Abstract
Purpose
Efficacy of F-18 fluorodeoxyglucose positron emission tomography combined with computed tomography (FDG-PET/CT) for determining neoadjuvant therapy response in rectal cancer is not well established. We sought to evaluate serial FDG-PET/CT for assessing tumor down-staging, percentage residual tumor, and complete response or microscopic disease with rectal cancer neoadjuvant therapy.
Methods
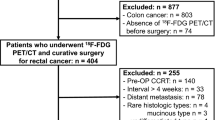
Patients with rectal cancer undergoing neoadjuvant therapy, definitive surgical resection, and FDG-PET/CT before and 4–6 weeks after neoadjuvant treatment were included. Tumors were evaluated pretreatment and on final pathology for size and stage. FDG-PET/CT parameters assessed were visual response score (VRS), standardized uptake value (SUV), PET-derived tumor volume (PETvol), CT-derived tumor volume (CTvol), and total lesion glycolysis (δTLG).
Results
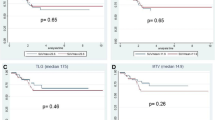
Twenty-one rectal cancer patients over 3 years underwent neoadjuvant treatment, serial FDG-PET/CT, and resection. Complete response or microscopic disease (n = 7, 33%) was associated with higher ΔCTvol (AUC = 0.82, p = 0.004) and ΔSUV (AUC = 0.79, p = 0.01). Tumor down-staging (n = 14, 67%) was associated with greater ΔPETvol (AUC = 0.82, p < 0.001) and ΔSUV (AUC = 0.82, p < 0.001). Pathologic lymph node disease (n = 7, 33%) correlated with ΔCTvol (AUC = 0.75, p = 0.03) and ΔPETvol (AUC = 0.70, p = 0.08).
Conclusion
FDG-PET/CT parameters were best for assessing tumor down-staging and percentage of residual tumor after neoadjuvant treatment of rectal cancer and can potentially assist in treatment planning.


Similar content being viewed by others
References
Improved survival with preoperative radiotherapy in resectable rectal cancer. Swedish Rectal Cancer Trial. N Engl J Med 1997;336(14):980–987.
Sauer R, Becker H, Hohenberger W, et al. Preoperative versus postoperative chemoradiotherapy for rectal cancer. N Engl J Med 2004;351(17):1731–1740.
Wolmark N, Wieand HS, Hyams DM, et al. Randomized trial of postoperative adjuvant chemotherapy with or without radiotherapy for carcinoma of the rectum: National Surgical Adjuvant Breast and Bowel Project Protocol R-02. J Natl Cancer Inst 2000;92(5):388–396.
Guillem JG, Chessin DB, Cohen AM, et al. Long-term oncologic outcome following preoperative combined modality therapy and total mesorectal excision of locally advanced rectal cancer. Ann Surg 2005;241(5):829–836; Discussion 36–38.
Jemal A, Tiwari RC, Murray T, et al. Cancer statistics, 2004. CA Cancer J Clin 2004;54(1):8–29.
Schaffzin DM, Wong WD. Endorectal ultrasound in the preoperative evaluation of rectal cancer. Clin Colorectal Cancer 2004;4(2):124–132.
Zerhouni EA, Rutter C, Hamilton SR, et al. CT and MR imaging in the staging of colorectal carcinoma: report of the Radiology Diagnostic Oncology Group II. Radiology 1996;200(2):443–451.
Joyce D, Wahl R, Patel P, Schulick R, Gearhart S, Choti M. Preoperative PET to evaluate potentially resectable hepatic colorectal metastases. Arch Surg 2006;141(12):1220–1226.
Ogunbiyi OA, Flanagan FL, Dehdashti F, et al. Detection of recurrent and metastatic colorectal cancer: comparison of positron emission tomography and computed tomography. Ann Surg Oncol 1997;4(8):613–620.
Staib L, Schirrmeister H, Reske SN, Beger HG. Is (18)F-fluorodeoxyglucose positron emission tomography in recurrent colorectal cancer a contribution to surgical decision making? Am J Surg 2000;180(1):1–5.
