Abstract
Background
Studies addressing both lymphovascular invasion (LVI) and perineural invasion (PNI) in patients with esophageal squamous cell carcinoma (ESCC) treated with or without neoadjuvant therapy are limited. We aimed to analyze the incidence and prognostic significance of LVI and PNI in patients with thoracic ESCC.
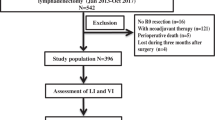
Methods
This retrospective study included 520 patients with ESCC: 174 patients after neoadjuvant treatment followed by surgery and 346 after primary esophagectomy, from two medical centers. The relationships between LVI, PNI, and other histological factors were evaluated. The Cox regression model was used for survival analysis.
Results
Positive LVI and PNI were noted in 35.6% and 22.4% of patients with residual primary tumor after neoadjuvant treatment and in 39.6% and 24.0% of patients who underwent primary esophagectomy, respectively. In patients with neoadjuvant treatments, the 5-year overall survival rates were 12.7% and 28.3% in patients with positive LVI and negative LVI, respectively (p = 0.001). The 5-year overall survival rates were 6.4% and 29.9% in patients with positive PNI and negative PNI, respectively (p < 0.001). In patients who did not receive neoadjuvant treatment, the 5-year overall survival rates were 28.2% and 61.1% in patients with positive LVI and negative LVI, respectively (p < 0.001). The 5-year overall survival rates were 30.2% and 52.5% in patients with positive PNI and negative PNI (p < 0.001). In subgroup analysis, the presence of PNI was an independent prognostic factor in patients with neoadjuvant treatments, whereas the presence of LVI had more significant prognostic impact in patients with node-negative ESCC after primary esophagectomy.
Conclusions
Both LVI and PNI statuses are significant prognostic factors for patients with ESCC. However, the prognostic impact of LVI was majorly in the subgroup of node-negative patients who received primary esophagectomy.


Similar content being viewed by others
References
Lagarde SM, Reitsma JB, Ten Kate FJW, Busch ORC, Obertop H, Zwinderman AH, et al. Predicting individual survival after potentially curative esophagectomy for adenocarcinoma of the esophagus or gastroesophageal junction. Ann Surg 2008;248:1006–13.
Hsu PK, Wang BY, Huang CS, Wu YC, Hsu WH. Prognostic factors for post-recurrence survival in esophageal squamous cell carcinoma patients with recurrence after resection. J Gastrointest Surg 2011;15:558–65.
Van Hagen P, Hulshof MC, van Lanschot JJ, Steyerberg EW, van Berge Henegouwen MI, Wijnhoven BP, et al. Preoperative chemoradiotherapy for esophageal or junctional Cancer. N Engl J Med 2012;366:2074–84.
Mariette C, Dahan L, Mornex F, Maillard E, Thomas PA, Meunier B et al. Surgery alone versus chemoradiotherapy followed by surgery for stage I and II esophageal cancer: final analysis of randomized controlled phase III trial FFCD 9901. J Clin Oncol 2014;32:2416–22.
Hsu WH, Hsu PK, Hsieh CC, Huang CS, Wu YC. The metastatic lymph node number and ratio are independent prognostic factors in esophageal cancer. J Gastrointest Surg 2009;13:1913–20.
Peyre CG, Hagen JA, DeMeester SR, Altorki NK, Ancona E, Griffin SM, et al. The number of lymph nodes removed predicts survival in esophageal cancer: an international study on the impact of extent of surgical resection. Ann Surg 2008;248: 549–56.
Hsu PK, Chien LI, Wang LC, Chou TY. Lymphovascular invasion and extracapsular invasion are risk factors for distant recurrence after preoperative chemoradiotherapy and esophagectomy in patients with esophageal squamous cell carcinoma. Eur J Cardiothorac Surg 2017;51:1188–94.
Hogan J, Chang KH, Duff G, Samaha G, Kelly N, Burton M, et al. Lymphovascular invasion: a comprehensive appraisal in colon and rectal adenocarcinoma. Dis Colon Rectum 2015;58:547–55.
Lee AH, Pinder SE, Macmillan RD, Mitchell M, Ellis IO, Elston CW, et al. Prognostic value of lymphovascular invasion in women with lymph node negative invasive breast carcinoma. Eur J Cancer 2006;42:357–62.
Yanagawa N, Shiono S, Abiko M, Ogata SY, Sato T, Tamura G. Prognostic impact and initial recurrence site of lymphovascular and visceral pleural invasion in surgically resected stage I non-small-cell lung carcinoma. Eur J Cardiothorac Surg 2013;44:e200–6.
Chen WH, Huang YL, Chao YK, Yeh CJ, Chang HK, Tseng CK, et al. Prognostic significance of lymphovascular invasion in patients with esophageal squamous cell carcinoma treated with neoadjuvant chemoradiotherapy. Ann Surg Oncol 2015;22:338–43.
Lagarde SM, Phillips AW, Navidi M, Disep B, Immanuel A, Griffin SM. The presence of lymphovascular and perineural infiltration after neoadjuvant therapy and oesophagectomy identifies patients at high risk for recurrence. Br J Cancer 2015;113:1427–33.
