Abstract
Background
Postoperative pancreatic fistula (POPF) is a severe complication after pancreatic resections. The aim was to assess if application of TachoSil® patch could reduce incidence of postoperative fistulas after laparoscopic distal pancreatic resections.
Methods
This is a retrospective study of prospectively collected data after enucleations and distal pancreatic resections. Patients were divided in two groups: with or without application of TachoSil® patch. Demographic and surgical data were analyzed.
Results
One hundred twenty-one patients with distal pancreatic resections without additional resections were identified among 230 patients operated by laparoscopic approach at our institution since 1998. They were divided into two groups. In group 1 (n = 48), TachoSil® patch was not applied while in group 2 (n = 73), the pancreatic stump was covered with TachoSil®. Postoperative fistulas were registered in 8% (4/48) and 12% (9/73) in groups 1 and 2, respectively. The median duration of postoperative hospital stay in group 1 was 5.5 (2–35) days compared with 5 (2–16) days in group 2. No significant difference in surgical outcomes was found.
Conclusions
The application of the TachoSil® patch did not affect either occurrence of POPF or duration of postoperative hospital stay. Routine use of TachoSil® patch to prevent pancreatic fistulas does not provide clinically significant benefit.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The laparoscopic approach for distal pancreatic resections has gained increased acceptance for several indications during the past decade and an increasing number of patients is operated by this method both for nonmalignant as well as for malignant diseases. There is increasing documentation that both endocrine tumors, cystic lesions, metastatic lesions, and adenocarcinomas can be safely operated by the laparoscopic approach1–3 and the implementation of minimally invasive techniques has led to reduced morbidity.4,5 Despite this, perioperative bleeding and pancreatic leakage still remain a challenge for the surgeons. General morbidity rate and perioperative hemorrhage is generally lower for laparoscopic procedures6, but there is no conclusive evidence that minimally invasive surgery leads to reduced POPF rate after distal pancreas resections. Various centers have published different rates of POPF varying from 0% to 32% as defined by the International study group on pancreatic fistulas (ISGPF).7 In our institution, the overall fistula rate after laparoscopic resections of the pancreas has been 10%.2
The continuous search for the new and more effective remedies and techniques to prevent POPF remains is important. In January 2005, we introduced the surgical patch TachoSil® (Nycomed, Pharmaceutical Co. Ltd, Denmark) to cover the resection margin of the pancreas after laparoscopic resections. It was announced as a fast and reliable remedy for haemostasis and sealing of soft tissues. These argued characteristics corresponded to our needs in order to prevent postoperative complications. This study evaluated TachoSil as a prevention remedy for postoperative pancreatic fistula (POPFs) in pancreatic surgery.
Patients and Methods
Patients
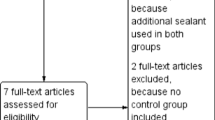
A total of 230 patients underwent laparoscopic pancreas resections in our institution from March 1997 to December 2010. After exclusion of local tumor resections (n = 36), procedures with additional resections of adjacent organs (n = 29), procedures where other types of protection of surgical margin were used (n = 14), converted procedures or accomplished as hand assisted (n = 5), and explorative and other types of procedures (n = 25) a total of 121 patients undergoing distal pancreatic resection (DPR) with or without splenectomy, were left for analysis. All procedures were performed by the same group of surgeons. From January 2005 majority of the procedures have been completed with covering of surgical margin and part of pancreatic remnant by TachoSil patch for to prevent postoperative pancreatic fistulas and potential postoperative bleeding. To that time not all effects of this remedy were clear and good documented, especially about its effectiveness in pancreatic surgery.
Indications to surgical procedures were endocrine tumors, cystic lesions, adenocarcinomas, and others as described in our previous publication.
The patients were retrospectively divided in two groups according to the final management of the surgical margin. In the first group (group 1, consisting of 48 patients (32 women and 16 men) with a median age of 62 (30–81) years and median ASA score of 2 (1–3)), the pancreas was divided by a linear stapler and left without additional covering. In the second group (group 2, consisting of 73 patients (49 women and 24 men) with a median age of 60 (16–82) years and median ASA score of 2 (1–3)), the staple line of the resection margin was covered with a TachoSil® patch. As our method for pancreas division has been described in detail earlier,2,8 this study focused only on the final part of the procedure.
Data were analyzed retrospectively. Patient’s characteristics are presented in Table 1.
Outcome Parameters
According to the ISGPF definition, pancreatic fistula was defined as a drainage fluid beyond the third postoperative day with at least threefold elevation of normal serum amylase. The grading system (grades A, B, and C) of severity of pancreatic fistula was applied (Table 2).9
Postoperative complications were registered in accordance with a last revision of the accordion classification, from mild complications (grade 1) to death of the patient—(grade 6) as described in Table 3.10
Statistical Analysis
Statistical analysis was conducted using SPSS 16, 0. Data were presented as median (range). For comparison of frequencies, the Chi-square test was performed. For comparison of the continuous variables, Mann–Whitney U test was used.
