Abstract
Background
Extended thromboprophylaxis after abdominal and pelvic cancer surgery to prevent venous thromboembolic events (VTE) is recommended but adherence is sub-optimal. Identifying patients at highest risk for post-discharge events may allow for selective extended thromboprophylaxis. The aim of our study was to identify the different risk factors of venous thromboembolism for in-hospital and post-discharge events.
Methods
The American College of Surgeons-National Surgical Quality Improvement Program (ACS-NSQIP) 2012–2016 database was queried for all patients having colorectal resection. Primary outcome was postoperative VTE occurrence within 30 days. A multinomial logistic regression was performed to identify in-hospital and post-discharge predictors of VTE, adjusting for potential confounders.
Results
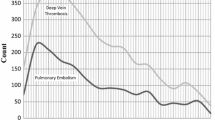
Out of 260,258 patients, 5381 (2.1%) developed VTE. A total of 3442 (1.3%) were diagnosed during the initial hospital stay and 1929 (0.8%) post-discharge. Risk factors for in-hospital and post-discharge VTE were different as patients with an in-hospital event were more likely to be older, male, known for preoperative steroid use, have poor functional status, significant weight loss, preoperative sepsis, prolonged operative time, undergoing an emergency operation. In the post-discharge setting, steroid use, poor functional status, preoperative sepsis, and postoperative complications remained significant. Postoperative complications were the strongest predictor of in-hospital and post-discharge VTE. Patients with inflammatory bowel disease had a higher risk of VTE than patients with malignancy for both in-patient and post-discharge events.
Conclusions
Patients at high-risk for post-discharge events have different characteristics than those who develop VTE in-hospital. Identifying this specific subset of patients at highest risk for post-discharge VTE may allow for the selective use of prolonged thromboprophylaxis.
Similar content being viewed by others
References
Vedovati MC et al (2014) A randomized study on 1-week versus 4-week prophylaxis for venous thromboembolism after laparoscopic surgery for colorectal cancer. Ann Surg 259(4):665–669
Fleming F et al (2018) The American Society of Colon and Rectal Surgeons Clinical Practice Guideline for the Prevention of Venous Thromboembolic Disease in Colorectal Surgery. Dis Colon Rectum 61(1):14–20
McLeod RS et al (2001) Subcutaneous heparin versus low-molecular-weight heparin as thromboprophylaxis in patients undergoing colorectal surgery: results of the canadian colorectal DVT prophylaxis trial: a randomized, double-blind trial. Ann Surg 233(3):438–444
Gross ME et al (2014) The importance of extended postoperative venous thromboembolism prophylaxis in IBD: a National Surgical Quality Improvement Program analysis. Dis Colon Rectum 57(4):482–489
Murthy SK, Nguyen GC (2011) Venous thromboembolism in inflammatory bowel disease: an epidemiological review. Am J Gastroenterol 106(4):713–718
Wallaert JB et al (2012) Venous thromboembolism after surgery for inflammatory bowel disease: are there modifiable risk factors? Data from ACS NSQIP. Dis Colon Rectum 55(11):1138–1144
Gould MK et al., Prevention of VTE in nonorthopedic surgical patients: antithrombotic therapy and prevention of Thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest, 2012. 141(2 Suppl):e227S–e277S
Fleming FJ et al (2010) How much do we need to worry about venous thromboembolism after hospital discharge? A study of colorectal surgery patients using the National Surgical Quality Improvement Program database. Dis Colon Rectum 53(10):1355–1360
Agnelli G et al (2006) A clinical outcome-based prospective study on venous thromboembolism after cancer surgery: the @RISTOS project. Ann Surg 243(1):89–95
Lyman GH et al (2013) Venous thromboembolism prophylaxis and treatment in patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol 31(17):2189–2204
Lyman GH et al (2015) Venous thromboembolism prophylaxis and treatment in patients with cancer: american society of clinical oncology clinical practice guideline update 2014. J Clin Oncol 33(6):654–656
Selby LV et al (2016) Preoperative chemoprophylaxis is safe in major oncology operations and effective at preventing venous thromboembolism. J Am Coll Surg 222(2):129–137
Amin AN et al (2011) Inpatient and outpatient occurrence of deep vein thrombosis and pulmonary embolism and thromboprophylaxis following selected at-risk surgeries. Ann Pharmacother 45(9):1045–1052
Surgeons AC.o. ACS NSQIP Participant Use Data File (2018) April 2, 2018]; https://www.facs.org/quality-programs/acs-nsqip/program-specifics/participant-use
Buchberg B et al (2011) Incidence and risk factors of venous thromboembolism in colorectal surgery: does laparoscopy impart an advantage? Arch Surg 146(6):739–743
Shapiro R, Vogel JD, Kiran RP (2011) Risk of postoperative venous thromboembolism after laparoscopic and open colorectal surgery: an additional benefit of the minimally invasive approach? Dis Colon Rectum 54(12):1496–1502
