Abstract
Background
Venous thromboembolism (VTE) is the most common preventable cause of 30-day post-operative mortality, with many events occurring after hospital discharge. High-level evidence supports post-discharge VTE chemoprophylaxis following abdominal/pelvic cancer resection; however, some studies support a more tailored approach. Our objectives were to (1) identify risk factors associated with post-discharge VTE in a large cohort of patients undergoing colorectal cancer resection and (2) develop a post-discharge VTE risk calculator.
Methods
Patients who underwent colorectal cancer resection from 2012 to 2016 were identified from ACS NSQIP colectomy and proctectomy procedure–targeted modules. Multivariable logistic regression was used to identify factors associated with post-discharge VTE. Incorporating pre-operative, intra-operative, and post-operative variables, a post-discharge VTE risk calculator was constructed and validated.
Results
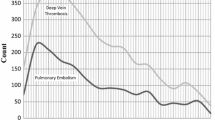
Of 51,139 patients, 387 (0.76%) developed post-discharge VTE. Pre-operative factors associated with post-discharge VTE included BMI (e.g., morbidly obese OR 2.27, 95% CI 1.65–3.12 vs. normal BMI), and thrombocytosis (OR 1.41, 95% CI 1.03–1.92). Intra-operative factors included operative time (4–6 h OR 1.56, 95% CI 1.12–2.17; > 6 h, OR 1.85, 95% CI 1.21–2.84, vs. < 2 h), and type of operation (e.g., open partial colectomy OR 1.67, 95% CI 1.30–2.16 vs. laparoscopic partial colectomy). Post-operative factors included anastomotic leak (OR 2.05, 95% CI 1.31–3.21) and post-operative ileus (OR 1.39, 95% CI 1.07–1.79). Using the risk calculator, the predicted probability of post-discharge VTE ranged from 0.04 to 10.29%. On a 10-fold cross validation, the calculator’s mean C-Statistic was 0.65.
Conclusions
Patient-specific factors are associated with varying rates of post-discharge VTE. We present the first post-discharge VTE risk calculator designed for use at the time of discharge following colorectal cancer resection.

Similar content being viewed by others
References
Lyman GH. Venous thromboembolism in the patient with cancer: focus on burden of disease and benefits of thromboprophylaxis. Cancer. 2011;117(7):1334–1349.
Sanden P, Svensson PJ, Sjalander A. Venous thromboembolism and cancer risk. J Thromb Thrombolysis. 2017;43(1):68–73.
Agnelli G, Bolis G, Capussotti L, et al. A Clinical Outcome-Based Prospetive Study on Venous Thromboembolism After Cancer Surgery The @Ristos Project. Ann Surg. 2006;243(1):89–95.
Serrano PE, Parpia S, Linkins LA, et al. Venous Thromboembolism Events Following Major Pelvic and Abdominal Surgeries for Cancer: A Prospective Cohort Study. Ann Surg Oncol. 2018;25(11):3214–3221.
Moghadamyeghaneh Z, Hanna MH, Carmichael JC, Nguyen NT, Stamos MJ. A nationwide analysis of postoperative deep vein thrombosis and pulmonary embolism in colon and rectal surgery. J Gastrointest Surg. 2014;18(22):2169–2177.
Davenport DL, Vargas HD, Kasten MW, Xenos ES. Timing and perioperative risk factors for in-hospital and post-discharge venous thromboembolism after colorectal cancer resection. Clin Appl Thromb Hemost. 2012;18(6):569–575.
Merkow RP, Bilimoria KY, McCarter MD, et al. Post-discharge venous thromboembolism after cancer surgery: extending the case for etended prohylaxis. Ann Surg. 2011;2554(1):131–137.
Bergqvist D, Agnelli G, Cohen AT, et al. Duration of Prophylaxis Against Venous Thromboembolism with Enoxaparin after Surgery for Cancer. NEJM. 2002;346:975–980.
