Summary
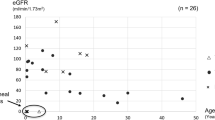
PKHD1 mutations are generally considered to cause autosomal recessive polycystic kidney disease (ARPKD). ARPKD is a rare disorder and one of the most severe conditions leading to end-stage renal disease in childhood. With the biallelic deletion mutation, patients have difficulty in surviving the perinatal period, resulting in perinatal or neonatal death. This study retrospectively analyzed patient characteristics, imaging characteristics, laboratory examinations and family surveys from 7 Chinese children with different PKHD1 gene mutations diagnosed by high-throughput sequencing from January 2014 to February 2018. Of the 7 children, there were 3 males and 4 females. Eight missense mutations, two frameshift mutations, two deletion mutations, and two intronic slicing mutations were identified. Six of the mutations have not previously been identified. In the literature search, we identified a total of 29 Chinese children with PKHD1 mutations. The missense mutation c.2507T>C in exon 24 was found in one patient in our study, and five patients with liver fibrosis but normal renal function were reported in the literature. The missense mutation c.5935G>A in exon 37 was found in two patients in our study and three cases in the literature. Four patients had renal failure at an age as young as 1 year of those five patients with the missense mutation c.5935G>A in exon 37. It was concluded that: (1) Kidney length more than 2–3 SDs above the mean and early-onset hypertension might be associated with PKHD1-associated ARPKD; (2) The more enlarged the kidney size is, the lower the renal function is likely to be; (3) c.5935G>A may be a hot spot that leads to early renal failure in Chinese children with PKHD1 mutations; (4) c.2507T>C may be a hot-spot mutation associated with hepatic lesions in Chinese children with PKHD1.
Similar content being viewed by others
References
Ward CJ, Hogan MC, Rossetti S, et al. The gene mutated in autosomal recessive polycystic kidney disease encodes a large, receptor-like protein. Nat Genet, 2002,30(3):259–269
Onuchic LF, Furu L, Nagasawa Y, et al. PKHD1, the polycystic kidney and hepatic disease 1 gene, encodes a novel large protein containing multiple immunoglobulin-like plexin-transcription-factor domains and parallel beta-helix 1 repeats. Am J Hum Genet, 2002,70(5):1305–1317
Buscher R, Buscher AK, Weber S, et al. Clinical manifestations of autosomal recessive polycystic kidney disease (ARPKD): kidney-related and non-kidney-related phenotypes. Pediatr Nephrol, 2014,29(10):1915–1925
Zerres K, Rudnik-Schoneborn S, Steinkamm C, et al. Autosomal recessive polycystic kidney disease. J Mol Med (Berl), 1998,76(5):303–309
Bergmann C, Senderek J, Sedlacek B, et al. Spectrum of mutations in the gene for autosomal recessive polycystic kidney disease (ARPKD/PKHD1). J Am Soc Nephrol, 2003,14(1):76–89
Wehrman A, Kriegermeier A, Wen J. Diagnosis and Management of Hepatobiliary Complications in Autosomal Recessive Polycystic Kidney Disease. Front Pediatr, 2017,5:124
Zhang D, Lu L, Yang HB, et al. Exome sequencing identifies compound heterozygous PKHD1 mutations as a cause of autosomal recessive polycystic kidney disease. Chin Med J (Engl), 2012,125(14):2482–2486
Song HX, Sun CM, Han Z, et al. Detection of PKHD1 gene in autosomal recessive polycystic kidney disease. Chin J Woman Child Health Res (Chinese), 2013,24(4):495–497
Yang XY, Zhu LP, Liu XQ, et al. Genetic diagnosis of Caroli syndrome with autosomal recessive polycystic kidney disease: a case report and literature review. J Peking Univ Health Sci (Chinese), 2018,50(2):335–339
Hao X, Liu S, Dong Q, et al. Whole exome sequencing identifies recessive PKHD1 mutations in a Chinese twin family with Caroli disease. PLoS One, 2014,9(4):e92661
Meng DH, Li Y, Wei QF, et al. Neonatal polycystic kidney disease: a case report and literature review. Zhong Guo Xin Sheng Er Ke Za Zhi (Chinese), 2016,31(5):343–347
Xiang YB, Li HZ, Xu CY, et al. Analysis of PKHD1 gene mutation in a family affected with infantile polycystic kidney disease. Chin J Med Genet, 2016,33(5):662–665
Guo XY, Wang ZH, Liao J, et al. Mutational analysis in PKHD1 gene from a family of infantile polycystic kidney. J Mol Diag Ther, 2012,4(4):227–232
Li GM, Shen Q, Sun L, et al. Phenotype analysis of 9 cases with mutations in PKHD1 gene. Clin J Nephrol, 2017,33(11):831–837
Yan YY, Gong JY, Shi YY, et al. Portal hypertention caused by PKHD1 mutations in childern: 4 cases report. Chin J Evid Based Pediatr, 2016,11(6):455–459
Liu SP, Ding J, Wang F, et al. Clinical characteristics and mutation analysis of three Chinese children with autosomal recessive polycystic kidney disease. World J Pediatr, 2014,10(3):271–274
Chen J, Ma N, Zhao X, et al. A rare deep intronic mutation of PKHD1 gene, c.8798-459 C > A, causes autosomal recessive polycystic kidney disease by pseudoexon activation. J Hum Genet, 2019,64(3):207–214
Zhou XH, Yuan L, Hui ZY, et al. PKHD1 gene analysis in a newborn with autosomal recessive polycystic kidney disease. Chin J Woman Child Health Res (Chinese), 2012,23(1):9–12
Zhang ML, Zhou HH, Lu YP, et al. Application of targeted exome capture in identifying genetic mutations in ciliopathies. Chin J Perinat Med, 2016,19(6):422–426
Zhang JW, Wang C, Wang CY, et al. Gene analysis and literature review of autosomal recessive polycystic kidney disease. Chin J Pediatr, 2013,51(9):684–686
Bitarafan F, Garshasbi M. Molecular Genetic Analysis of PKHD1 Mutations in Pedigrees With Autosomal Recessive Polycystic Kidney Disease. Iran J Kidney Dis, 2018,12(6):350–358
Bergmann C, Senderek J, Windelen E, et al. Clinical consequences of PKHD1 mutations in 164 patients with autosomal-recessive polycystic kidney disease (ARPKD). Kidney Int, 2005,67(3):829–948
Outeda P, Menezes L, Hartung EA, et al. A novel model of autosomal recessive polycystic kidney questions the role of the fibrocystin C-terminus in disease mechanism. Kidney Int, 2017,92(5):1130–1144
Author information
Authors and Affiliations
Corresponding author
Additional information
This project was supported by the National Natural Science Foundation of China (No. 81873596).
Conflict of Interest Statement
The authors have declared no conflicts of interest for this article.
Rights and permissions
About this article
Cite this article
Qiu, Lr., Xu, Rr., Tang, Jh. et al. Possible PKHD1 Hot-spot Mutations Related to Early Kidney Function Failure or Hepatofibrosis in Chinese Children with ARPKD: A Retrospective Single Center Cohort Study and Literature Review. CURR MED SCI 40, 835–844 (2020). https://doi.org/10.1007/s11596-020-2268-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-020-2268-z