Summary
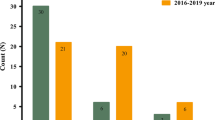
Central nervous system (CNS) infections are associated with high mortality rates. The clinical presentation of many CNS infections by different pathogens is difficult to distinguish, but the definite diagnosis of the etiology is critical for effective therapy and prognosis. The aim of this study was to explore the etiology of CNS infections with definite diagnoses based on data from a clinical microbiology laboratory in Tongji Hospital, a teaching hospital in China, obtained over a six-year period. We conducted a retrospective study on all cerebrospinal fluid (CSF) specimens submitted to our clinical microbiology laboratory from September, 2012 to December, 2018. The etiology of CNS infections caused by Cryptococcus neoformans, Mycobacterium tuberculosis and common bacteria was analyzed. Antimicrobial susceptibility testing was conducted on all isolates. The results showed that 1972 cases of CNS infections were identified from 18 300 CSF specimens. Common bacterial meningitis (BM), cryptococcal meningitis (CM) and tuberculous meningitis (TM) accounted for 86.3% (677/785), 9.4% (74/785) and 4.3% (34/785) respectively of cases over the six-year period. BM was the most common among the different age groups, followed by CM. Of the TM cases, 44.1% (15/34) were distributed within the age group of 15–34 years, whereas for CM cases, 52.7% (39/74) occurred within the 35–54-year age group, and the age distribution of BM cases was fairly even. Among the bacterial pathogens isolated, Staphylococcus epidermidis was the most common, accounting for 12.5% (98/785), followed by Acinetobacter baumannii (ABA) and Staphylococcus aureus (SAU), accounting for 11.8% (93/785) and 7.6% (60/785) respectively. The resistance rates to antibiotics were >75%, with the exception of the resistance rate of ABA to tegafycline, which was <3%. More than 60% of SAU strains displayed resistance to penicillin, oxacillin, ampicillin/sulbactam, cefazolin, cefuroxime, gentamycin, tobramycin, erythromycin and levofloxacin, whereas more than 90% of SAU strains showed susceptibility to trimethoprim/sulfamethoxazole, tegafycline, vancomycin, teicoplanin and linezolid. For C. neoformans, the susceptibility rates to amphotericin B, 5-fluorocytosine, fluconazol and voriconazole were >95%. Analysis of samples from patients with CNS infection in a clinical microbiology laboratory at a teaching hospital in China over a six-year period indicated that the most common etiological agents were the bacteria ABA and SAU. The antibiotic resistance levels of ABA were found to be high and of concern, whereas isolates of C. neoformans were found to be sensitive to antifungal antibiotics.
Similar content being viewed by others
References
He T, Kaplan S, Kamboj M, et al. Laboratory Diagnosis of Central Nervous System Infection. Cur Infect Dis Rep, 2016, 18(11):35
John, CC, Carabin H, Montano, SM, et al. Global research priorities for infections that affect the nervous system. Nature, 2015, 527(7578):S178–S186
Dunbar, SA, Eason, RA, Musher, DM, et al. Microscopic examination and broth culture of cerebrospinal fluid in diagnosis of meningitis. J Clin Microbiol, 1998, 36(6):1617–1620
Polage, CR, Petti, CA. Assessment of the utility of viral culture of cerebrospinal fluid. Clin Infect Dis, 2006, 43(12):1578–1579
Ubukata K. Rapid identification of meningitis due to bacterial pathogens. Rinsho Shinkeigaku (Japanese), 2013, 53(11):1184–1186
van de Beek D, Cabellos C, Dzupova O, et al. ESCMID guideline: diagnosis and treatment of acute bacterial meningitis. Clin Microbiol Infect, 2016, 22(Suppl 3):S37–S62
Glimaker M, Johansson B, Grindborg O, et al. Adult bacterial meningitis: earlier treatment and improved outcome following guideline revision promoting prompt lumbar puncture. Clin Infect Dis, 2015, 60(8):162–1169
Scheld, WM, Koedel U, Nathan B, et al. Pathophysiology of bacterial meningitis: mechanism(s) of neuronal injury. J Infect Dis, 2002, 186(Suppl 2):S225–S233
Adriani, KS, van de Beek D, Brouwer, MC, et al. Community-acquired recurrent bacterial meningitis in adults. Clin Infect Dis, 2007, 45(5):e46–e51
Okike, IO, Ribeiro S, Ramsay, ME, et al. Trends in bacterial, mycobacterial, and fungal meningitis in England and Wales 2004-11: an observational study. Lancet Infect Dis, 2014, 14(4):301–307
Harrison, LH, Trotter, CL, Ramsay, ME. Global epidemiology of meningococcal disease. Vaccine, 2009, 27(Suppl 2):B51–B63