Rasmussen MS, Jorgensen LN, Wille-Jorgensen P, et al. Prolonged prophylaxis with dalteparin to prevent late thromboembolic complications in patients undergoing major abdominal surgery: a multicenter randomized open-label study. J Thromb Haemost. 2006;4(11):2384–2390.
Kakkar VV, Balibrea JL, Martinez-Gonzalez J, Prandoni P, Group CS. Extended prophylaxis with bemiparin for the prevention of venous thromboembolism after abdominal or pelvic surgery for cancer: the CANBESURE randomized study. J Thromb Haemost. 2010;8(6):1223–1229.
Lyman GH, Khorana AA, Kuderer NM, et al. Venous thromboembolism prophylaxis and treatment in patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31(17):2189–2204.
Gould MK, Garcia DA, Wren SM, et al. Prevention of VTE in nonorthopedic surgical patients: Antithrombotic Therapy and Prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):e227S-e277S.
Fleming F, Gaertner W, Ternent CA, et al. The American Society of Colon and Rectal Surgeons Clinical Practice Guideline for the Prevention of Venous Thromboembolic Disease in Colorectal Surgery. Dis Colon Rectum. 2018;61(1):14–20.
Merkow RP, Bilimoria KY, Sohn MW, et al. Adherence with postdischarge venous thromboemboism chemoprophylaxis recommendations after colorectal cancer surgery among elderly Medicare beneficiaries. Ann Surg. 2014;260(1):103–108.
Sammour T, Chandra R, Moore JW. Extended venous thromboembolism prophylaxis after colorectal cancer surgery: the current state of the evidence. J Thromb Thrombolysis. 2016;42(1):27–32.
Beal EW, Tumin D, Chakedis J, et al. Which Patients Reuire Extended Thromboprophylaxis After Colectomy? Modeling Risk and Assessing Indications for Post-discharge Pharmacoprophylaxis. World J Surg. 2018;42(7):2242–2251.
Ay C, Pabinger I, Cohen AT. Cancer-associated venous thromboembolism: Burden, mechanisms, and management. Thromb Haemost. 2017;117(2):219–230.
Crous-Bou M, Harrington LB, Kabrhel C. Environmental and Genetic Risk Factors Associated with Venous Thromboembolism. Semin Thromb Hemost. 2016;42(8):808–820.
Heit JA. Epidemiology of venous thromboembolism. Nat Rev Cardiol. 2015;12(8):464–474.
Li M, Guo Q, Hu W. Incidence, risk factors, and outcomes of venous thromboembolism after oncologic surgery: A systemic review and meta-analysis. Thromb Res. 2019;173:48–56.
Gonzalez R, Haines K, Nelson LG, Gallagher SF, Murr MM. Predictive factors of thromboembolic events in patients undergoing Roux-en-Y gastric bypass. Surg Obes Relat Dis. 2006;2(1):30–35.
Moghadamyeghaneh Z, Alizadeh RF, Hanna MH, et al. Post-Hospital Discharge Venous Thromboembolism in Colorectal Surgery. World J Surg. 2016;40(5):1255–1263.
Henderson WG, Daley J. Design and statistical methodology of the National Surgical Quality Improvement Program: why is it what it is? Am J Surg. 2009;198(5 Suppl):S19-S27.
Cohen ME, Ko CY, Bilimoria KY, et al. Optimizing ACS NSQIP modeling for evaluation of surgical quality and risk: patient risk adjustment, procedure mix adjustment, shrinkage adjustment, and surgical factors. J Am Coll Surg. 2013;217(2):336–346.
Shiloach M, Frencher SK Jr, Steeger JE, et al. Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg. 2010;210(1):6–16.
Merkow RP, Hall BL, Cohen ME, et al. Relevance of the c-statistic when evaluating risk-adjustment models in surgery. J Am Coll Surg. 2012;214(5):822–830.
