Abstract
Background
Gastric cardia cancer is currently treated with several operations. The purpose of the current study was to compare outcomes associated with three common operative approaches.
Methods
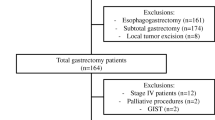
The ACS-NSQIP Participant Use File was searched to identify all patients with gastric cardia malignancy who underwent total gastrectomy (TG), transhiatal esophagectomy (THE), or thoraco-abdominal esophagectomy (TAE) between 2005 and 2012. Demographic, perioperative risk factors, and outcomes were analyzed.
Results
Overall, there were 982 patients identified in the database who met inclusion criteria. The median age was 65 years (range 20–88) and 807 (82.2 %) were male. The number of patients allocated to each approach was 204 TGs (20.8 %), 271 THE (27.6 %), and 507 TAE (51.6 %). All approaches had similar major morbidity, cardiopulmonary morbidity, and 30-day mortality, however, TAE was associated with the highest overall morbidity (TAE 49.9 % vs. TG 40.7 % and THE 43.5 %, p = 0.048). The independent risk factors predicting mortality were age greater than 65 years, history of myocardial infarction, and postoperative cardiopulmonary morbidity.
Conclusions
For patients with proximal gastric cancer, the three most common operative approaches were associated with clinically-significant rates of overall and major morbidity. Approach-associated morbidity should be considered along with tumor location and extent when choosing a technique for resection of gastric cardia malignancy.

Similar content being viewed by others
References
Husemann B. Cardia carcinoma considered as a distinct clinical entity. Br J Surg. 1989;76(2):136–139.
Edge S BD, Compton Cc, Fritz Ag, Green Fl, Trotti A. AJCC Cancer Staging Manual. 2010.
Rice TW, Blackstone EH and Rusch VW. 7th edition of the AJCC Cancer Staging Manual: esophagus and esophagogastric junction. Ann Surg Oncol. 2010;17(7):1721–1724.
Siewert JR, Holscher AH, Becker K and Gossner W. [Cardia cancer: attempt at a therapeutically relevant classification]. Chirurg. 1987;58(1):25–32.
Jemal A, Bray F, Center MM, Ferlay J, Ward E and Forman D. Global cancer statistics. CA Cancer J Clin. 2011;61(2):69–90.
Blot WJ, Devesa SS, Kneller RW and Fraumeni JF, Jr. Rising incidence of adenocarcinoma of the esophagus and gastric cardia. JAMA. 1991;265(10):1287–1289.
Devesa SS, Blot WJ and Fraumeni JF, Jr. Changing patterns in the incidence of esophageal and gastric carcinoma in the United States. Cancer. 1998;83(10):2049–2053.
Vial M, Grande L and Pera M. Epidemiology of adenocarcinoma of the esophagus, gastric cardia, and upper gastric third. Recent Results Cancer Res. 2010;182:1–17.
Papenfuss WA, Kukar M, Oxenberg J, Attwood K, Nurkin S, Malhotra U and Wilkinson NW. Morbidity and Mortality Associated with Gastrectomy for Gastric Cancer. Ann Surg Oncol. 2014.
Martin JT, Mahan A, Zwischenberger JB, Mcgrath PC and Tzeng CW. Should Gastric Cardia Cancers Be Treated with Esophagectomy or Total Gastrectomy? A Comprehensive Analysis of 4,996 NSQIP/SEER Patients. J Am Coll Surg. 2015;220(4):510–520.
Yang K, Chen HN, Chen XZ, Lu QC, Pan L, Liu J, Dai B, Zhang B, Chen ZX, Chen JP and Hu JK. Transthoracic resection versus non-transthoracic resection for gastroesophageal junction cancer: a meta-analysis. PLoS One. 2012;7(6):e37698.
Ahmed S, Iqbal N, Yadav S, Zaidi A, Ahmed O, Alvi R, Gardner D and Haider K. Time to adjuvant therapy and other variables in localized gastric and gastroesophageal junction (GEJ) cancer (IJGC-D-13-00162). J Gastrointest Cancer. 2014;45(3):284–290.
Lerut T, Moons J, Coosemans W, Van Raemdonck D, De Leyn P, Decaluwe H, Decker G and Nafteux P. Postoperative complications after transthoracic esophagectomy for cancer of the esophagus and gastroesophageal junction are correlated with early cancer recurrence: role of systematic grading of complications using the modified Clavien classification. Ann Surg. 2009;250(5):798–807.
Xia BT, Rosato EL, Chojnacki KA, Crawford AG, Weksler B and Berger AC. Major perioperative morbidity does not affect long-term survival in patients undergoing esophagectomy for cancer of the esophagus or gastroesophageal junction. World J Surg. 2013;37(2):408–415.
Aloia TA, Zimmitti G, Conrad C, Gottumukalla V, Kopetz S and Vauthey JN. Return to intended oncologic treatment (RIOT): a novel metric for evaluating the quality of oncosurgical therapy for malignancy. J Surg Oncol. 2014;110(2):107–114.
Acs. User Guide for the 2012 ACS NSQIP. 2012.
