Abstract
Background
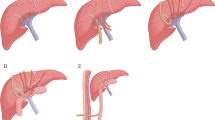
Roux-en-Y hepaticojejunostomy (HJ) currently represents the gold standard after resection of the biliary confluence. This non-physiological reconstruction poses several problems such as repeated cholangitis or stricture without conventional endoscopic access. Our aim was to describe and to report both feasibility and results of duct-to-duct anastomosis with removable internal biliary drain (RIBS) as an alternative technique to the HJ after resection of the biliary confluence in patients undergoing major liver resection.
Methods
Between January 2014 and January 2018, all patients who underwent a major hepatectomy associated with resection of the biliary confluence and reconstruction by duct-to-duct biliary anastomosis with RIBS were retrospectively included. Patient demographics, tumor characteristics, pre- and postoperative outcomes, early and late biliary complications, endoscopic complications, and clinical follow-up were collected.
Results
Twelve patients were included. The operative time was 326 ± 45 min (range 240–380 min). There was no postoperative mortality. Only one patient experienced biliary anastomotic leakage treated exclusively by radiological and endoscopic drainage. Four patients had an asymptomatic stricture of the biliary anastomosis detected by endoscopic retrograde cholangiopancreatography (ERCP) during the extraction of the RIBS requiring iterative dilatation and replacement of the RIBS. Among 21 performed ERCP, no complications such as failure of RIBS extraction, duodenal perforation, bleeding after sphincterotomy, cholangitis, or pancreatitis were observed. After a mean and a median follow-up of respectively 15.0 ± 14.9 and 8.7 months (range 2.0–46.1 months), no cholangitis occurred.
Conclusion
Duct-to-duct biliary anastomosis with RIBS insertion after resection of the biliary confluence represents a feasible and safe alternative to the HJ.





Similar content being viewed by others
References
Memeo R, de Blasi V, Adam R, Goéré D, Piardi T, Lermite E, Turrini O, Navarro F, de’Angelis, N, Cunha AS, Pessaux P, French Colorectal Liver Metastases Working Group, Association Française de Chirurgie (AFC). Margin Status is Still an Important Prognostic Factor in Hepatectomies for Colorectal Liver Metastases: A Propensity Score Matching Analysis. World J Surg 2018;42:892–901
Tang H, Lu W, Li B, Meng X, Dong J. Influence of surgical margins on overall survival after resection of intrahepatic cholangiocarcinoma: A meta-analysis. Medicine (Baltimore) 2016;95:e4621.
Chang YJ, Chung KP, Chang YJ, Chen LJ. Long-term survival of patients undergoing liver resection for very large hepatocellular carcinomas. Br J Surg 2016;103:1513–1520.
Takatsuki M, Tokunaga S, Uchida S, Sakoda M, Shirabe K, Beppu T, Emi Y, Oki E, Ueno S, Eguchi S, Akagi Y, Ogata Y, Baba H, Natsugoe S, Maehara Y; Kyushu Study Group of Clinical Cancer (KSCC). Evaluation of resectability after neoadjuvant chemotherapy for primary non-resectable colorectal liver metastases: A multicenter study. Eur J Surg Oncol 2016;42:184–189.
Zhang X-F, Bagante F, Chakedis J, Moris D, Beal EW, Weiss M, Popescu I, Marques HP, Aldrighetti L, Maithel SK, Pulitano C, Bauer TW, Shen F, Poultsides GA, Soubrane O, Martel G, Groot Koerkamp B, Guglielmi A, Itaru E, Pawlik TM. Perioperative and Long-Term Outcome for Intrahepatic Cholangiocarcinoma: Impact of Major Versus Minor Hepatectomy. J. Gastrointest. Surg. 2017;21:1841–1850.
Hanau LH, Steigbigel NH. Acute (ascending) cholangitis. Infect. Dis. Clin. North Am 2000;14:521–546.
Cammann S, Timrott K, Vonberg R-P, Vondran FW, Schrem H, Suerbaum S, Klempnauer J, Bektas H, Kleine M. Cholangitis in the postoperative course after biliodigestive anastomosis. Langenbecks Arch Surg 2016;401:715–724.
Dimou FM, Adhikari D, Mehta HB, Olino K, Riall TS, Brown KM. Incidence of hepaticojejunostomy stricture after hepaticojejunostomy. Surgery 2016;160:691–698.
Moris D, Papalampros A, Vailas M, Petrou A, Kontos M, Felekouras E. The hepaticojejunostomy technique with intra-anastomotic stent in biliary diseases and its evolution throughout the years: a technical analysis. Gastroenterol Res Pract 2016 2016; 3692096.
Tocchi A, Mazzoni G, Liotta G, Lepre L, Cassini D, Miccini M. Late development of bile duct cancer in patients who had biliary-enteric drainage for benign disease: a follow-up study of more than 1,000 patients. Ann. Surg 2001;234:210–214.