Steyerberg EW, Vickers AJ, Cook NR, et al. Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology. 2010;21(1):128–138.
Jung Y, Hu J. A K-fold Averaging Cross-vaidation Procedure. J Nonparametr Stat. 2015;27(2):167–179.
Bilimoria KY, Liu Y, Paruch JL, et al. Development and evaluation of the universal ACS NSQIP surgical risk calculator: a decision aid and informed consent tool for patients and surgeons. J Am Coll Surg. 2013;217(5):833–842.
Cohen ME, Bilimoria KY, Ko CY, Hall BL. Development of an American College of Surgeons National Surgery Quality Improvement Program: morbidity and mortality risk calculator for colorectal surgery. J Am Coll Surg. 2009;208(6):1009–1016.
Hyder JA, Wakeam E, Habermann EB, Hess EP, Cima RR, Nguyen LL. Derivation and validation of a simple calculator to predict home discharge after surgery. J Am Coll Surg. 2014;218(2):226–236.
Mansmann U, Rieger A, Strahwald B, Crispin A. Risk calculators-methods, development, implementtion, and validation. Int J Colorectal Dis. 2016;31(6):1111–1116.
Parikh P, Shiloach M, Cohen ME, et al. Pancreatectomy risk calculator: an ACS-NSQIP resource. HPB (Oxford). 2010;12(7):488–497.
Rasmussen MS, Jorgensen LN, Wille-Jorgensen P. Prolonged thromboprophylaxis with low molecular weight heparin for abdominal or pelvic surgery. Cochrane Database Syst Rev. 2009;21(1):CD004318.
Tevis SE, Kennedy GD. Postoperative Complications: Looking Forward to a Safer Future. Clin Colon Rectal Surg. 2016;29(3):246–252.
Longo WE, Virgo KS, Johnson FE, et al. Risk factors for mobidity and mortality after colectomy for colon cancer. Dis Colon Rectum. 2000;43(1):83–91.
Kronberg U, Kiran RP, Soliman MS, et al. A characterization of factors determining postoperative ileus after laparoscopic colectomy enables the generation of a novel predictive score. Ann Surg. 2011;253(1):78–81.
Funding
This study was supported by the Northwestern Institute for Comparative Effectiveness Research in Oncology (NICER-Onc) of the Robert H. Lurie Comprehensive Cancer Center. ADY is supported by the National Heart, Lung and Blood Institute (K08HL145139), DJB is supported by the Veteran’s Administration Health Services Research and Development Program (I01HX002290), KYB is supported by the Agency for Healthcare Research and Quality (R01HS024516), and RPM is supported by the Agency for Healthcare Research and Quality (K12HS026385) and an Institutional Research Grant from the American Cancer Society (IRG-18-163-24).
Author information
Authors and Affiliations
Contributions
CRS, JYL, ADY, DJB, KYB, and RPM conceived and designed the study.
CRS and JYL collected and analyzed the data.
CRS, JYL, ADY, DJB, KYB, and RPM interpreted the data.
CRS drafted the manuscript.
JYL, ADY, DJB, KYB, and RPM critically revised the manuscript.
CRS, JYL, ADY, DJB, KYB, and RPM have made final approval of this version and agree to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Presentation
Presented at the Society of Surgeons of the Alimentary Tract Small Bowel and Colorectal Plenary Session; San Diego, CA; May 21, 2019.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplemental Table 1
(DOCX 12 kb)
Supplemental Table 2
(DOCX 14 kb)
Rights and permissions
About this article
Cite this article
Schlick, C.J.R., Liu, J.Y., Yang, A.D. et al. Pre-Operative, Intra-Operative, and Post-Operative Factors Associated with Post-Discharge Venous Thromboembolism Following Colorectal Cancer Resection. J Gastrointest Surg 24, 144–154 (2020). https://doi.org/10.1007/s11605-019-04354-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04354-2