Bijlsma, MW, Brouwer, MC, Kasanmoentalib, ES, et al. Community-acquired bacterial meningitis in adults in the Netherlands, 2006-14: a prospective cohort study. Lancet Infect Dis, 2016, 16(3):339–347
McGill F, Heyderman, RS, Panagiotou S, et al. Acute bacterial meningitis in adults. Lancet, 2016, 388(10063):3036–3047
Martin, NG, Sadarangani M, Pollard, AJ, et al. Hospital admission rates for meningitis and septicaemia caused by Haemophilus influenzae, Neisseria meningitidis, and Streptococcus pneumoniae in children in England over five decades: a population-based observational study. Lancet Infect Dis, 2014, 14(5):397–405
Gray, KJ, Bennett, SL, French N, et al. Invasive group B streptococcal infection in infants, Malawi. Emerg Infect Dis, 2007, 13(2):223–229
Iregbu, KC, Elegba, OY, Babaniyi, IB. Bacteriological profile of neonatal septicaemia in a tertiary hospital in Nigeria. Afr Health Sci, 2006, 6(3):151–154
Kayange N, Kamugisha E, Mwizamholya, DL, et al. Predictors of positive blood culture and deaths among neonates with suspected neonatal sepsis in a tertiary hospital, Mwanza-Tanzania. BMC Pediatr, 2010, 10:39
Mehar V, Yadav D, Somani P, et al. Neonatal sepsis in a tertiary care center in central India: microbiological profile, antimicrobial sensitivity pattern and outcome. J Neonatal Perinatal Med, 2013, 6(2):165–172
Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing, Twenty-eighth Informational Supplement, M100-S28. Wayne, PA: Clin Lab Stand Institute; 2018.
Britz E, Perovic O, von Mollendorf C, et al. The Epidemiology of Meningitis among Adults in a South African Province with a High HIV Prevalence, 20092012. PloS one, 2016, 11(9):e0163036
Guo, LY, Liu, LL, Liu Y, et al. Characteristics and outcomes of cryptococcal meningitis in HIV seronegative children in Beijing, China, 2002–2013. BMC Infect Dis, 2016, 16(1):635
Denkinger, CM, Schumacher, SG, Boehme, CC, et al. Xpert MTB/RIF assay for the diagnosis of extrapulmonary tuberculosis: a systematic review and meta-analysis. Eur Respir J, 2014, 44(2):435–446
Bilal A, Taha, MK, Caeymaex L, et al. Neonatal Meningococcal Meningitis In France From 2001 To 2013. Pediatr Infect Dis J, 2016, 35(11):1270–1272
Heydari B, Khalili H, Karimzadeh I, et al. Clinical, Paraclinical, and Antimicrobial Resistance Features of Community-Acquired Acute Bacterial Meningitis at a Large Infectious Diseases Ward in Tehran, Iran. Iran J Pharm Res, 2016, 15(1):347–354
Guo J, Zhou J, Zhang S, et al. A case-control study of risk factors for HIV-negative children with cryptococcal meningitis in Shi Jiazhuang, China. BMC Infect Dis, 2012, 12:376
McKenney J, Bauman S, Neary B, et al. Prevalence, correlates, and outcomes of cryptococcal antigen positivity among patients with AIDS, United States, 1986–2012. Clin Infect Dis, 2015, 60(6):959–965
Bowen, LN, Smith B, Reich D, et al. HIV-associated opportunistic CNS infections: pathophysiology, diagnosis and treatment. Nat Rev Neurol, 2016, 12(11):662–674
Rhein J, Morawski, BM, Hullsiek, KH, et al. Efficacy of adjunctive sertraline for the treatment of HIV-associated cryptococcal meningitis: an open-label dose-ranging study. Lancet Infect Dis, 2016, 16(7):809–818
Thwaites, GE, van Toorn R, Schoeman J. Tuberculous meningitis: more questions, still too few answers. Lancet Neurol, 2013, 12(10):999–1010
Marais S, Thwaites G, Schoeman, JF, et al. Tuberculous meningitis: a uniform case definition for use in clinical research. Lancet Infect Dis, 2010, 10(11):803–812
Morfin-Otero R, Noriega, ER, Dowzicky, MJ. Antimicrobial susceptibility trends among grampositive and -negative clinical isolates collected between 2005 and 2012 in Mexico: results from the Tigecycline Evaluation and Surveillance Trial. Ann Clin Microbiol Antimicrob, 2015, 14:53
Author information
Authors and Affiliations
Corresponding author
Additional information
This project was supported by the National Mega Project on Major Infectious Disease Prevention (No. 2017ZX10103005007).
Rights and permissions
About this article
Cite this article
Tian, L., Zhang, Z. & Sun, ZY. Pathogen Analysis of Central Nervous System Infections in a Chinese Teaching Hospital from 2012–2018: A Laboratory-based Retrospective Study. CURR MED SCI 39, 449–454 (2019). https://doi.org/10.1007/s11596-019-2058-7
Received:
Revised:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11596-019-2058-7