Abstract
Purpose
To compare the incidences of positive hemodynamic response (HR > 100 beats min−1 or SBP > 160 mmHg) during abdominal exploration and moderate pain after surgery, when using dexmedetomidine infusion and rectus sheath block.
Methods
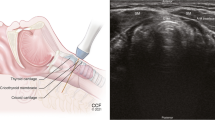
One hundred patients undergoing open gastrectomy were randomized to receive rectus sheath block with ropivacaine (Group B, n = 25), initial loading dose of 0.6 μg kg−1 dexmedetomidine, followed by a continuous infusion of 0.2 μg kg−1 h−1 throughout surgery (Group D, n = 25), both rectus sheath block and dexmedetomidine (Group BD, n = 25), or neither rectus sheath block nor dexmedetomidine (Group C, n = 25). General anesthesia techniques were standardized. HR, SBP, and positive hemodynamic response at peritoneum incision (TPI), 5 min (TAE-5), 10 min (TAE-10), and 15 min (TAE-15) after the start of abdominal exploration, and incidences of moderate postoperative pain were recorded.
Results
Positive hemodynamic responses during abdominal exploration were more common in Groups B (82%) and C (74%) than in Groups D (14%) and BD (9%) (all P = 0.000). HR and SBP were lower in Groups D and BD, compared with those in Groups C and B (all P < 0.05). Compared with TPI, HR and SBP increased significantly in Groups B and C during abdominal exploration (all P < 0.05), but not in Group BD (except HR at TAE-15). The incidences of moderate pain in Groups B and BD were noticeably lower than in Groups C and D at 1 h, 2 h, and 6 h after surgery (all P < 0.0083).
Conclusion
Dexmedetomidine infusion combined with rectus sheath block provided more hemodynamic stability during abdominal exploration and better analgesia after surgery.



Similar content being viewed by others
References
Wu Y, Liu F, Tang H, Wang Q, Chen L, Wu H, Zhang X, Miao J, Zhu M, Hu C, Goldsworthy M, You J, Xu X. The analgesic efficacy of subcostal transversus abdominis plane block compared with thoracic epidural analgesia and intravenous opioid analgesia after radical gastrectomy. Anesth Analg. 2013;117: 507–13.
Block BM, Liu SS, Rowlingson AJ, Cowan AR, Cowan JA, Jr., Wu CL. Efficacy of postoperative epidural analgesia: a meta-analysis. JAMA. 2003;290: 2455–63.
Wilkinson KM, Krige A, Brearley SG, Lane S, Scott M, Gordon AC, Carlson GL. Thoracic Epidural analgesia versus Rectus Sheath Catheters for open midline incisions in major abdominal surgery within an enhanced recovery programme (TERSC): study protocol for a randomised controlled trial. Trials. 2014;15: 400.
Kang XH, Bao FP, Xiong XX, Li M, Jin TT, Shao J, Zhu SM. Major complications of epidural anesthesia: a prospective study of 5083 cases at a single hospital. Acta Anaesthesiol Scand. 2014;58: 858–66.
Rawal N. Epidural technique for postoperative pain: gold standard no more? Reg Anesth Pain Med. 2012;37: 310–7.
Ganapathy S, Sondekoppam RV, Terlecki M, Brookes J, Das Adhikary S, Subramanian L. Comparison of efficacy and safety of lateral-to-medial continuous transversus abdominis plane block with thoracic epidural analgesia in patients undergoing abdominal surgery: A randomised, open-label feasibility study. Eur J Anaesthesiol. 2015;32: 797–804.
Aho M, Scheinin M, Lehtinen AM, Erkola O, Vuorinen J, Korttila K. Intramuscularly administered dexmedetomidine attenuates hemodynamic and stress hormone responses to gynecologic laparoscopy. Anesth Analg. 1992;75: 932–9.
Willschke H, Bosenberg A, Marhofer P, Johnston S, Kettner SC, Wanzel O, Kapral S. Ultrasonography-guided rectus sheath block in paediatric anaesthesia--a new approach to an old technique. Br J Anaesth. 2006;97: 244–9.
