Abstract
This article examines the relationship between social inequity and the immune system, emphasizing some of the many ways that systemic racism and other forms of marginalization can undermine health. Of much sociological concern, chronic stressors increase inflammation and consequent susceptibility to health morbidities and, ultimately, mortality by burdening marginalized group members in ways that adversely affect immune regulation and functioning. As with social systems more generally, the immune system is a cross-scale complex system of many regulating, coordinating, and interacting parts, within both itself and the other bodily systems it protects. Along these lines, we thus propose that to properly conceptualize how social conditions undermine immune functioning and health, it is important to consider the immune system beyond its component mechanisms and parts. This view is akin to the way critical race theory proposes that “systemic racism” in the United States is a collaborative arrangement of social structures whose explanatory richness and historical durability can only be fully understood as a gestalt. We therefore seek, where possible, to emphasize the systems nature of the immune system similarly to the sociological insight that society comprises complex systems whose interrelated structures interact in dynamic and sometimes unpredictable ways. We scaffold this discussion within the literature on systemic racism in the United States, emphasizing inflammation as a key marker of immune demand and dysregulation and highlighting some implications for health inequities among marginalized populations more generally.
Zusammenfassung
In diesem Beitrag wird die Beziehung zwischen sozialer Ungleichheit und dem Immunsystem untersucht, wobei einige der vielen Arten hervorgehoben werden, wie systemischer Rassismus und andere Formen der Marginalisierung die Gesundheit beeinträchtigen können. Von großer soziologischer Bedeutung sind chronische Stressoren, die die Entzündung und damit die Anfälligkeit für Erkrankungen und letztlich die Sterblichkeit erhöhen, indem sie Mitglieder marginalisierter Gruppen in einer Weise belasten, die sich negativ auf die Immunregulation und -funktion auswirkt. Wie soziale Systeme im Allgemeinen ist auch das Immunsystem ein komplexes System mit vielen regulierenden, koordinierenden und interagierenden Teilen, sowohl intern als auch mit den anderen körperlichen Systemen, die es schützt. In diesem Sinne schlagen wir vor, das Immunsystem über seine einzelnen Mechanismen und Teile hinaus zu betrachten, um zu verstehen, wie soziale Bedingungen die Funktion des Immunsystems und die Gesundheit beeinträchtigen. Diese Sichtweise ist vergleichbar mit der Art, wie „systemischer Rassismus“ in den USA durch die kritische Rassentheorie gefasst wird. Demzufolge ist systemischer Rassismus eine kollaborative Anordnung sozialer Strukturen, deren Erklärungsreichtum und historische Dauerhaftigkeit nur als Gestalt vollständig verstanden werden kann. Wir versuchen daher, wo immer möglich, den Systemcharakter des Immunsystems zu betonen, ähnlich wie die soziologische Erkenntnis, dass die Gesellschaft aus komplexen Systemen besteht, deren miteinander verbundene Strukturen auf dynamische und manchmal unvorhersehbare Weise interagieren. Wir ordnen diese Diskussion in die Literatur zum systemischen Rassismus in den USA ein, wobei wir Entzündungen als einen wichtigen Marker für die Nachfrage und Dysregulation des Immunsystems hervorheben und einige Implikationen für gesundheitliche Ungleichheiten unter marginalisierten Bevölkerungsgruppen im Allgemeinen aufzeigen.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1 Introduction
From a critical race theory (CRT) perspective, the concept of systemic racism denotes a complex system of racial power and privilege that denies Black people full and equal access to economic, political, social, ideological, and other cultural resources and opportunities (Bonilla-Silva 1997). Research across multiple disciplines documents and illustrates a diversity of ways by which systemic racism operates, is coordinated, and is maintained through institutional practices, policies, culture, and microsociological encounters to shape risks for inequitable life experiences and outcomes for Black Americans (Delgado and Stefancic 2023; Ray 2022). A key insight of a critical and systemic view of racism is that the interplay among the many interconnected social systems within and spanning layers of social organization from micro to macro, each playing causal roles within its sphere of influence, collectively constitutes a robust and mutually reinforcing complex system. By interlocking together and buttressing one another, the dynamics of these various factors reinforce the status quo, sustain the existing racial hierarchy, and perpetuate the inequities it produces (e.g., Reskin 2012). The gestalt of this emergent system of racial power and privilege increases the challenges Black Americans face across life domains, forming barriers, blocking opportunities, and making the world a more dangerous and threatening place—both materially and existentially. The varied social forces comprising systemic racism are thus widely regarded as key contributors or “fundamental causes” that regulate the risks of many forms of adversity, including chronic stress, health morbidities, and, ultimately, mortality (Glass and McAtee 2006; Link and Phelan 1995).
We expect the notion that a social system involves the complex interplay between reinforcing and competing structures at multiple physical and temporal scales to be sociologically intuitive and central to the sociological imagination (Mills 2022). Taking systemic racism as metaphor, we argue that the body should be understood and intuited similarly. Like systemic racism, the immune system is also a complex nonlinear system of many coordinating and interacting parts (Ahmed and Hashish 2006; Thomas-Vaslin 2017). Moreover, the immune system’s role in the body is multifaceted, as it is a sophisticated self-regulator that adapts both to itself and to the broader inner milieu of the body over different time scales while also interacting with the primary regulator of the body, the brain, in complex bidirectional ways (e.g., Dantzer 2018). These processes all occur vis-à-vis social environments comprising a “stress universe” whose challenges have been characterized along multiple dimensions (Wheaton 1994), the particular constellations of which are underwritten by systemic racism for Black Americans (i.e., Williams 2018). Although the immune system is highly sophisticated in its ability to both anticipate and adapt to a wide range of threats and challenges, chronic exposure to stress undermines and impairs immune function regulation and the ways it interacts with the very body it attempts to protect (Arnaldo et al. 2022).
