Abstract
Objective
This study assessed predictors of survival after repeat hepatectomy and the feasibility of a repeat hepatectomy after a major hepatectomy in the patients with colorectal liver metastases (CLM).
Background
More than half of all patients who receive a curative initial hepatectomy for CLM develop hepatic recurrence, and aggressive indications for a repeat hepatectomy can improve the outcome in selected patients. However, the feasibility of repeat hepatectomy after major hepatectomy remains uncertain, and optimal selection criteria for repeat hepatectomy have not yet been established.
Methods
Data were collected retrospectively on 296 CLM patients who underwent an initial curative hepatectomy between 2007 and 2017 at our institution. The postoperative outcomes of patients undergoing a repeat hepatectomy after major hepatectomy were assessed, and independent predictors of survival were investigated.
Results
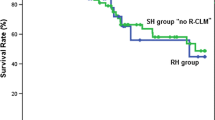
After a median follow-up period of 32 months, 247 patients (83%) developed disease recurrence and 122 patients (49%) underwent repeat hepatectomy. The 5-year overall survival (OS) was significantly higher in patients who underwent a repeat hepatectomy than in those who did not receive repeat hepatectomy (51% vs. 19%, respectively; P < 0.001). In a multivariate analysis, an extrahepatic lesion at the time of the repeat hepatectomy (HR, 2.49; P = 0.001) and 5 or more liver tumors at the time of recurrence (HR, 1.88; P = 0.04) remained as independent factors negatively affecting OS after repeat hepatectomy. The type of operative procedure and the intraoperative and postoperative factors at the time of the initial hepatectomy did not have any significant influence on the OS after repeat hepatectomy. No significant difference in OS was found between patients who received repeat hepatectomy after major hepatectomy (n = 43) and those after non-major hepatectomy (n = 79).
Conclusions
The operative procedure and the liver tumor status at the time of the initial hepatectomy have little impact on the indications for a repeat hepatectomy for recurrent CLM. Repeat hepatectomy is feasible even if major hepatectomy was initially performed.



Similar content being viewed by others
References
Hepatitis B vaccine in the expanded programme of immunisation: The Gambian experience. The Gambia Hepatitis Study Group. Lancet. 1989;1(8646):1057–9.
Rees M, Tekkis PP, Welsh FK, O'Rourke T, John TG. Evaluation of long-term survival after hepatic resection for metastatic colorectal cancer: a multifactorial model of 929 patients. Ann Surg. 2008;247(1):125–35.
House MG, Ito H, Gonen M, Fong Y, Allen PJ, DeMatteo RP et al. Survival after hepatic resection for metastatic colorectal cancer: trends in outcomes for 1,600 patients during two decades at a single institution. J Am Coll Surg. 2010;210(5):744–52, 52-5.
de Haas RJ, Wicherts DA, Andreani P, Pascal G, Saliba F, Ichai P et al. Impact of expanding criteria for resectability of colorectal metastases on short- and long-term outcomes after hepatic resection. Ann Surg. 2011;253(6):1069–79.
Minagawa M, Makuuchi M, Torzilli G, Takayama T, Kawasaki S, Kosuge T et al. Extension of the frontiers of surgical indications in the treatment of liver metastases from colorectal cancer: long-term results. Ann Surg. 2000;231(4):487–99.
Jones RP, Jackson R, Dunne DF, Malik HZ, Fenwick SW, Poston GJ et al. Systematic review and meta-analysis of follow-up after hepatectomy for colorectal liver metastases. Br J Surg. 2012;99(4):477–86.
Mise Y, Aloia TA, Brudvik KW, Schwarz L, Vauthey JN, Conrad C. Parenchymal-sparing Hepatectomy in Colorectal Liver Metastasis Improves Salvageability and Survival. Ann Surg. 2016;263(1):146–52.
Matsumura M, Mise Y, Saiura A, Inoue Y, Ishizawa T, Ichida H et al. Parenchymal-Sparing Hepatectomy Does Not Increase Intrahepatic Recurrence in Patients with Advanced Colorectal Liver Metastases. Ann Surg Oncol. 2016;23(11):3718–26.
Takamoto T, Hashimoto T, Ogata S, Inoue K, Maruyama Y, Miyazaki A et al. Planning of anatomical liver segmentectomy and subsegmentectomy with 3-dimensional simulation software. Am J Surg. 2013;206(4):530–8.
Makuuchi M, Kosuge T, Takayama T, Yamazaki S, Kakazu T, Miyagawa S et al. Surgery for small liver cancers. Semin Surg Oncol. 1993;9(4):298–304.
Kubota K, Makuuchi M, Kusaka K, Kobayashi T, Miki K, Hasegawa K et al. Measurement of liver volume and hepatic functional reserve as a guide to decision-making in resectional surgery for hepatic tumors. Hepatology. 1997;26(5):1176–81.
Hamady ZZ, Lodge JP, Welsh FK, Toogood GJ, White A, John T et al. One-millimeter cancer-free margin is curative for colorectal liver metastases: a propensity score case-match approach. Ann Surg. 2014;259(3):543–8.
Takamoto T, Sugawara Y, Hashimoto T, Shimada K, Inoue K, Maruyama Y et al. Two-dimensional assessment of submillimeter cancer-free margin area in colorectal liver metastases. Medicine (Baltimore). 2016;95(27):e4080.