Lui MW, Li TKT, Lui F, Ong CYT. A randomised, controlled trial of rectus sheath bupivacaine and intrathecal bupivacaine, without or with intrathecal morphine, vs. intrathecal bupivacaine and morphine after caesarean section. Anaesthesia. 2017;72: 1225–9.
Bakshi SG, Mapari A, Shylasree TS. REctus Sheath block for postoperative analgesia in gynecological ONcology Surgery (RESONS): a randomized-controlled trial. Can J Anaesth. 2016;63: 1335–44.
Shido A, Imamachi N, Doi K, Sakura S, Saito Y. Continuous local anesthetic infusion through ultrasound-guided rectus sheath catheters. Can J Anaesth. 2010;57: 1046–7.
Meng L, Yu W, Wang T, Zhang L, Heerdt PM, Gelb AW. Blood Pressure Targets in Perioperative Care. Hypertension. 2018;72: 806–17.
Reich DL, Bennett-Guerrero E, Bodian CA, Hossain S, Winfree W, Krol M. Intraoperative tachycardia and hypertension are independently associated with adverse outcome in noncardiac surgery of long duration. Anesth Analg. 2002;95: 273–7, table of contents.
Abbott TEF, Pearse RM, Archbold RA, Ahmad T, Niebrzegowska E, Wragg A, Rodseth RN, Devereaux PJ, Ackland GL. A Prospective International Multicentre Cohort Study of Intraoperative Heart Rate and Systolic Blood Pressure and Myocardial Injury After Noncardiac Surgery: Results of the VISION Study. Anesth Analg. 2018;126: 1936–45.
Breschan C, Jost R, Stettner H, Feigl G, Semmelrock S, Graf G, Likar R. Ultrasound-guided rectus sheath block for pyloromyotomy in infants: a retrospective analysis of a case series. Paediatr Anaesth. 2013;23: 1199–204.
Li Y, Wang B, Zhang LL, He SF, Hu XW, Wong GT, Zhang Y. Dexmedetomidine Combined with General Anesthesia Provides Similar Intraoperative Stress Response Reduction When Compared with a Combined General and Epidural Anesthetic Technique. Anesth Analg. 2016;122: 1202–10.
Menda F, Koner O, Sayin M, Ture H, Imer P, Aykac B. Dexmedetomidine as an adjunct to anesthetic induction to attenuate hemodynamic response to endotracheal intubation in patients undergoing fast-track CABG. Ann Card Anaesth. 2010;13: 16–21.
Kim SY, Kim JM, Lee JH, Song BM, Koo BN. Efficacy of intraoperative dexmedetomidine infusion on emergence agitation and quality of recovery after nasal surgery. Br J Anaesth. 2013;111: 222–8.
Li YH, Wang YQ, Zhang YJ, Zheng DY, Hu L, Tian ML. Influence of Dexmedetomidine on the Tourniquet Related Responses in Hypertension Patients Receiving Unilateral Knee Arthroplasty under General Anesthesia. J Arthroplasty. 2015;30: 1359–63.
Hamasaki J, Tsuneyoshi I, Katai R, Hidaka T, Boyle WA, Kanmura Y. Dual alpha(2)-adrenergic agonist and alpha(1)-adrenergic antagonist actions of dexmedetomidine on human isolated endothelium-denuded gastroepiploic arteries. Anesth Analg. 2002;94: 1434–40, table of contents.
Talke P, Lobo E, Brown R. Systemically administered alpha2-agonist-induced peripheral vasoconstriction in humans. Anesthesiology. 2003;99: 65–70.
Le Guen M, Liu N, Tounou F, Auge M, Tuil O, Chazot T, Dardelle D, Laloe PA, Bonnet F, Sessler DI, Fischler M. Dexmedetomidine reduces propofol and remifentanil requirements during bispectral index-guided closed-loop anesthesia: a double-blind, placebo-controlled trial. Anesth Analg. 2014;118: 946–55.
