Abstract
Introduction
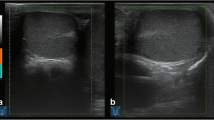
The power Doppler is a useful tool in the evaluation of pediatric acute scrotal pain. Nonetheless, it may have some inherent limitations in scrotal vascularization analysis, potentially causing unnecessary surgery. The microvascular imaging ultrasound (MicroV) is an innovative Doppler technique able to improve the detection of very low flow. This retrospective study aims to compare both power Doppler and MicroV in the evaluation of a pediatric population with early-stage scrotal pain onset, first in testis vascularization analysis, and second in their diagnostic performances.
Materials and methods
69 patients met the following inclusion criteria, age < 18-year-old, a clinical diagnosis of acute scrotal disease, pain onset ≤ 6 h, ultrasound examination (including B-mode, power Doppler, and MicroV), 3-months follow-up. For both power Doppler and MicroV, through a defined vascularization scale, it was evaluated the agreement in vascularization detection, and the sensitivity and specificity in US diagnostic abilities.
Results
Retrospective diagnoses were of 8 testicular torsion, 15 orchi-epididymitis, and 46 children with other scrotal conditions. Power Doppler provided inconclusive US evaluation in 37.68% of the cases, while MicroV only in the 1.45% (p < 0.0001). Testicular torsion and orchi-epididymitis were identified, respectively, with MicroV in 100% (sensitivity, specificity, PPV, NPV, and accuracy of 100%) and 80% of patients (80% sensitivity, 100% specificity and PPV, 94.73% NPV, 95.65% accuracy); with power Doppler the identification was, respectively, of 87.5% (87.5% sensitivity, 100% specificity and PPV, 98.38% NPV and accuracy) and of 73.3% (73.33% sensitivity, 98.14% specificity, 91.66% PPV, 92.98% NPV, 92.75% accuracy).
Conclusions
Our findings indicate that MicroV is a reliable technique in vascularization detection of pediatric testes, being able also to detect vascularization in healthy testicles with no-flow at power Doppler examination. Moreover, MicroV could be a valuable ally in the US diagnostic of children with early-stage scrotal pain onset.





Similar content being viewed by others
References
Sharp VJ, Kieran K, Arlen AM. Testicular torsion: diagnosis, evaluation, and management. Am Fam Physician. 2013;88(12):835–40.
Mohammed WM, Davis NF, O’Connor KM, Kiely EA. Re-evaluating the role of Doppler ultrasonography in patients presenting with scrotal pain. Ir J Med Sci. 2016;185(3):705–9.
Abbas TO, Abdelkareem M, Alhadi A, Kini V, Chandra P, Al-Ansari A, et al. Suspected testicular torsion in children: diagnostic dilemma and recommendation for a lower threshold for initiation of surgical exploration. Res Rep Urol. 2018;10:241–9.
Laher A, Ragavan S, Mehta P, Adam A. Testicular torsion in the emergency room: a review of detection and management strategies. Open Access Emerg Med. 2020;12:237–46.
Sanelli PC, Burke BJ, Lee L. Color and spectral Doppler sonography of partial torsion of the spermatic cord. AJR Am J Roentgenol. 1999;172(1):49–51.
Vijayaraghavan SB. Sonographic differential diagnosis of acute scrotum: real-time whirlpool sign, a key sign of torsion. J Ultrasound Med. 2006;25(5):563–74.
McDowall J, Adam A, Gerber L, Enyuma COA, Aigbodion SJ, Buchanan S, et al. The ultrasonographic “whirlpool sign” in testicular torsion: valuable tool or waste of valuable time? A systematic review and meta-analysis. Emerg Radiol. 2018;25(3):281–92.
Sparano A, Acampora C, Scaglione M, Romano L. Using color power Doppler ultrasound imaging to diagnose the acute scrotum. A pictorial essay Emerg Radiol. 2008;15(5):289–94.
Blaivas M, Brannam L. Testicular ultrasound. Emerg Med Clin North Am. 2004;22(3):723–48.
Stehr M, Boehm R. Critical validation of colour Doppler ultrasound in diagnostics of acute scrotum in children. Eur J Pediatr Surg. 2003;13(6):386–92.
Prando D. Torsion of the spermatic cord: the main gray-scale and Doppler sonographic signs. Abdom Imaging. 2009;34(5):648–61.
Nason GJ, Tareen F, McLoughlin D, McDowell D, Cianci F, Mortell A. Scrotal exploration for acute scrotal pain: a 10-year experience in two tertiary referral paediatric units. Scand J Urol. 2013;47(5):418–22.
Altinkilic B, Pilatz A, Weidner W. Detection of normal intratesticular perfusion using color coded duplex sonography obviates need for scrotal exploration in patients with suspected testicular torsion. J Urol. 2013;189(5):1853–8.
Lam WW, Yap TL, Jacobsen AS, Teo HJ. Colour Doppler ultrasonography replacing surgical exploration for acute scrotum: myth or reality? Pediatr Radiol. 2005;35(6):597–600.
Ota K, Fukui K, Oba K, Shimoda A, Oka M, Ota K, Sakaue M, Takasu A, et al. The role of ultrasound imaging in adult patients with testicular torsion: a systematic review and meta-analysis. J Med Ultrason. 2001;2019(46):325–34.
Burud IAS, Alsagoff SMI, Ganesin R, Selvam ST, Zakaria NAB, Tata MD. Correlation of ultrasonography and surgical outcome in patients with testicular torsion. Pan Afr Med J. 2020;36:45. https://doi.org/10.11604/pamj.2020.36.45.21824.
Aso C, Enríquez G, Fité M, Torán N, Piró C, Piqueras J, et al. Gray-scale and color Doppler sonography of scrotal disorder in children: an update. Radiographics. 2005;25:1197–214.