Takamoto T, Hashimoto T, Inoue K, Nagashima D, Maruyama Y, Mitsuka Y et al. Applicability of enhanced recovery program for advanced liver surgery. World J Surg. 2014;38(10):2676–82.
Clavien PA, Petrowsky H, DeOliveira ML, Graf R. Strategies for safer liver surgery and partial liver transplantation. N Engl J Med. 2007;356(15):1545–59.
Rahbari NN, Garden OJ, Padbury R, Brooke-Smith M, Crawford M, Adam R et al. Posthepatectomy liver failure: a definition and grading by the International Study Group of Liver Surgery (ISGLS). Surgery. 2011;149(5):713–24.
Oba M, Hasegawa K, Matsuyama Y, Shindoh J, Mise Y, Aoki T et al. Discrepancy between recurrence-free survival and overall survival in patients with resectable colorectal liver metastases: a potential surrogate endpoint for time to surgical failure. Ann Surg Oncol. 2014;21(6):1817–24.
Muratore A, Polastri R, Bouzari H, Vergara V, Ferrero A, Capussotti L. Repeat hepatectomy for colorectal liver metastases: A worthwhile operation? J Surg Oncol. 2001;76(2):127–32.
Jones NB, McNally ME, Malhotra L, Abdel-Misih S, Martin EW, Bloomston M et al. Repeat hepatectomy for metastatic colorectal cancer is safe but marginally effective. Ann Surg Oncol. 2012;19(7):2224–9.
Kulik U, Bektas H, Klempnauer J, Lehner F. Repeat liver resection for colorectal metastases. Br J Surg. 2013;100(7):926–32.
Ali MA, Di Sandro S, Lauterio A, Concone G, Mangoni I, Ferla F et al. Repeat Hepatectomy for Recurrent Colorectal Liver Metastases: Is it Worth the Challenge? J Gastrointest Surg. 2015;19(12):2192–8.
Shaw IM, Rees M, Welsh FK, Bygrave S, John TG. Repeat hepatic resection for recurrent colorectal liver metastases is associated with favourable long-term survival. Br J Surg. 2006;93(4):457–64.
Saiura A, Yamamoto J, Koga R, Takahashi Y, Takahashi M, Inoue Y et al. Favorable outcome after repeat resection for colorectal liver metastases. Ann Surg Oncol. 2014;21(13):4293–9.
Hellman S, Weichselbaum RR. Oligometastases. J Clin Oncol. 1995;13(1):8–10.
Reyes DK, Pienta KJ. The biology and treatment of oligometastatic cancer. Oncotarget. 2015;6(11):8491–524.
Fong Y, Cohen AM, Fortner JG, Enker WE, Turnbull AD, Coit DG et al. Liver resection for colorectal metastases. J Clin Oncol. 1997;15(3):938–46.
Adam R, Wicherts DA, de Haas RJ, Ciacio O, Levi F, Paule B et al. Patients with initially unresectable colorectal liver metastases: is there a possibility of cure? J Clin Oncol. 2009;27(11):1829–35.
Folprecht G, Gruenberger T, Bechstein WO, Raab HR, Lordick F, Hartmann JT et al. Tumour response and secondary resectability of colorectal liver metastases following neoadjuvant chemotherapy with cetuximab: the CELIM randomised phase 2 trial. Lancet Oncol. 2010;11(1):38–47.
Venook AP, Niedzwiecki D, Lenz HJ, Innocenti F, Fruth B, Meyerhardt JA et al. Effect of First-Line Chemotherapy Combined With Cetuximab or Bevacizumab on Overall Survival in Patients With KRAS Wild-Type Advanced or Metastatic Colorectal Cancer: A Randomized Clinical Trial. Jama. 2017;317(23):2392–401.
Grothey A, Sargent D, Goldberg RM, Schmoll HJ. Survival of patients with advanced colorectal cancer improves with the availability of fluorouracil-leucovorin, irinotecan, and oxaliplatin in the course of treatment. J Clin Oncol. 2004;22(7):1209–14.
Normanno N, Tejpar S, Morgillo F, De Luca A, Van Cutsem E, Ciardiello F. Implications for KRAS status and EGFR-targeted therapies in metastatic CRC. Nature reviews Clinical oncology. 2009;6(9):519–27.
Farina-Sarasqueta A, van Lijnschoten G, Moerland E, Creemers GJ, Lemmens VE, Rutten HJ et al. The BRAF V600E mutation is an independent prognostic factor for survival in stage II and stage III colon cancer patients. Ann Oncol. 2010;21(12):2396–402.
Tol J, Nagtegaal ID, Punt CJ. BRAF mutation in metastatic colorectal cancer. N Engl J Med. 2009;361(1):98–9.
Author information
Authors and Affiliations
Contributions
Takeshi Takamoto performed data analysis and wrote the manuscript with support from Takuya Hashimoto, Akinori Miyata, Kei Shimada, Yoshikazu Maruyama, and Masatoshi Makuuchi. All authors contributed to data collection, discussed the results, and contributed to the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Takamoto, T., Hashimoto, T., Miyata, A. et al. Repeat Hepatectomy After Major Hepatectomy for Colorectal Liver Metastases. J Gastrointest Surg 24, 380–387 (2020). https://doi.org/10.1007/s11605-019-04154-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-019-04154-8