Huang Q, Luo K, Chen C, Wang G, Jin J, Kong M, et al. Identification and validation of lymphovascular invasion as a prognostic and staging factor in node-negative esophageal squamous cell carcinoma. J Thorac Oncol 2016;11:583–92.
Imamura Y, Watanabe M, Nagai Y, Baba Y, Hirashima K, Karashima R, et al. Lymphatic vessel invasion detected by the D2-40 monoclonal antibody is an independent prognostic factor in node-negative esophageal squamous cell carcinoma. J Surg Oncol 2012;105:277–83.
Cen P, Hofstetter WL, Correa AM, Wu TT, Lee JH, Ross WA, et al. Lymphovascular invasion as a tool to further subclassify T1b esophageal adenocarcinoma. Cancer. 2008;112:1020–7.
Wang S, Chen X, Fan J, Lu L. Prognostic significance of lymphovascular invasion for thoracic esophageal squamous cell carcinoma. Ann Surg Oncol 2016;23:4101–9.
Faiz Z, Huijgen LJW, Alqethami HJ, Burgerhof JGM, Kats-Ugurlu G, Plukker JTM. Prevalence and prognostic significance of extramural venous invasion in patients with locally advanced esophageal cancer. Ann Surg Oncol 2018;25:1588–97.
Brucher BL, Stein HJ, Werner M, Siewert JR. Lymphatic vessel invasion is an independent prognostic factor in patients with a primary resected tumor with esophageal squamous cell carcinoma. Cancer 2001;92:2228–33.
Von Rahden BH, Stein HJ, Feith M, Becker K, Siewert JR. Lymphatic vessel invasion as a prognostic factor in patients with primary resected adenocarcinomas of the esophagogastric junction. J Clin Oncol 2005;23:874–9.
Liebig C, Ayala G, Wilks JA, Berger DH, Albo D. Perineural invasion in cancer: a review of the literature. Cancer 2009;115:3379–91.
Meng Y, Liao YB, Xu P, Wei WR, Wang J. Perineural invasion is an independent predictor of biochemical recurrence of prostate cancer after local treatment: a meta-analysis. Int J Clin Exp Med 2015;8:13267–74.
Murakami Y, Uemura K, Sudo T, Hashimoto Y, Kondo N, Nakagawa N, et al. Perineural invasion in extrahepatic cholangiocarcinoma: prognostic impact and treatment strategies. J Gastrointest Surg 2013;17:1429–39.
Aivazian K, Ebrahimi A, Low TH, Gao K, Clifford A, Shannon K, et al. Perineural invasion in oral squamous cell carcinoma: quantitative subcategorisation of perineural invasion and prognostication. J Surg Oncol 2015;111:352–8.
Deng J, You Q, Gao Y, Yu Q, Zhao P, Zheng Y, et al. Prognostic value of perineural invasion in gastric cancer: a systematic review and meta-analysis. PLoS One 2014;9:e88907.
Ning ZH, Zhao W, Li XD, Chen LJ, Xu B, Gu WD, et al. The status of perineural invasion predicts the outcomes of postoperative radiotherapy in locally advanced esophageal squamous cell carcinoma. Int J Clin Exp Pathol 2015;8:6881–90.
Xu G, Feng F, Liu Z, Liu S, Zheng G, Xiao S, et al. Prognosis and progression of ESCC patients with perineural invasion. Sci Rep 2017;7:43828.
Tsai CY, Yeh CJ, Chao YK, Chang HK, Tseng CK, Liu YH. Perineural invasion through the sheath in posttherapy esophagectomy specimens predicts poor survival in patients with esophageal squamous cell carcinoma. Eur J Surg Oncol 2017;43:1970–6.
Chen JW, Xie JD, Ling YH, Li P, Yan SM, Xi SY, et al. The prognostic effect of perineural invasion in esophageal squamous cell carcinoma. BMC Cancer 2014;14:313.
Acknowledgments
We would like to especially thank all the members in the Taipei Veterans General Hospital Esophageal Cancer Panel and Taichung Veterans General Hospital Esophageal Cancer Panel for assisting with patient care and data collection.
Author information
Authors and Affiliations
Contributions
Hsu CP: conception and design of the work, interpretation of data, and final approval.
Chung CY: substantial contributions to data acquisition and final approval.
Hsu PK: design of the work data analysis and drafting the work.
Chien LI: substantial contributions to data acquisition (Taipei VGH).
Lin CH: substantial contributions to data acquisition (Taichung VGH).
Yeh YC: substantial contributions to data interpretation and analysis.
Hsu HS: conception of the work and final approval.
Wu YC: conception of the work and final approval.
Corresponding author
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hsu, CP., Chuang, CY., Hsu, PK. et al. Lymphovascular Invasion as the Major Prognostic Factor in Node-Negative Esophageal Cancer After Primary Esophagectomy. J Gastrointest Surg 24, 1459–1468 (2020). https://doi.org/10.1007/s11605-019-04310-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04310-0