Bennet W, Zimmerman MA, Campsen J, Mandell MS, Bak T, Wachs M, Kam I. Choledochoduodenostomy is a safe alternative to Roux-en-Y choledochojejunostomy for biliary reconstruction in liver transplantation. World J Surg 2009;33:1022–1025.
Goumard C, Cachanado M, Herrero A, Rousseau G, Dondero F, Compagnon P, Boleslawski E, Mabrut JY, Salamé E, Soubrane O, Simon T, Scatton O. Biliary reconstruction with or without an intraductal removable stent in liver transplantation: study protocol for a randomized controlled trial. Trials 2015;16:598.
Tranchart H, Zalinski S, Sepulveda A, Chirica M, Prat F, Soubrane O, Scatton O. Removable intraductal stenting in duct-to-duct biliary reconstruction in liver transplantation. Transpl. Int 2012;25:19–24.
Endo I, Shimada H, Takeda K, Fujii Y, Yoshida K, Morioka D, Sadatoshi S, Togo S, Bourquain H, Peitgen HO. Successful duct-to-duct biliary reconstruction after right hemihepatectomy. Operative planning using virtual 3D reconstructed images. J. Gastrointest. Surg 2007;11:666–670.
Hashimoto T, Kokudo N, Hasegawa K, Sano K, Imamura H, Sugawara Y, Makuuchi M. Reappraisal of duct-to-duct biliary reconstruction in hepatic resection for liver tumors. Am. J. Surg 2007;194:283–287.
Memeo R, Belli A, Kluger MD, Tayar C, Laurent A, Cherqui D. Duct-to-duct biliary reconstruction during complex hepatectomy: a useful technique in selected cases. World J Surg 2012;36:129–135.
Dindo D, Demartines N, Clavien P-A. Classification of Surgical Complications. Ann Surg 2004;240:205–213.
Shimoda M, Saab S, Morrisey M, Ghobrial RM, Farmer DG, Chen P, Han SH, Bedford RA, Goldstein LI, Martin P, Busuttil RW. A cost-effectiveness analysis of biliary anastomosis with or without T-tube after orthotopic liver transplantation. Am. J. Transplant 2001;1:157–161.
Scatton O, Meunier B, Cherqui D, Boillot O, Sauvanet A, Boudjema K, Launois B, Fagniez PL, Belghiti J, Wolff P, Houssin D, Soubrane O. Randomized trial of choledochocholedochostomy with or without a T tube in orthotopic liver transplantation. Ann. Surg 2001;233:432–437.
Santosh Kumar KY, Mathew JS, Balakrishnan D, Bharathan VK, Thankamony Amma BSP, Gopalakrishnan U, Narayana Menon R, Dhar P, Vayoth SO, Sudhindran S. Intraductal Transanastomotic Stenting in Duct-to-Duct Biliary Reconstruction after Living-Donor Liver Transplantation: A Randomized Trial. J. Am. Coll. Surg 2017;225:747–754.
Kadaba RS, Bowers KA, Khorsandi S, Hutchins RR, Abraham AT, Sarker SJ, Bhattacharya S, Kocher HM. Complications of biliary-enteric anastomoses. Ann R Coll Surg Engl 2017;99:210–215.
de Castro SMM, Kuhlmann KFD, Busch ORC, van Delden OM, Laméris JS, van Gulik TM, Obertop H, Gouma DJ. Incidence and management of biliary leakage after hepaticojejunostomy. J. Gastrointest. Surg 2005;9:1163–1173.
Schumacher B, Othman T, Jansen M, Preiss C, Neuhaus H. Long-term follow-up of percutaneous transhepatic therapy (PTT) in patients with definite benign anastomotic strictures after hepaticojejunostomy. Endoscopy 2001;33:409–415.
Fontein DBY, Gibson RN, Collier NA, Tse GT, Wang LL, Speer TG, Dowling R, Robertson A, Thomson B, de Roos A. Two decades of percutaneous transjejunal biliary intervention for benign biliary disease: a review of the intervention nature and complications. Insights Imaging 2011;2:557–565.
Acknowledgments
Dr. R. Brustia for the schematic drawing explaining the surgical procedure.
Author information
Authors and Affiliations
Contributions
Study concept and design: M. Collard, J. Danion, F. Cauchy, O. Soubrane, O. Scatton. Data collection, analysis, and interpretation: M. Collard, F. Perdigao, S. Leblanc, F. Prat, O. Scatton. Writing: M. Collard, J. Danion, O. Scatton Critical revision: F. Cauchy, F. Perdigao, S. Leblanc, F. Prat, O. Soubrane. All authors approved the final version to be published. Each author is accountable for all aspects of the work.
Corresponding author
Electronic supplementary material
Video 1
(MOV 64283 kb)
Rights and permissions
About this article
Cite this article
Collard, M.K., Danion, J., Cauchy, F. et al. Duct-To-Duct Biliary Anastomosis with Removable Internal Biliary Stent During Major Hepatectomy Extended to the Biliary Confluence. J Gastrointest Surg 22, 2201–2208 (2018). https://doi.org/10.1007/s11605-018-3905-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-018-3905-8