Even-Sapir E, Parag Y, Lerman H, et al. Detection of recurrence in patients with rectal cancer: PET/CT after abdominoperineal or anterior resection. Radiology 2004;232(3):815–822.
Cohade C, Osman M, Leal J, Wahl RL. Direct comparison of (18)F-FDG PET and PET/CT in patients with colorectal carcinoma. J Nucl Med 2003;44(11):1797–1803.
Gearhart SL, Frassica D, Rosen R, Choti M, Schulick R, Wahl R. Improved staging with pretreatment positron emission tomography/computed tomography in low rectal cancer. Ann Surg Oncol 2006;13(3):397–404.
American Joint Committee on Cancer. AJCC cancer staging manual. 6th ed. New York: Springer-Verlag, 2002.
Rusch V, Klimstra D, Venkatraman E, et al. Aberrant p53 expression predicts clinical resistance to cisplatin-based chemotherapy in locally advanced non-small cell lung cancer. Cancer Res 1995;55(21):5038–5042.
Young H, Baum R, Cremerius U, et al. Measurement of clinical and subclinical tumour response using [18F]-fluorodeoxyglucose and positron emission tomography: review and 1999 EORTC recommendations. European Organization for Research and Treatment of Cancer (EORTC) PET Study Group. Eur J Cancer 1999;35(13):1773–1782.
Larson SM, Erdi Y, Akhurst T, et al. Tumor treatment response based on visual and quantitative changes in global tumor glycolysis using PET-FDG imaging. The Visual Response Score and the Change in Total Lesion Glycolysis. Clin Positron Imaging 1999;2(3):159–171.
Eng J. Receiver operating characteristic analysis: a primer. Acad Radiol 2005;12(7):909–916.
Gibbons JD. Nonparametric methods for quantitative analysis, 3rd ed. Ohio: American Sciences Press Inc., 1997.
Rodel C, Grabenbauer GG, Papadopoulos T, Hohenberger W, Schmoll HJ, Sauer R. Phase I/II trial of capecitabine, oxaliplatin, and radiation for rectal cancer. J Clin Oncol 2003;21(16):3098–3104.
Gerard JP, Chapet O, Nemoz C, et al. Preoperative concurrent chemoradiotherapy in locally advanced rectal cancer with high-dose radiation and oxaliplatin-containing regimen: the Lyon R0-04 phase II trial. J Clin Oncol 2003;21(6):1119–1124.
Aschele C, Friso ML, Pucciarelli S, et al. A phase I-II study of weekly oxaliplatin, 5-fluorouracil continuous infusion and preoperative radiotherapy in locally advanced rectal cancer. Ann Oncol 2005;16(7):1140–1146.
Capirci C, Rubello D, Chierichetti F, et al. Restaging after neoadjuvant chemoradiotherapy for rectal adenocarcinoma: role of F18-FDG PET. Biomed Pharmacother 2004;58(8):451–457.
Liersch T, Langer C, Jakob C, et al. [Preoperative diagnostic procedures in locally advanced rectal carcinoma (> or =T3 or N+). What does endoluminal ultrasound achieve at staging and restaging (after neoadjuvant radiochemotherapy) in contrast to computed tomography? Chirurg 2003;74(3):224–234.
Calvo FA, Domper M, Matute R, et al. 18F-FDG positron emission tomography staging and restaging in rectal cancer treated with preoperative chemoradiation. Int J Radiat Oncol Biol Phys 2004;58(2):528–535.
Guillem JG, Puig-La Calle J, Jr., Akhurst T, et al. Prospective assessment of primary rectal cancer response to preoperative radiation and chemotherapy using 18-fluorodeoxyglucose positron emission tomography. Dis Colon Rectum 2000;43(1):18–24.
Amthauer H, Denecke T, Rau B, et al. Response prediction by FDG-PET after neoadjuvant radiochemotherapy and combined regional hyperthermia of rectal cancer: correlation with endorectal ultrasound and histopathology. Eur J Nucl Med Mol Imaging 2004;31(6):811–819.