Nguyen NT et al (2007) Laparoscopic surgery is associated with a lower incidence of venous thromboembolism compared with open surgery. Ann Surg 246(6):1021–1027
Guo Q et al (2017) Perioperative pharmacological thromboprophylaxis in patients with cancer: a systematic review and meta-analysis. Ann Surg 265(6):1087–1093
Vendler MMI et al (2017) Incidence of venous thromboembolic events in enhanced recovery after surgery for colon cancer: a retrospective, population-based cohort study. Colorectal Dis 19(11):O393–O401
El-Dhuwaib Y et al (2017) Venous thromboembolism following colorectal resection. Colorectal Dis 19(4):385–394
McKenna NP et al (2017) Analysis of postoperative venous thromboembolism in patients with chronic ulcerative colitis: is it the disease or the operation? Dis Colon Rectum 60(7):714–722
Ali F et al (2018) Elevated venous thromboembolism risk following colectomy for IBD is equal to those for colorectal cancer for ninety days after surgery. Dis Colon Rectum 61(3):375–381
Tagalakis V et al (2013) Incidence of and mortality from venous thromboembolism in a real-world population: the Q-VTE Study Cohort. Am J Med 126(9):832 e13–21
Gussoni G et al (2013) Three-month mortality rate and clinical predictors in patients with venous thromboembolism and cancer. Findings from the RIETE registry. Thromb Res 131(1):24–30
Alsubaie H et al (2015) Diagnosis of VTE postdischarge for major abdominal and pelvic oncologic surgery: implications for a change in practice. Can J Surg 58(5):305–311
Hanna N et al (2012) Impact of venous thromboembolism on mortality of elderly Medicare patients with stage III colon cancer. Oncologist 17(9):1191–1197
Fanikos J et al (2013) Hospital costs of acute pulmonary embolism. Am J Med 126(2):127–132
Merli G et al., Hospital-based costs associated with venous thromboembolism treatment regimens. J Thromb Haemost, 2008. 6(7):1077–1086
Amin AN, Lin J, Ryan A (2010) Need to improve thromboprophylaxis across the continuum of care for surgical patients. Adv Ther 27(2):81–93
Merkow RP et al (2014) Adherence with postdischarge venous thromboembolism chemoprophylaxis recommendations after colorectal cancer surgery among elderly Medicare beneficiaries. Ann Surg 260(1):103–108
Bradley CT et al (2010) Cost-effectiveness of prolonged thromboprophylaxis after cancer surgery. Ann Surg Oncol 17(1):31–39
Iannuzzi JC et al (2014) Defining high risk: cost-effectiveness of extended-duration thromboprophylaxis following major oncologic abdominal surgery. J Gastrointest Surg 18(1):60–68
Sarasin FP, Bounameaux H (1996) Cost-effectiveness of prophylactic anticoagulation prolonged after hospital discharge following general surgery. Arch Surg 131(7):694–697; discussion 698
Berian JR et al (2018) Association of an enhanced recovery pilot with length of stay in the national surgical quality improvement program. JAMA Surg 153(4):358–365
Kwon S et al (2011) Perioperative pharmacologic prophylaxis for venous thromboembolism in colorectal surgery. J Am Coll Surg 213(5):596–603, 603 e1
Colorectal Writing Group for Surgical (2015) thromboembolic complications and prophylaxis patterns in colorectal surgery. JAMA Surg 150(8):712–720
Alcalay A et al (2006) Venous thromboembolism in patients with colorectal cancer: incidence and effect on survival. J Clin Oncol 24(7):1112–1118
Grainge MJ, West J, Card TR (2010) Venous thromboembolism during active disease and remission in inflammatory bowel disease: a cohort study. Lancet 375(9715):657–663
Funding
None.
Author information
Authors and Affiliations
Contributions
Conception and design of study: Alhassan, Trepanier. Acquisition of data: Alhassan, Chaudhury, Lee. Analysis and/or interpretation of data: Alhassan, Trepanier, Sabapathy, Chaudhury, Liberman, Charlebois, Stein, Lee. Drafting of manuscript: Alhassan, Trepanier. Revising the manuscript for critical content: Sabapathy, Chaudhury, Liberman, Charlebois, Stein, Lee. Approval of the final version to be published: Alhassan, Trepanier, Sabapathy, Chaudhury, Liberman, Charlebois, Stein, Lee.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Liberman is on the medical advisory committee on ERAS for Merck, and on the advisory committee meeting for Novadaq. Dr. Lee is the recipient of an unrestricted educational grant from Johnson & Johnson. Drs. Alhassan, Trepanier, Sabapathy, Chaudhury, Charlebois, and Stein have no conflicts of interest or financial ties to disclose.
Ethical approval
The study protocol was approved by the local institutional review board.
Informed consent
The need for informed consent was waived due to the retrospective nature of the study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Alhassan, N., Trepanier, M., Sabapathy, C. et al. Risk factors for post-discharge venous thromboembolism in patients undergoing colorectal resection: a NSQIP analysis. Tech Coloproctol 22, 955–964 (2018). https://doi.org/10.1007/s10151-018-1909-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10151-018-1909-8