment approach. Gut Microbes 2017;8: 289-302.
Mamo Y, Woodworth MH, Wang T, Dhere T, Kraft CS. Durability and long-term clinical outcomes of fecal microbiota transplant (FMT) treatment in patients with recurrent Clostridium difficile infection. Clin Infect Dis 2018; 66: 1705-1711.
Woodworth MH, Carpentieri C, Sitchenko KL, Kraft CS. Challenges in fecal donor selection and screening for fecal microbiota transplantation: A review. Gut Microbes 2017;8: 225-237.
Ott SJ, Waetzig GH, Rehman A, Moltzau-Anderson J, Bharti R, Grasis JA, et al. Efficacy of sterile fecal filtrate transfer for treating patients with Clostridium difficile infection. Gastroenterology 2017;152: 799-811 e7.
Zainah H, Hassan M, Shiekh-Sroujieh L, Hassan S, Alangaden G, Ramesh M. Intestinal microbiota transplantation, a simple and effective treatment for severe and refractory Clostridium difficile infection. Dig Dis Sci 2015;60: 181-5.
Kulaylat AS, Kassam Z, Hollenbeak CS, Stewart DB, Sr. A surgical Clostridium-associated risk of death score predicts mortality after colectomy for Clostridium difficile. Dis Colon Rectum 2017;60: 1285-1290.
Stewart DB, Hollenbeak CS, Wilson MZ. Is colectomy for fulminant Clostridium difficile colitis life saving? A systematic review. Colorectal Dis 2013;15: 798-804.
Koss K, Clark MA, Sanders DS, Morton D, Keighley MR, Goh J. The outcome of surgery in fulminant Clostridium difficile colitis. Colorectal Dis 2006;8: 149-54.
Peprah D, Chiu AS, Jean RA, Pei KY. Comparison of outcomes between total abdominal and partial colectomy for the management of severe, complicated Clostridium difficile infection. J Am Coll Surg 2019;228: 925-930.
Ferrada P, Callcut R, Zielinski MD, Bruns B, Yeh DD, Zakrison TL, et al. Loop ileostomy versus total colectomy as surgical treatment for Clostridium difficile-associated disease: An Eastern Association for the Surgery of Trauma multicenter trial. J Trauma Acute Care Surg 2017;83: 36-40.
Hall BR, Leinicke JA, Armijo PR, Smith LM, Langenfeld SJ, Oleynikov D. No survival advantage exists for patients undergoing loop ileostomy for clostridium difficile colitis. Am J Surg 2019;217: 34-39.
Brown CJ, Boutros M, Morris A, Divino CM. CAGS and ACS evidence based reviews in surgery. Is a diverting loop ileostomy and colonic lavage an alternative to colectomy for the treatment of severe Clostridium difficile-associated disease? Can J Surg 2014;57: 214-6.
Fashandi AZ, Ellis SR, Smith PW, Hallowell PT. Overwhelming recurrent Clostridium difficile infection after reversal of diverting loop ileostomy created for prior fulminant C. difficile colitis. Am Surg 2016;82: e194-5.
Kidane B, Lung K, McCreery G, El-Khatib C, Ott MC, Hernandez-Alejandro R, et al. Early rescue from acute severe Clostridium difficile: A novel treatment strategy. Surg Infect (Larchmt) 2018;19: 78-82.
Funding
Dr. Bowman was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through grant #UL1 TR001860, and by the Agency for Healthcare Research and Quality through grant #T32HS022236.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Disclaimer
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or AHRQ.
Disclosure Information
Dr. Utter reports non-financial support from the American Association for the Surgery of Trauma during the conduct of the study. Dr. Bowman does not report any.
Additional information
Learning objectives
1. Understand the transmission of Clostridium difficile in hospital settings
2. Describe the recommended antibiotic treatment of Clostridium difficile infection
3. Discuss the roles of novel therapies such as probiotics, immunotherapy, and fecal microbiota transplant in prevention and treatment of Clostridium difficile infection
4. Describe the surgical options for treatment of Clostridium difficile infection, including the underlying rationale
Questions
1. Which of the following strains of Clostridium difficile is considered the most virulent?
a. NAP1
b. NAP4
c. NAP7
d. NAP11
2. Which of the following is NOT associated with Clostridium difficile infection (CDI)?
a. Age > 65 years
b. Recent antibiotic use
c. Non-steroidal anti-inflammatory drug use
d. Proton pump inhibitor use
3. Which of the following statements is true regarding CDI diagnosis?
a. Nucleic acid amplification testing (NAAT) identifies the amount of TcdA toxin
b. NAAT cannot readily discriminate between those with active infection and those who are colonized
c. Following resolution of symptoms, repeat NAAT should be performed to ensure cure
d. CT scan is helpful in the identification of pseudomembranes
4. Which of the following is the most appropriate treatment for mild-moderate initial CDI?
a. Oral vancomycin
b. Intravenous fidaxomicin
c. Intravenous vancomycin
d. Rectal metronidazole
5. Which of the following is an appropriate treatment for recurrent CDI?
a. 10-day course of intravenous vancomycin if the initial episode was treated with metronidazole
b. 10-day course of oral vancomycin if the initial episode was treated with vancomycin
c. Oral vancomycin taper if the initial episode was treated with vancomycin
d. Oral fidaxomicin if the initial episode was treated with metronidazole
6. Which of the following is a true statement regarding fecal microbiota transplant (FMT)?
a. FMT is associated with a cure of approximately 80%
b. FMT administered via oral capsules had a significantly lower likelihood of cure than FMT via colonoscopy
c. FMT can be administered via suppositories
d. FMT with frozen stool had a significantly lower cure rate than with fresh stool
7. Which of the following is NOT involved as part of diverting ileostomy and colonic irrigation?
a. Diagnostic laparoscopy
b. Intraoperative lavage with polyethylene glycol
c. Postoperative antegrade irrigation with polyethylene glycol
d. Postoperative retrograde (per rectum) vancomycin enemas
8. Which of the following is a true statement regarding surgical outcomes for CDI?
a. Total abdominal colectomy is associated with 20% 30-day mortality
b. The standard NSQIP calculator overestimates CDI-related surgical mortality
c. Diverting ileostomy can be successfully completed in only 50% of cases
d. Ileostomy reversal appears to be more common after diverting ileostomy than after total abdominal colectomy
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Disclosure Information
Dr. Utter reports non-financial support from the American Association for the Surgery of Trauma during the conduct of the study. Dr. Bowman does not report any.
Rights and permissions
About this article
Cite this article
Bowman, J.A., Utter, G.H. Evolving Strategies to Manage Clostridium difficile Colitis. J Gastrointest Surg 24, 484–491 (2020). https://doi.org/10.1007/s11605-019-04478-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04478-5