Brucher BL, Weber W, Bauer M, et al. Neoadjuvant therapy of esophageal squamous cell carcinoma: response evaluation by positron emission tomography. Ann Surg 2001;233(3):300–309.
Hersh MR, Choi J, Garrett C, Clark R. Imaging gastrointestinal stromal tumors. Cancer Control 2005;12(2):111–115.
Lerut T, Flamen P, Ectors N, et al. Histopathologic validation of lymph node staging with FDG-PET scan in cancer of the esophagus and gastroesophageal junction: a prospective study based on primary surgery with extensive lymphadenectomy. Ann Surg 2000;232(6):743–752.
Goerres GW, Stupp R, Barghouth G, et al. The value of PET, CT and in-line PET/CT in patients with gastrointestinal stromal tumours: long-term outcome of treatment with imatinib mesylate. Eur J Nucl Med Mol Imaging 2005;32(2):153–162.
Antoch G, Kanja J, Bauer S, et al. Comparison of PET, CT, and dual-modality PET/CT imaging for monitoring of imatinib (STI571) therapy in patients with gastrointestinal stromal tumors. J Nucl Med 2004;45(3):357–365.
Cerfolio RJ, Ojha B, Bryant AS, Raghuveer V, Mountz JM, Bartolucci AA. The accuracy of integrated PET-CT compared with dedicated PET alone for the staging of patients with nonsmall cell lung cancer. Ann Thorac Surg 2004;78(3):1017–1023.
Cerfolio RJ, Bryant AS, Ohja B, Bartolucci AA, Eloubeidi MA. The accuracy of endoscopic ultrasonography with fine-needle aspiration, integrated positron emission tomography with computed tomography, and computed tomography in restaging patients with esophageal cancer after neoadjuvant chemoradiotherapy. J Thorac Cardiovasc Surg 2005;129(6):1232–1241.
Francois Y, Nemoz CJ, Baulieux J, et al. Influence of the interval between preoperative radiation therapy and surgery on downstaging and on the rate of sphincter-sparing surgery for rectal cancer: the Lyon R90-01 randomized trial. J Clin Oncol 1999;17(8):2396–2402.
Rengan R, Paty PB, Wong WD, et al. Ten-year results of preoperative radiation followed by sphincter preservation for rectal cancer: increased local failure rate in nonresponders. Clin Colorectal Cancer 2006;5(6):413–421.
Pachler J, Wille-Jorgensen P. Quality of life after rectal resection for cancer, with or without permanent colostomy. Cochrane Database Syst Rev 2005(2):CD004323.
Engel J, Kerr J, Schlesinger-Raab A, Eckel R, Sauer H, Holzel D. Quality of life in rectal cancer patients: a four-year prospective study. Ann Surg 2003;238(2):203–213.
Kuzu MA, Topcu O, Ucar K, et al. Effect of sphincter-sacrificing surgery for rectal carcinoma on quality of life in Muslim patients. Dis Colon Rectum 2002;45(10):1359–1366.
Camilleri-Brennan J, Steele RJ. Objective assessment of morbidity and quality of life after surgery for low rectal cancer. Colorectal Dis 2002;4(1):61–66.
Habr-Gama A, Perez RO, Nadalin W, et al. Operative versus nonoperative treatment for stage 0 distal rectal cancer following chemoradiation therapy: long-term results. Ann Surg 2004;240(4):711–717; Discussion 7–8.
Habr-Gama A, Perez RO, Nadalin W, et al. Long-term results of preoperative chemoradiation for distal rectal cancer correlation between final stage and survival. J Gastrointest Surg 2005;9(1):90–99; Discussion 9–101.
Acknowledgments
The authors thank the surgical and nuclear medicine house staff and the nurses of The Johns Hopkins Hospital for their skill and devotion and David Chang, PhD for his assistance with statistics.
Author information
Authors and Affiliations
Corresponding author
Additional information
DISCUSSION
Dr. M. Dayton (Buffalo, NY): That was a very nice presentation, Dr. Melton. I would like to thank the authors for the opportunity to review the manuscript in advance of the meeting.