Results
Out of 230 patients, 121 were included in this study of which 91 were DPR with splenectomy and 30 were DPR performed as spleen-preserving procedures. Details regarding the indications for surgery are summarized in Table 4. All procedures were completed laparoscopically. Data regarding the surgical details are described in Table 5:
In group 1, 38 DPR with splenectomy and ten spleen-preserving resections were performed without using TachoSil. The median operative time for these procedures was 202 (29–350) minutes and the median intraoperative bleeding was 50 (0–1,500) ml. There were three grade 1, two grade 2, four grade 3, and two grade 4 events. Four patients developed pancreatic fistula of which all were grade B. The overall morbidity in the group was 30%. The median duration of postoperative hospital stay for group 1 was 5 (2–16) days.
In group 2, we included only those procedures where the pancreatic remnant was covered with TachoSil®. In this group, 53 procedures were DPR with splenectomy and 20 spleen-preserving DPR. The median operative time was 158 (88–608) min, and the median intraoperative bleeding was 50 (5–3,000) ml. The postoperative morbidity included four grade 1 event, three grade 2, one grade 3 event, and three grade 4 events. Postoperative pancreatic leakage was registered in ten patients of which one grade A, six grade B, and three grade C fistulas. The overall morbidity rate in group 2 was 30%, and the median duration of postoperative hospital stay was 5.5 (2–35) days.
No postoperative mortality was recorded in any of the groups. Detailed description over all postoperative complications is shown in Table 6. We did not find statistical difference in postoperative data between these two groups.
Discussion
Laparoscopic DPR have steadily gained acceptance as a method for surgical removal of both benign and malignant lesions in the tail and body of the pancreas.
The technique not only shows better cosmetic results but is also associated with reduced bleeding and overall morbidity rate compared with traditional open surgery.11 It is unclear if the method influences the rate of postoperative pancreatic leakage since no randomized studies has been conducted while comparing the techniques. There are, however, studies in which a trend has been reported about nonsignificant reduced rate of POPF after minimally invasive procedures.6
Pancreatic leakage is one of the most commonly encountered severe complications following pancreatic resections and leak rates up to 46% has been described.12 Several different techniques have been attempted in order to prevent fistulas and some authors mean that management of the resectional margin of pancreatic stump is very important. To develop a standardized technique which can demonstrate a significant decrease in overall morbidity including fistula formation is important.
Better results and safety of the patient is a major concern of any surgical procedures and laparoscopic pancreas resection is no exception. One contribution for the decreased overall morbidity in pancreatic surgery during the last years is the introduction of new staplers, electrosurgical instruments, surgical methods, and other technical and pharmaceutical remedies. TachoSil® is a fixed combination of a patch sponge coated with a dry layer of the human coagulation factors fibrinogen and thrombin. TachoSil® is indicated for supportive treatment in surgery, for improvement of haemostasis, to promote tissue sealing and for suture support in vascular surgery where standard techniques are insufficient.
The haemostatic effect of Tachosil patch in surgical procedures is well documented in the literature13 in a wide variety of organs.14
Since the TachoSil® patch was also reported to be of value in terms of sealing surgical resection surfaces; we postulated it to be of value also in pancreas resections in which fistula formation continued to constitute a problem. Covering of the stapling line on the cut surface of the pancreas therefore became a routine part of the procedure since 2005.
It was described as predicting factors for development of pancreatic fistulas15, and we tried to look if TachoSil® patch could be beneficial in special cases. In the present series, we found that in the first group (without application of TachoSil) fistulas were registered only in soft glands whereas in the second (where TachoSil was applied on the resectional line) 30% (three out of ten) of all fistulas developed in the hard glands. To make any conclusions based on these results is difficult. We did not experience serious blood loss (≤1,000 ml) in any of these cases.
When we designed this retrospective study we were aware about its limitations and have tried to diminish their possibility. To avoid selection bias only distal resections with or without splenectomy independent of other factors (age, pathology, etc.) were included to the study. Chances that some of the patients fall out of control were equal for both groups. However, due to general low rate of fistulas in our material, one should be aware about possibility of statistical type 2 error.
In this study, however we did not observe significant differences in any of the studied parameters between patients in whom stapling line was covered by TachoSil patch after the resection and those without it. Somewhat surprisingly, grade C fistulas were only observed in patients in group 2, in which TachoSil® was used. The reason for this is unclear. One possible explanation could be that reducing of the natural outflow from the pancreatic remnant can lead to accumulation of ferments and thereby impair the normal process of postoperative healing. To make any conclusion about this, randomized studies are needed.
The haemostatic effect of TachoSil® in various procedures makes the product of great value in complex laparoscopic procedures.
Present data do not support the use of the TachoSil® patch for the prevention of fistulas following distal pancreatic resections.
References
Cuschieri, S. A., and Jakimowicz, J. J. Laparoscopic pancreatic resections. Semin. Laparosc. Surg. 5:168–179, 1998.
Rosok, B. I., Marangos, I. P., Kazaryan, A. M., Rosseland, A. R., Buanes, T., Mathisen, O., and Edwin, B. Single-centre experience of laparoscopic pancreatic surgery191. Br. J. Surg. 97:902–909, 2010.
