Abstract
Objective
The clinical characteristics and microbiological data of patients with K. pneumoniae bloodstream infections (BSI) from January 2018 to December 2020 were retrospectively analyzed to study the molecular epidemiology of Carbapenem-resistant Klebsiella pneumoniae (CRKP). We also aimed to identify the risk factors for the development of CRKP BSI.
Methods
This retrospective study was conducted at Renmin Hospital of Wuhan University from January 2018 to December 2020. The date of non-duplicate K. pneumoniae isolates isolated from blood samples was identified using the microbiology laboratory database. The data from patients diagnosed with K. pneumoniae BSI were collected and analyzed.
Results
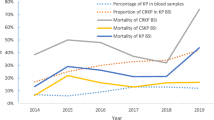
From 2018 to 2020, there were 510 non-duplicated K. pneumoniae blood isolates, mainly distributed in the intensive care unit (ICU) (28.4%), that were identified in our research. These cases included 77 strains of CRKP and 433 strains of carbapenem-susceptible K. pneumoniae (CSKP). The resistance rate of K. pneumoniae to meropenem and imipenem increased from 11.2% in 2018 to 27.1% in 2020. Moreover, Compared with CSKP, all CRKP isolates showed multi-resistance to tested antibiotics. The phylogenetic analysis showed that the CRKP isolates could be grouped into four major clades, and multilocus sequence typing revealed that the isolates had considerable clonality. Overall, 8 sequence types (STs) of CRKP were detected, of which ST11 comprised the majority and clustered into clade 3. The most prevalent carbapenemase gene was blaKPC (87%) among the CRKP isolates, followed by blaNDM (9.1%) and blaIMP (1.3%). A total of 74 (16.6%) patients with CRKP BSI and 373 (83.4%) patients with CSKP BSI were categorized as the case and control groups. The mortality in the CRKP group was 44.6%, and 11.5% in CSKP group (P<0.001). A multivariate analysis that a long hospital stay before BSI (OR=1.42, 95% CI 1.02–4.31, P=0.011), ICU hospitalization history (OR=3.30, 95% CI 1.35–8.05, P=0.002), and prior use of carbapenems (OR=3.33, 95% CI 1.29–7.27, P=0.001) and antifungals (OR=2.81, 95% CI 1.24–6.04, P<0.001) were independent risk factors for CRKP BSI.
Conclusion
ST11 is the predominant type of CRKP mediating inter-hospital transmission, and blaKPC is the main carbapenemase gene harboured by CRKP blood isolates. ICU stay, prolonged hospitalization before BSI, and prior use of carbapenems and antifungals were independent risk factors for acquiring CRKP BSI. Our study may provide insights into early infection control practices.
Similar content being viewed by others
References
Pitout JD, Nordmann P, Poirel L. Carbapenemase-Producing Klebsiella pneumoniae, a Key Pathogen Set for Global Nosocomial Dominance. Antimicrob Agents Chemother, 2015,59(10):5873–5884
Russo TA, Marr MC. hypervirulent Klebsiella pneumoniae. Clin Microbiol Rev, 2019, 32(3): e0001–19
Munoz-Price LS, Poirel L, Bonomo RA, et al. Clinical epidemiology of the global expansion of Klebsiella pneumoniae carbapenemases. Lancet Infect Dis, 2013, 13(9):785–796
Girometti N, Lewis RE, Giannella M, et al. Klebsiella pneumoniae bloodstream infection: epidemiology and impact of inappropriate empirical therapy. Medicine (Baltimore), 2014,93(17):298–309
Yang Y, Chen J, Lin D, et al. Prevalence and drug resistance characteristics of carbapenem-resistant Enterobacteriaceae in Hangzhou, China. Front Med, 2018,12(2):182–188
Xu LF, Sun XX, Ma XL. Systematic review and meta-analysis of mortality of patients infected with carbapenem-resistant Klebsiella pneumoniae. Ann Clin Microbiol Antimicrob, 2017,16(1):18
Suay-Garcia B, Perez-Gracia MT. Present and Future of Carbapenem-resistant Enterobacteriaceae (CRE) Infections. Antibiotics (Basel), 2019,8(3):122
Jeon JH, Lee JH, Lee JJ, et al. Structural basis for carbapenem-hydrolyzing mechanisms of carbapenemases conferring antibiotic resistance. Int J Mol Sci, 2015, 16(5):9654–9692
Iredell J, Brown J, Tagg K. Antibiotic resistance in Enterobacteriaceae: mechanisms and clinical implications. BMJ, 2016,352:h6420
Kopotsa K, Sekyere JO, Mbelle NM. Plasmid evolution in carbapenemase-producing Enterobacteriaceae: a review. Ann N Y Acad Sci, 2019,1457(1):61–91