Yassin HM, Abd Elmoneim AT, El Moutaz H. The Analgesic Efficiency of Ultrasound-Guided Rectus Sheath Analgesia Compared with Low Thoracic Epidural Analgesia After Elective Abdominal Surgery with a Midline Incision: A Prospective Randomized Controlled Trial. Anesth Pain Med. 2017;7: e14244.
Gurnaney HG, Maxwell LG, Kraemer FW, Goebel T, Nance ML, Ganesh A. Prospective randomized observer-blinded study comparing the analgesic efficacy of ultrasound-guided rectus sheath block and local anaesthetic infiltration for umbilical hernia repair. Br J Anaesth. 2011;107: 790–5.
Ding W, Li W, Zeng X, Li J, Jiang J, Guo C. Effect of Adding Dexmedetomidine to Ropivacaine on Ultrasound-Guided Dual Transversus Abdominis Plane Block after Gastrectomy. J Gastrointest Surg. 2017;21: 936–46.
Murouchi T, Iwasaki S, Yamakage M. Chronological Changes in Ropivacaine Concentration and Analgesic Effects Between Transversus Abdominis Plane Block and Rectus Sheath Block. Reg Anesth Pain Med. 2015;40: 568–71.
Rahiri J, Tuhoe J, Svirskis D, Lightfoot NJ, Lirk PB, Hill AG. Systematic review of the systemic concentrations of local anaesthetic after transversus abdominis plane block and rectus sheath block. Br J Anaesth. 2017;118: 517–26.
Phua DS, Phoo JW, Koay CK. The ultrasound-guided rectus sheath block as an anaesthetic in adult paraumbilical hernia repair. Anaesth Intensive Care. 2009;37: 499–500.
Vorobeichik L, Brull R, Abdallah FW. Evidence basis for using perineural dexmedetomidine to enhance the quality of brachial plexus nerve blocks: a systematic review and meta-analysis of randomized controlled trials. Br J Anaesth. 2017;118: 167–81.
Kim NY, Kwon TD, Bai SJ, Noh SH, Hong JH, Lee H, Lee KY. Effects of dexmedetomidine in combination with fentanyl-based intravenous patient-controlled analgesia on pain attenuation after open gastrectomy in comparison with conventional thoracic epidural and fentanyl-based intravenous patient-controlled analgesia. Int J Med Sci. 2017;14: 951–60.
Acknowledgements
We are thankful to Dr.Fengfeng Mo and Dr. Xiaofei Ye for their help in statistical work.
Funding
The authors received financial support from the National Science Foundation of China (81671304, 81873945, 81870864, 81571935), the Pujiang Talent Program of Shanghai (16PJD002), and the Outstanding Technical Leader Project of Shanghai Science and Technology Commission (17XD1424300).
Author information
Authors and Affiliations
Contributions
All authors contributed to the concept and design of the trial, reviewed the analyses, and participated in the preparation of the submitted manuscript. Yonghua Li, Xin Jiang, and Jiafeng Wang conducted or supervised patient recruitment and data collection. Liye Yang performed nerve block and anesthesia. Wei Chen conducted the statistical analysis with the collaboration of Xuerong Miao and Hongbin Yuan. Dr. Xuerong Miao and Hongbin Yuan had full access to the study data and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding authors
Ethics declarations
This study was approved by the Chinese Ethics Committee of Registering Clinical Trials (ethical number ChiECRCT-20170107) and was registered at http://www.chictr.org.cn (registration number ChiCTR1800014437). Written informed consents were obtained from all patients.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Li, Y., Jiang, X., Wang, J. et al. Intravenous Dexmedetomidine Combined with Ultrasound-Guided Rectus Sheath Block for Open Gastrectomy: a Prospective Randomized Trial. J Gastrointest Surg 24, 1290–1297 (2020). https://doi.org/10.1007/s11605-019-04249-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04249-2