Kitami M. Ultrasonography of pediatric urogenital emergencies: review of classic and new techniques. Ultrasonography. 2017;36:222–38.
Barth RA, Shortliffe LD. Normal pediatric testis: comparison of power Doppler and color Doppler US in the detection of blood flow. Radiology. 1997;204:389–93.
D’Andrea A, Coppolino F, Cesarano E, Russo A, Cappabianca S, Genovese EA, et al. US in the assessment of acute scrotum. Crit Ultrasound J. 2013. https://doi.org/10.1186/2036-7902-5-S1-S8.
Malferrari G, Pulito G, Pizzini AM, Carraro N, Meneghetti G, Sanzaro E, et al. MicroV technology to improve transcranial color coded doppler examinations. J Neuroimaging. 2018;28(4):350–8.
Visalli C, Mormina E, Tessitore A, Impellizzeri P, Arena S, Genitori F, et al. Acute scrotal pain in pediatric patients: diagnosis with an innovative Doppler technique (MicroV). Emerg Radiol. 2021;28(1):209–14.
Artul S, Nseir W, Armaly Z, Soudack M. Superb microvascular imaging: added value and novel applications. J Clin Imaging Sci. 2017;7:45. https://doi.org/10.4103/jcis.JCIS_79_17.
Van Swieten J, Koudstaal P, Visser M, Schouten H, Van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke. 1988;19(5):604–7.
Liang T, Metcalfe P, Sevcik W, Noga M. Retrospective review of diagnosis and treatment in children presenting to the pediatric department with acute scrotum. AJR Am J Roentgenol. 2013;200:W444-449.
Romeo C, Impellizzeri P, Arrigo T, Antonuccio P, Valenzise M, Mirabelli S, et al. Late hormonal function after testicular torsion. J Pediatr Surg. 2010;45(2):411–3.
Ellati RT, Kavoussi PK, Turner TT, Lysiak JJ. Twist and shout: a clinical and experimental review of testicular torsion. Korean J Urol. 2009;50:1159–67.
Ingram S, Hollman AS. Colour Doppler sonography of the normal paediatric testis. Clin Radiol. 1994;49:266–7.
Albrecht T, Lotzof K, Hussain HK, Shedden D, Cosgrove DO, de Bruyn R. Power Doppler US of the normal prepubertal testis: does it live up to its promises? Radiology. 1997;203:227–31.
Lee YS, Kim MJ, Han SW, Lee HS, Im YJ, Shin HJ, et al. Superb microvascular imaging for the detection of parenchymal perfusion in normal and undescended testes in young children. Eur J Radiol. 2016;85:649–56.
McAdams CR, Del Gaizo AJ. The utility of scrotal ultrasonography in the emergent setting: beyond epididymitis versus torsion. Emerg Radiol. 2018;25(4):341–8.
Yoo J, Je BK, Choo JY. Ultrasonographic demonstration of the tissue microvasculature in children: microvascular ultrasonography versus conventional color doppler ultrasonography. Korean J Radiol. 2020;21(2):146–58.
Martinoli C, Pretolesi F, Crespi G, Bianchi S, Gandolfo N, Valle M, et al. Power Doppler sonography: clinical applications. Eur J Radiol. 1998;27(Suppl 2):S133–40.
Ayaz E, Ayaz M, Önal C, Yıkılmaz A. Seeing the unseen: evaluating testicular vascularity in neonates by using the superb microvascular imaging ultrasound technique. J Ultrasound Med. 2019;38:1847–54.
Keçeli M, Keskin Z, Keskin S. Comparison of superb microvascular imaging with other doppler methods in assessment of testicular vascularity in cryptorchidism. Ultrasound Q. 2020;36(4):363–70.
Karaca L, Oral A, Kantarci M, Sade R, Ogul H, Bayraktutan U, et al. Comparison of the superb microvascular imaging technique and the color Doppler techniques for evaluating children’s testicular blood flow. Eur Rev Med Pharmacol Sci. 2016;20:1947–53.
Durmaz MS, Sivri M. Comparison of superb micro-vascular imaging (SMI) and conventional Doppler imaging techniques for evaluating testicular blood flow. J Med Ultrason. 2001;2018(45):443–52.
Alis D, Erol BC, Akbas S, Barut K, Kasapcopur O, Adaletli I. Superb microvascular imaging compared with power doppler ultrasound in assessing synovitis of the knee in juvenile idiopathic arthritis: a preliminary study. J Ultrasound Med. 2020;39(1):99–106.
Gitto S, Messina C, Chianca V, Tuscano B, Lazzara A, Corazza A, et al. Superb microvascular imaging (SMI) in the evaluation of musculoskeletal disorders: a systematic review. Radiol Med. 2020;125(5):481–90.
Diao X, Zhan J, Chen L, Chen Y, Cao H. Role of superb microvascular imaging in differentiating between malignant and benign solid breast masses. Clin Breast Cancer. 2020;20(6):e786–93. https://doi.org/10.1016/j.clbc.2020.06.009.
Lemini R, Guanà R, Tommasoni N, Mussa A, Di Rosa G, Schleef J. Predictivity of clinical findings and doppler ultrasound in pediatric acute scrotum. Urol J. 2016;13(4):2779–83.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
This retrospective study was approved by the local Institutional Review Board with a waiver for written informed consent. All procedures performed in our study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Visalli, C., Vinci, S.L., Mondello, S. et al. Microvascular imaging ultrasound (MicroV) and power Doppler vascularization analysis in a pediatric population with early scrotal pain onset. Jpn J Radiol 40, 192–201 (2022). https://doi.org/10.1007/s11604-021-01194-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11604-021-01194-6