Abstract
Objective
This study aimed to investigate the correlation between the surface area ratio of medial tibial plateau (MTP) to lateral tibial plateau (LTP) and the mechanical tibiofemoral angle (mTFA).
Methods
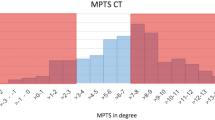
Lower limb computed tomography (CT) images were collected at our hospital. Then, the original CT data were analyzed and reconstructed using medical image processing software. The proximal and distal centres of the femur and tibia were marked. The surface areas of MTP and LTP were identified using image processing software. GraphPad Prism 8.0.2 was used to perform the statistical analysis.
Results
The surface area ratio of MTP to LTP was significantly correlated with the mTFA in all patients (P<0.0001), male group (P<0.0001), female group (P<0.0001), varus group (P<0.0001), and valgus group (P=0.002). Furthermore, the surface area of MTP and LTP was significantly greater in the male group than in the female group (P<0.0001). There was significant difference in the surface area of the MTP between the varus and valgus groups (P<0.0001). Significant difference was also observed in the surface area ratio of MTP to LTP between the varus and valgus groups (P<0.0001).
Conclusion
The surface area ratio of MTP to LTP was correlated with the mTFA. Within a certain range, the smaller the mTFA, the greater the surface area ratio of MTP to LTP. For patients undergoing total knee arthroplasty, of whom the surface area of the MTP was basically equal to that of the LTP, it is recommended that the osteotomy should be performed in accordance with mechanical alignment standards, and that a symmetrical tibial plateau prosthesis should be used. For patients whose surface area of MTP is significantly greater than that of the LTP, it is recommended that the osteotomy should be performed in accordance with kinematic alignment standards, and that an anatomical tibial plateau prosthesis should be used.
Similar content being viewed by others
References
Flandry F, Hommel G. Normal anatomy and biomechanics of the knee. Sports Med Arthrosc Rev, 2011,19(2):82–92
Zhang Y, Chen Y, Qiang M, et al. Morphometry of the Tibial Plateau at the Surface and Resected Levels. J Arthroplasty, 2017,32(8):2563–2567
Dong XH, Huang XH, Chen M, et al. Three-dimensional morphometric differences of resected distal femurs and proximal tibias in osteoarthritic and normal knees. BMC Musculoskelet Disord, 2021,22(1):1013
Erkocak OF, Kucukdurmaz F, Sayar S, et al. Anthropometric measurements of tibial plateau and correlation with the current tibial implants. Knee Surg Sports Traumatol Arthrosc, 2016,24(9):2990–2997
Hsu RW, Himeno S, Coventry MB, et al. Normal Axial Alignment of the Lower Extremity and Load-Bearing Distribution at the Knee. Clin Orthop Relat Res, 1990, (255):215–227
Moreland JR, Bassett LW, Hanker GJ. Radiographic analysis of the axial alignment of the lower extremity. J Bone Joint Surg Am, 1987,69(5):745–749
Tang WM, Zhu YH, Chiu KY. Axial alignment of the lower extremity in Chinese adults. J Bone Joint Surg Am, 2000,82(11):1603–1608
Victor JM, Bassens D, Bellemans J, et al. Constitutional Varus Does Not Affect Joint Line Orientation in the Coronal Plane. Clin Orthop Relat Res, 2014,472(1):98–104
Mandl LA. Osteoarthritis year in review 2018: clinical. Osteoarthritis Cartilage, 2019,27(3):359–364
Price AJ, Alvand A, Troelsen A, et al. Knee replacement. Lancet, 2018,392(10158):1672–1682
Shan L, Shan B, Suzuki A, et al. Intermediate and Long-Term Quality of Life After Total Knee Replacement: A Systematic Review and Meta-Analysis. J Bone Joint Surg Am, 2015,97(2):156–168
Dai Y, Scuderi GR, Bischoff JE, et al. Anatomic tibial component design can increase tibial coverage and rotational alignment accuracy: a comparison of six contemporary designs. Knee Surg Sports Traumatol Arthrosc, 2014,22(12):2911–2923
Jin C, Song EK, Prakash J, et al. How Much Does the Anatomical Tibial Component Improve the Bony Coverage in Total Knee Arthroplasty? J Arthroplasty, 2017,32(6):1829–1833
Schiraldi M, Bonzanini G, Chirillo D, et al. Mechanical and kinematic alignment in total knee arthroplasty. Ann Transl Med, 2016,4(7):130
Lee YS, Howell SM, Won YY, et al. Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc, 2017,25(11):3467–3479
Rivière C, Iranpour F, Auvinet E, et al. Alignment options for total knee arthroplasty: A systematic review. Orthop Traumatol Surg Res, 2017,103(7):1047–1056
Agha R, Abdall-Razak A, Crossley E, et al. The STROCSS 2019 Guideline: Strengthening the Reporting of Cohort Studies in Surgery. Int J Surg, 2019,72:156–165
Fürmetz J, Sass J, Ferreira T, et al. Three-dimensional assessment of lower limb alignment: accuracy and reliability. Knee, 2019,26(1):185–193
Asada S, Mori S, Inoue S, et al. Location of the ankle center for total knee arthroplasty. Knee, 2017,24(1):121–127
Sikorski JM. Alignment in total knee replacement. J Bone Joint Surg Br, 2008,90:1121–1127
Victor J, Dujardin J, Vandenneucker H, et al. Patient-specific guides do not improve accuracy in total knee arthroplasty: a prospective randomized controlled trial. Clin Orthop Relat Res, 2014,472(1):263–271
Vide J, Freitas TP, Ramos A, et al. Patient-specific instrumentation in total knee arthroplasty: simpler, faster and more accurate than standard instrumentation—a randomized controlled trial. Knee Surg Sports Traumatol Arthrosc, 2017,25(8):2616–2621
Ma Y, Mizu-Uchi H, Okazaki K, et al. Effects of tibial baseplate shape on rotational alignment in total knee arthroplasty: three-dimensional surgical simulation using osteoarthritis knees. Arch Orthop Trauma Surg, 2018,138(1):105–114
Bagaria V, Bhansali R, Pawar P. 3D printing- creating a blueprint for the future of orthopedics: Current concept review and the road ahead! J Clin Orthop Trauma, 2018,9(3):207–212
Heller M, Bauer HK, Goetze E, et al. Applications of patient-specific 3D printing in medicine. Int J Comput Dent, 2016,19(4):323–339
König IR, Fuchs O, Hansen G, et al. What is precision medicine? Eur Respir J, 2017,50(4):1700391
Calliess T, Bauer K, Stukenborg-Colsman C, et al. PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc, 2017, 25(6):1743–1748
Courtney PM, Lee GC. Early Outcomes of Kinematic Alignment in Primary Total Knee Arthroplasty: A Meta-Analysis of the Literature. J Arthroplasty, 2017,32(6):2028–2032.e1
Luo Z, Zhou K, Peng L, et al. Similar results with kinematic and mechanical alignment applied in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc, 2020,28(6):1720–1735
Author information
Authors and Affiliations
Corresponding authors
Additional information
Conflict of Interest Statement
All authors declare that they have no conflict of interest.
This work was supported by the National Natural Science Foundation of China (No. 81672155).
Rights and permissions
About this article
Cite this article
Gong, S., Han, Lz., Gong, Tl. et al. Correlation between Surface Area Ratio of Medial to Lateral Tibial Plateau and Knee Alignment in Adults. CURR MED SCI 42, 577–583 (2022). https://doi.org/10.1007/s11596-022-2590-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-022-2590-8