Fernandez-Cruz, L., Herrera, M., Saenz, A., Pantoja, J. P., Astudillo, E., and Sierra, M. Laparoscopic pancreatic surgery in patients with neuroendocrine tumours: indications and limits. Best Practice and Research Clinical Endocrinology and Metabolism 15:161–175, 2001.
Bassi, C., Butturini, G., Molinari, E., Mascetta, G., Salvia, R., Falconi, M., Gumbs, A., and Pederzoli, P. Pancreatic fistula rate after pancreatic resection. The importance of definitions. Dig. Surg. 21:54–59, 2004.
DeOliveira, M. L., Winter, J. M., Schafer, M., Cunningham, S. C., Cameron, J. L., Yeo, C. J., and Clavien, P. A. Assessment of complications after pancreatic surgery: a novel grading system applied to 633 patients undergoing pancreaticoduodenectomy 6. Ann. Surg. 244:931–937, 2006.
Nigri, G. R., Rosman, A. S., Petrucciani, N., Fancellu, A., Pisano, M., Zorcolo, L., Ramacciato, G., and Melis, M. Metaanalysis of trials comparing minimally invasive and open distal pancreatectomies 1. Surg. Endosc. 25(5):1642–1651, 2010
Kooby, D. A., Gillespie, T., Bentrem, D., Nakeeb, A., Schmidt, M. C., Merchant, N. B., Parikh, A. A., Martin, R. C., Scoggins, C. R., Ahmad, S., Kim, H. J., Park, J., Johnston, F., Strouch, M. J., Menze, A., Rymer, J., McClaine, R., Strasberg, S. M., Talamonti, M. S., Staley, C. A., McMasters, K. M., Lowy, A. M., Byrd-Sellers, J., Wood, W. C., and Hawkins, W. G. Left-sided pancreatectomy: a multicenter comparison of laparoscopic and open approaches 8. Annals of Surgery 248:438–446, 2008.
Edwin, B., Mala, T., Mathisen, O., Gladhaug, I., Buanes, T., Lunde, O. C., Soreide, O., Bergan, A., and Fosse, E. Laparoscopic resection of the pancreas: a feasibility study of the short-term outcome 14. Surgical Endoscopy 18:407–411, 2004.
Bassi, C., Dervenis, C., Butturini, G., Fingerhut, A., Yeo, C., Izbicki, J., Neoptolemos, J., Sarr, M., Traverso, W., and Buchler, M. Postoperative pancreatic fistula: an international study group (ISGPF) definition. Surgery 138:8–13, 2005.
Porembka, M. R., Hall, B. L., Hirbe, M., and Strasberg, S. M. Quantitative weighting of postoperative complications based on the accordion severity grading system: demonstration of potential impact using the american college of surgeons national surgical quality improvement program 2. J. Am. Coll. Surg. 210:286–298, 2010.
Weber, S. M., Cho, C. S., Merchant, N., Pinchot, S., Rettammel, R., Nakeeb, A., Bentrem, D., Parikh, A., Mazo, A. E., Martin, R. C., III, Scoggins, C. R., Ahmad, S. A., Kim, H. J., Hamilton, N., Hawkins, W., Max, S. C., and Kooby, D. A. Laparoscopic left pancreatectomy: complication risk score correlates with morbidity and risk for pancreatic fistula. Ann. Surg. Oncol. 16:2825–2833, 2009.
Moskovic, D. J., Hodges, S. E., Wu, M. F., Brunicardi, F. C., Hilsenbeck, S. G., and Fisher, W. E. Drain data to predict clinically relevant pancreatic fistula. HPB (Oxford) 12:472–481, 2010.
Siemer, S., Lahme, S., Altziebler, S., Machtens, S., Strohmaier, W., Wechsel, H. W., Goebell, P., Schmeller, N., Oberneder, R., Stolzenburg, J. U., Becker, H., Luftenegger, W., Tetens, V., and Van, P. H. Efficacy and safety of TachoSil as haemostatic treatment versus standard suturing in kidney tumour resection: a randomised prospective study 1. Eur. Urol. 52:1156–1163, 2007.
Kazaryan, A. M., Pavlik, M., I, Rosseland, A. R., Rosok, B. I., Mala, T., Villanger, O., Mathisen, O., Giercksky, K. E., and Edwin, B. Laparoscopic liver resection for malignant and benign lesions: ten-year Norwegian single-center experience 4. Arch. Surg. 145:34–40, 2010.
Pratt, W. B., Callery, M. P., and Vollmer, C. M., Jr. Risk prediction for development of pancreatic fistula using the ISGPF classification scheme 8. World J. Surg. 32:419–428, 2008.
Conflicts of Interest
The authors declare that they have no conflict of interest.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Pavlik Marangos, I., Røsok, B.I., Kazaryan, A.M. et al. Effect of TachoSil Patch in Prevention of Postoperative Pancreatic Fistula. J Gastrointest Surg 15, 1625–1629 (2011). https://doi.org/10.1007/s11605-011-1584-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-011-1584-9