Mohamed ER, Ali MY, Waly NGFM, et al. The Inc FII Plasmid and its Contribution in the Transmission of blaNDM-1 and blaKPC-2 in Klebsiella pneumoniae in Egypt. Antibiotics (Basel), 2019,8(4):266
Lee CR, Lee JH, Park KS, et al. Global Dissemination of Carbapenemase-Producing Klebsiella pneumoniae: Epidemiology, Genetic Context, Treatment Options, and Detection Methods. Front Microbiol, 2016,7:895
Chen L, Mathema B, Chavda KD, et al. Carbapenemase-producing Klebsiella pneumoniae: molecular and genetic decoding. Trends Microbiol, 2014,22(12):686–696
Diancourt L, Passet V, Verhoef J, et al. Multilocus sequence typing of Klebsiella pneumoniae nosocomial isolates. J Clin Microbiol, 2005,43(8):4178–4182
Shao CH, Wang W, Liu S, et al. Molecular Epidemiology and Drug Resistant Mechanism of Carbapenem-Resistant Klebsiella pneumoniae in Elderly Patients With Lower Respiratory Tract Infection. Front Public Health, 2021,9:669173
Tian LJ, Tan RM, Chen Y, et al. Epidemiology of bloodstream infections in a teaching hospital: factors related to the carbapenem resistance and patient mortality. Antimicrob Resist Infect Control, 2016,5:48
Li YY, Li JH, Hu T, et al. Five-year change of prevalence and risk factors for infection and mortality of carbapenem-resistant Klebsiella pneumoniae bloodstream infection in a tertiary hospital in North China. Antimicrob Resist Infect Control, 2020,9(1):79
Zhang SG, Yang ZY, Sun LM, et al. Clinical Observation and Prognostic Analysis of Patients With Klebsiella pneumoniae Bloodstream Infection. Front Cell Infect Microbiol, 2020,10:577244
Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control, 2008,36(5):309–332
Probst K, Boutin S, Bandilla M, et al. Fast and automated detection of common carbapenemase genes using multiplex real-time PCR on the BD MAX™ system. J Microbiol Methods, 2021,185:106224
Diancourt L, Psaaet V, Verhoef J, et al. Multilocus sequence typing of Klebsiella pneumoniae nosocomial isolates. J Clin Microbiol, 2005,43(8):4178–4182
Rose DD, Sordillo P, Gini S, et al. Microbiologic characteristics and predictors of mortality in bloodstream infections in intensive care unit patients: A 1-year, large, prospective surveillance study in 5 Italian hospitals. Am J Infect Control, 2015,43(11):1178–1183
Hu YM, Ping YT, Li LQ, et al. A retrospective study of risk factors for carbapenem-resistant Klebsiella pneumoniae acquisition among ICU patients. J Infect Dev Ctries, 2016,10(3):208–213
Zhang Y, Guo LY, Song WQ, et al. Risk factors for carbapenem-resistant K. pneumoniae bloodstream infection and predictors of mortality in Chinese paediatric patients. BMC Infect Dis, 2018,18(1):248
Zheng X, Wang JF, Xu WL, et al. Clinical and molecular characteristics, risk factors and outcomes of Carbapenem-resistant bloodstream infections in the intensive care unit. Antimicrob Resist Infect Control, 2017,6:102
Zhang SG, Yang ZY, Sun LM, et al. Clinical Observation and Prognostic Analysis of Patients With Klebsiella pneumoniae Bloodstream Infection. Front Cell Infect Microbiol, 2020,10:577244
Viale P, Giannella M, Lewis R, et al. Predictors of mortality in multidrug-resistant Klebsiella pneumoniae bloodstream infections. Expert Rev Anti Infect Ther, 2013,11(10): 1053–1063
Jiao Y, Qin YH, Liu JJ, et al. Risk factors for carbapenem-resistant Klebsiella pneumoniae infection/colonization and predictors of mortality: a retrospective study. Pathog Glob Health, 2015,109(2):68–74
Karam G, Chastre J, Wilcox MH, et al. Antibiotic strategies in the era of multidrug resistance. Crit Care, 2016,20(1):136
Gorrie CL, Mirceta M, Wick RR, et al. Gastrointestinal Carriage Is a Major Reservoir of Klebsiella pneumoniae Infection in Intensive Care Patients. Clin Infect Dis, 2017,65(2): 208–215
Gao H, Liu YD, Wang RB, et al. The transferability and evolution of NDM-1 and KPC-2 co-producing Klebsiella pneumoniae from clinical settings. EBioMedicine, 2020,51:102599
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The authors declare that there are no conflicts of interest.
Rights and permissions
About this article
Cite this article
Liu, C., Liu, L., Jin, Mm. et al. Molecular Epidemiology and Risk Factors of Carbapenem-Resistant Klebsiella Pneumoniae Bloodstream Infections in Wuhan, China. CURR MED SCI 42, 68–76 (2022). https://doi.org/10.1007/s11596-021-2480-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-021-2480-5