Dr. Melton and her colleagues have conducted this study to ascertain the value of PET–CT in assessing the response of rectal cancer to neoadjuvant therapy. Most of us in the recent past have used PET–CT or PET scans to assess patients for recurrence or metastatic disease. That has been its major application for the majority of surgery. This work represents a possible new use of PET–CT, particularly if it is found to accurately predict downstaging, complete response, and nodal status. The results of your study seem to suggest that it does that at least in two of the three categories, downstaging and complete response. It probably isn’t quite as good in predicting nodal status. The study also seems to corroborate a previous study from your group that found that 27% of the time using this modality changes the strategic plan for therapy. An example might be downstaging an APR to a sphincter–sparing operation. This technique does have the potential to impact our management of rectal cancer, and I applaud the authors for conducting the study.
Just a couple of questions and maybe a minor criticism of the design. First, the PET–CT scan obtained post–neoadjuvant therapy was done four to six weeks post–operation, but surgery wasn’t done for four weeks beyond that. Why not get the PET–CT scan 8 to 10 weeks post–treatment instead of 4 to 6? It seems like it might more accurately predict the impact of the neoadjuvant therapy.
Second, I noticed in the manuscript that there were multiple, different chemotherapy regimens. Some patients just received 5–FU or capecitabine, others got 5–FU, leucovarin, and oxaliplatin. In a small study like this in which there are multiple regimens, it seems that that would muddy the waters quite a bit. The authors ought to either have a larger N or limit the study to one regimen. Similarly, it seems that patients who had radiation only or chemo only ought to be eliminated from your study group.
Third, was there any difference in response to neoadjuvant therapy based on the level of the rectal cancer? It might be a little bit early to predict that.
And finally, 67% of the patients responded to neoadjuvant therapy. Is it your experience that those that don’t respond at all have a poorer prognosis?
Again, I very much enjoyed the paper. I think it outlines a possible new use for PET CT scanning in rectal cancer.
Dr. Melton: Dr. Dayton, thank you for reviewing our manuscript and also for your insightful comments and questions.
The first question was specifically about the timing of the FDG–PET–CT scans. There are studies in the radiation oncology literature that you get maximal tumor shrinkage all the way out to 12 weeks. Therefore, one could argue that you could do it later, and that may be helpful for surgery planning. We believe that not only is four to six weeks a reasonable time to repeat the FDG–PET/CT but also repeating it earlier may be helpful for other parts of treatment planning. For example, if a FDG–PET–CT scan is completed a few weeks into a regimen, at that point, depending on the results of the scan you might be able to actually alter the neoadjuvant regimen. There is some evidence in the nuclear medicine literature that doing the scan earlier actually may be better. Both rationales make sense. The protocol that we have been using is the four to six weeks, and that I think is partially historical where tumor downstaging and tumor response was found to be maximized in some studies early on at about six weeks.
The next question was about different neoadjuvant regimens, specifically chemotherapeutic regimens, that patients were on. The authors acknowledge that this is a limitation of the study. I think this study can be strengthed if we conduct a follow-up study on a prospective basis and actually validate these measures. Another way to make the cleanest study would be, as you are saying, to make it a single regimen to take out those confounders.
The third question was about level of tumor and differences in response, and we did not see any difference in response according to the level of tumor.
The final question was about prognosis with the nonresponders, and we don’t actually have that data. We do know that those that do not respond generally don’t do as well and that the two strongest markers for having better long–term disease–free and overall survival are going to be lymph node status and having a complete pathological response.
Rights and permissions
About this article
Cite this article
Melton, G.B., Lavely, W.C., Jacene, H.A. et al. Efficacy of Preoperative Combined 18-Fluorodeoxyglucose Positron Emission Tomography and Computed Tomography for Assessing Primary Rectal Cancer Response to Neoadjuvant Therapy. J Gastrointest Surg 11, 961–969 (2007). https://doi.org/10.1007/s11605-007-0170-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11605-007-0170-7