Abstract
Objective
Cardiopulmonary resuscitation (CPR) after cardiac arrest (CA) is one of the main causes of capillary leakage syndrome (CLS). This study aimed to establish a stable CLS model following the CA and cardiopulmonary resuscitation (CA-CPR) model in Sprague-Dawley (SD) rats.
Methods
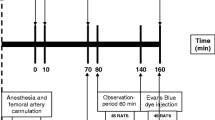
We conducted a prospective, randomized, animal model study. All adult male SD rats were randomly divided into a normal group (group N), a sham operation group (group S), and a cardiopulmonary resuscitation group (group T). The SD rats of the three groups were all inserted with 24-G needles through their left femoral arteries and right femoral veins. In group S and group T, the endotracheal tube was intubated. In group T, CA induced by asphyxia (AACA) was caused by vecuronium bromide with the endotracheal tube obstructed for 8 min, and the rats were resuscitated with manual chest compression and mechanical ventilation. Preresuscitation and postresuscitation measurements, including basic vital signs (BVS), blood gas analysis (BG), routine complete blood count (CBC), wet-to-dry ratio of tissues (W/D), and the HE staining results after 6 h were evaluated.
Results
In group T, the success rate of the CA-CPR model was 60% (18/30), and CLS occurred in 26.6% (8/30) of the rats. There were no significant differences in the baseline characteristics, including BVS, BG, and CBC, among the three groups (P>0.05). Compared with pre-asphyxia, there were significant differences in BVS, CBC, and BG, including temperature, oxygen saturation (SpO2), mean arterial pressure (MAP), central venous pressure (CVP), white blood cell count (WBC), hemoglobin, hematocrit, pH, pCO2, pO2, SO2, lactate (Lac), base excess (BE), and Na+ (P<0.05) after the return of spontaneous circulation (ROSC) in group T. At 6 h after ROSC in group T and at 6 h after surgery in groups N and S, there were significant differences in temperature, heart rate (HR), respiratory rate (RR), SpO2, MAP, CVP, WBC, pH, pCO2, Na+, and K+ among the three groups (P<0.05). Compared with the other two groups, the rats in group T showed a significantly increased W/D weight ratio (P<0.05). The HE-stained sections showed consistent severe lesions in the lung, small intestine, and brain tissues of the rats at 6 h after ROSC following AACA.
Conclusion
The CA-CPR model in SD rats induced by asphyxia could reproduce CLS with good stability and reproducibility.
Similar content being viewed by others
References
Cooper JA, Cooper JD, Cooper JM. Cardiopulmonary resuscitation: history, current practice, and future direction. Circulation, 2006,114(25):2839–2849
Reis AG, Nadkarni V, Perondi MB, et al. A prospective investigation into the epidemiology of in-hospital pediatric cardiopulmonary resuscitation using the international Utstein reporting style. Pediatrics, 2002,109(2):200–209
Fink EL, Prince DK, Kaltman JR, et al. Unchanged pediatric out-of-hospital cardiac arrest incidence and survival rates with regional variation in North America. Resuscitation, 2016,107:121–128
Berdowski J, Berg RA, Tijssen JG, et al. Global incidences of out-of-hospital cardiac arrest and survival rates: Systematic review of 67 prospective studies. Resuscitation, 2010,81(11):1479–1487
Gräsner JT, Lefering R, Koster RW, et al. EuReCa ONE-27 Nations, ONE Europe, ONE Registry: A prospective one month analysis of out-of-hospital cardiac arrest outcomes in 27 countries in Europe. Resuscitation, 2016,105:188–195
Ong ME, Shin SD, De Souza NN, et al. Outcomes for out-of-hospital cardiac arrests across 7 countries in Asia: The Pan Asian Resuscitation Outcomes Study (PAROS). Resuscitation, 2015,96:100–108
Tress EE, Clark RS, Foley LM, et al. Blood brain barrier is impermeable to solutes and permeable to water after experimental pediatric cardiac arrest. Neurosci Lett, 2014,578:17–21
Ibáñez B, Heusch G, Ovize M, et al. Evolving therapies for myocardial ischemia/reperfusion injury. J Am Coll Cardiol, 2015,65(14):1454–1471
de Perrot M, Liu M, Waddell TK, et al. Ischemia-reperfusion-induced lung injury. Am J Respir Crit Care Med, 2003,167(4):490–511
Druey KM, Greipp PR. Narrative review: the systemic capillary leak syndrome. Ann Int Med, 2010,153(2):90–98
Bateman RM, Sharpe MD, Jagger JE, et al. 36th International Symposium on Intensive Care and Emergency Medicine: Brussels, Belgium. 15–18 March 2016. Crit Care, 2016,20(Suppl 2):94