Tzeng CW, Cooper AB, Vauthey JN, Curley SA and Aloia TA. Predictors of morbidity and mortality after hepatectomy in elderly patients: analysis of 7621 NSQIP patients. HPB (Oxford). 2014;16(5):459–468.
Huscher CG, Mingoli A, Sgarzini G, Sansonetti A, Di Paola M, Recher A and Ponzano C. Laparoscopic versus open subtotal gastrectomy for distal gastric cancer: five-year results of a randomized prospective trial. Ann Surg. 2005;241(2):232–237.
Biere SS, Van Berge Henegouwen MI, Maas KW, Bonavina L, Rosman C, Garcia JR, Gisbertz SS, Klinkenbijl JH, Hollmann MW, De Lange ES, Bonjer HJ, Van Der Peet DL and Cuesta MA. Minimally invasive versus open oesophagectomy for patients with oesophageal cancer: a multicentre, open-label, randomised controlled trial. Lancet. 2012;379(9829):1887–1892.
Ito H, Clancy TE, Osteen RT, Swanson RS, Bueno R, Sugarbaker DJ, Ashley SW, Zinner MJ and Whang EE. Adenocarcinoma of the gastric cardia: what is the optimal surgical approach? J Am Coll Surg. 2004;199(6):880–886.
Lerut T, Moons J, Coosemans W, Decaluwe H, Decker G, De Leyn P, Nafteux P and Van Raemdonck D. Multidisciplinary treatment of advanced cancer of the esophagus and gastroesophageal junction: a European center's approach. Surg Oncol Clin N Am. 2008;17(3):485–502, vii-viii.
Meyer HJ. The influence of case load and the extent of resection on the quality of treatment outcome in gastric cancer. Eur J Surg Oncol. 2005;31(6):595–604.
Coupland VH, Lagergren J, Luchtenborg M, Jack RH, Allum W, Holmberg L, Hanna GB, Pearce N and Moller H. Hospital volume, proportion resected and mortality from oesophageal and gastric cancer: a population-based study in England, 2004–2008. Gut. 2013;62(7):961–966.
Anderson O, Ni Z, Moller H, Coupland VH, Davies EA, Allum WH and Hanna GB. Hospital volume and survival in oesophagectomy and gastrectomy for cancer. Eur J Cancer. 2011;47(16):2408–2414.
Author information
Authors and Affiliations
Corresponding author
Additional information
Primary Discussant
Kyle A. Perry, M.D. (Columbus, OH)
Thank you for sharing this nicely presented study examining the surgical approaches utilized to manage proximal gastric cancers. Proximal gastric cancer presents a challenging clinical dilemma, and consideration of oncologic outcome, the rate of return to normal functional status postoperatively, and perioperative risk all play an important role in planning the operative approach. This study aimed to identify predictive factors that predispose patients to major morbidity following esophagectomy or extended total gastrectomy in order to guide clinical decision making. In light of this, why was the decision made to combine the total gastrectomy and transhiatal esophagectomy groups in the multivariate analysis? These operations are associated with different risks and consequences, and it seems that analyzing them separately may identify different predictors for postoperative complications. Also, you noted significant differences between the patient populations undergoing esophagectomy and gastrectomy. Is it possible that a subset of the total gastrectomy patients was undergoing palliative surgery for inability to tolerate oral intake rather than a curative operation? If so, how might this influence the interpretation of the results. Congratulations again on an excellent presentation, and thank for the opportunity to discuss it.
Closing Discussant
Dr. Day
We thank the Dr. Perry for these insightful comments and questions.
Regarding the grouping of cases, initially each of the approaches was separately analyzed. However, there was recognition that the combined abdomino-thoracic approach may have a different complication profile compared to the two non-thoracotomy approaches (total gastrectomy and transhiatal esophagogastrectomy). The separate analysis yielded similar results to the combined analysis, but due to the small number of some comorbidities, the 95 % confidence intervals were very large. Since both groups had similar outcomes for the same disease, the decision was made to combine the analysis for increased power in the face of small numbers, allowing the potential to specifically comment on the morbidity of thoracotomy.
Regarding the use of total gastrectomy as a palliative maneuver, it is possible that some individuals underwent surgery without curative intent. Unfortunately, oncologic intent and stage of disease cannot be obtained from the NSQIP PUF. This having been said, we believe that most patients undergoing palliation for gastric cardia cancer would not have a total gastrectomy as the operation of choice in that scenario. Given the contemporary cohort, stenting, partial gastrectomy, bypass, or palliative feeding tube placement, which were excluded from the analysis, seem to be more likely surgical palliation options for this disease.
NSQIP Disclaimer
The American College of Surgeons National Surgical Quality Improvement Program and the hospitals participating in it represent the source of the data used herein; they have not verified and are not responsible for the statistical validity of the data analysis or for the conclusions derived by the authors.
This manuscript was presented in a plenary session at the Annual Meeting of the SSAT on May 18th, 2015.
Rights and permissions
About this article
Cite this article
Day, R.W., Badgwell, B.D., Fournier, K.F. et al. Defining the Impact of Surgical Approach on Perioperative Outcomes for Patients with Gastric Cardia Malignancy. J Gastrointest Surg 20, 146–153 (2016). https://doi.org/10.1007/s11605-015-2949-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-015-2949-2