Liu X, Wang G, Sun L, et al. The case report of capillary leakage syndrome secondary to malignant hypertension. Medicine (Baltimore), 2018,97(34):e11913
Liu Z, Li de C, Zhu YP. Interleukin-11-induced capillary leak syndrome companied with abdominal chylous leakage in primary sigmoid carcinoma patients with thrombocytopenia. J Cancer Res Ther, 2015,11(4):1024
Nong WX, Lv QJ, Lu YS. Veno-venous-extracorporeal membrane oxygenation treatment for severe capillary leakage syndrome: A case report. World J Clin Cases, 2021,9(33):10273–10278
Kamohara T, Weil MH, Tang W, et al. A comparison of myocardial function after primary cardiac and primary asphyxial cardiac arrest. Am J Respir Crit Care Med, 2001,164(7):1221–1224
Drabek T, Foley LM, Janata A, et al. Global and regional differences in cerebral blood flow after asphyxial versus ventricular fibrillation cardiac arrest in rats using ASL-MRI. Resuscitation, 2014,85(7):964–971
Aravamuthan BR, Shoykhet M. Long-term increase in coherence between the basal ganglia and motor cortex after asphyxial cardiac arrest and resuscitation in developing rats. Pediatr Res, 2015,78(4):371–379
Sharma HS, Miclescu A, Wiklund L. Cardiac arrest-induced regional blood-brain barrier breakdown, edema formation and brain pathology: a light and electron microscopic study on a new model for neurodegeneration and neuroprotection in porcine brain. J Neural Transm (Vienna), 2011,118(1):87–114
Geng Y, Li E, Mu Q, et al. Hydrogen sulfide inhalation decreases early blood-brain barrier permeability and brain edema induced by cardiac arrest and resuscitation. J Cereb Blood Flow Metab, 2015,35(3):494–500
Marx G, Vangerow B, Burczyk C, et al. Evaluation of noninvasive determinants for capillary leakage syndrome in septic shock patients. Intensive Care Med, 2000,26(9):1252–1258
Wollborn J, Hassenzahl LO, Reker D, et al. Diagnosing capillary leak in critically ill patients: development of an innovative scoring instrument for non-invasive detection. Ann Intensive Care, 2021,11(1):175
Kubicki R, Grohmann J, Siepe M, et al. Early prediction of capillary leak syndrome in infants after cardiopulmonary bypass. Eur J Cardiothorac Surg, 2013,44(2):275–281
Heradstveit BE, Guttormsen AB, Langørgen J, et al. Capillary leakage in post-cardiac arrest survivors during therapeutic hypothermia — a prospective, randomised study. Scand J Trauma Resusc Emerg Med, 2010,18:29
Hammersborg SM, Brekke HK, Haugen O, et al. Surface cooling versus core cooling: comparative studies of microvascular fluid- and protein-shifts in a porcine model. Resuscitation, 2008,79(2):292–300
Farstad M, Haugen O, Kvalheim VL, et al. Reduced fluid gain during cardiopulmonary bypass in piglets using a continuous infusion of a hyperosmolar/hyperoncotic solution. Acta Anaesthesiol Scand, 2006,50(7):855–862
Farstad M, Heltne JK, Rynning SE, et al. Can the use of methylprednisolone, vitamin C, or alpha-trinositol prevent cold-induced fluid extravasation during cardiopulmonary bypass in piglets? J Thorac Cardiovasc Surg, 2004,127(2):525–534
Nordmark J, Johansson J, Sandberg D, et al. Assessment of intravascular volume by transthoracic echocardiography during therapeutic hypothermia and rewarming in cardiac arrest survivors. Resuscitation, 2009,80(11):1234–1239
Geppert A, Zorn G, Karth GD, et al. Soluble selectins and the systemic inflammatory response syndrome after successful cardiopulmonary resuscitation. Crit Care Med, 2000,28(7):2360–2365
Zhou ZG, Chen YD, Sun W, et al. Pancreatic microcirculatory impairment in experimental acute pancreatitis in rats. World J Gastroenterol, 2002,8(5): 933–936
Schick MA, Wunder C, Wollborn J, et al. Phosphodiesterase-4 inhibition as a therapeutic approach to treat capillary leakage in systemic inflammation. J Physiol, 2012,590(11):2693–2708
Wollborn J, Siemering S, Steiger C, et al. Phosphodiesterase-4 inhibition reduces ECLS-induced vascular permeability and improves microcirculation in a rodent model of extracorporeal resuscitation. Am J Physiol Heart Circ Physiol, 2019,316(3):H751–H761
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that they have no conflicts of interest.
Rights and permissions
About this article
Cite this article
Zhang, Xl., Cheng, Y., Xing, Cl. et al. Establishment of a Rat Model of Capillary Leakage Syndrome Induced by Cardiopulmonary Resuscitation After Cardiac Arrest. CURR MED SCI 43, 708–715 (2023). https://doi.org/10.1007/s11596-023-2695-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-023-2695-8