Therefore, our goal in this paper is, first, to review how racism and social conditions impact immune functioning, particularly with respect to inflammation, which brings forward broad implications for health morbidity and mortality risks (Ferrucci and Fabbri 2018; Furman et al. 2019). As with much prior work, we first seek to understand some important component mechanisms of the immune system that are accessible to measurement modalities that have been incorporated into large-scale survey research designs. Second, we step back to consider the immune system from a multisystem perspective. We propose that to understand how social conditions undermine immune functioning and health, it is important to consider the immune system beyond its component mechanisms and parts, akin to the way that systemic racism is an arrangement of social factors that each make their own contributions but whose larger meaning and consequence emerge only as a gestalt. Although our interest at this stage is conceptual, it speaks to the potential of “immunomics” and other bioinformatic approaches that seek to provide cross-scale system-level insights into immune state dynamics (Bonaguro et al. 2022).Footnote 1 In other words, where our first goal is to provide descriptions and summaries over “mechanisms” reflecting current and common understandings, the second goal seeks to provide perspective and theoretical vantage.
2 Racism and Social Conditions
2.1 Systemic Racism and the Stress Universe
A key insight from CRT is that notions of “race” are both socially constructed and deeply interwoven in the social, political, economic, and cultural fabric of society, challenging the simplified idea that racism is “merely” the result of individual prejudice or bias (i.e., what could be called the “bad apples” hypothesis). By highlighting the many forms that racism takes and how it is embedded within cultural norms, institutional practices, policies, and local microsocial dynamics that work together to filter the opportunities and experiences of people of color, CRT has played a key role in illuminating the historical processes of marginalization and oppression from slavery into the present in the United States (Mills 2022). A key idea underpinning the CRT argument is that the systemic racism of today is the inheritance of a racial hierarchy that was developed to justify slavery in the past (Kendi 2016; Muhammad 2019). The systemic racism concept, therefore, refers to the ways in which institutional practices and policies work together across social domains to create and maintain racial inequities broadly construed and widely documented in the United States, even in the absence of overtly discriminatory intent or individual acts of bias (Williams 2020).Footnote 2 Because systemic racism involves the allocation of resources, opportunities, and privileges based on race/ethnicity defined against whiteness and European ancestry, it produces unequal outcomes for different racial groups throughout the social ecology.
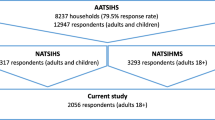
Figure 1 adapts Reskin’s (2012) depiction of “über discrimination,” which (partially) expresses systemic racism as an interconnected system of institutional arrangements. In this characterization, racism occupies a central role in shaping the policies, practices, and cultural factors embedded in different institutions. In turn, these social structures themselves reproduce racism by virtue of the relative disadvantages they produce through their own patterned activities, in turn sustaining and (both implicitly and explicitly) privileging White advantage. Racism is thus proposed to filter the experiences of Black people in the United States across levels of social organization and levels of abstraction from specific policies to the cultural headwinds that shape how race is conceptualized and how people of different backgrounds are essentialized (e.g., Graves Jr. 2001), ultimately filtering down into individual-level acts of bias and discrimination (Williams 2020). It is also important to note the bidirectionalities of the pathways between institutions in Fig. 1 and the ways they reinforce each other, so that an inequity in one area frequently propagates to others and vice versa, both directly and indirectly, reinforcing that initial inequality. It is in this sense that racism comprises a complex system that is self-reinforcing and durable. Moreover, recognizing these interdependencies and (positive) feedbacks is why the move from interpersonal racial discrimination at microsociological scales of interaction and toward systemic racism integrating over cross-scale levels of social organization is so critical to understanding racism as a systems concept (Bonilla-Silva 1997, 2015, 2019).
System representation of systemic racism. (Adapted from Reskin (2012))
An important consequence of the dynamics of such a system of inequity is the organization and distribution of the stressors to which different social groups are exposed. The concept of the stressor is usually characterized in two parts composed of the challenges or demands of the environment that tax or exceed the individual’s ordinary capacity to adapt, and the absence of means to attain sought-after ends (Aneshensel and Mitchell 2014). The stress universe characterizes stressors in terms of duration (e.g., discrete, intermittent, chronic), severity (e.g., mild to severe), level of social organization (e.g., micro to macro), and life course (e.g., life stage, timing, sequencing; Aneshensel and Mitchell 2014; Wheaton 1994). An important feature of the system of structurally embedded racism described in Fig. 1 is therefore the ways that stress is embedded dynamically in the social structures through which individuals pass on their journeys through life, increasing the risk of stressor exposures across scales—ranging from broad patterns of residential segregation (Massey and Denton 1993) to microsociological interaction dynamics (e.g., discrimination and social rejection; Cheadle et al. 2020; Goosby et al. 2018; Jelsma et al. 2021). Figure 1 therefore provides a model of how the “stress universe” (Wheaton 1994) arises from the socially structured and patterned experiences of Black Americans and perpetuates long-standing durable population health inequities (Goosby et al. 2018).
2.2 Black Health Inequities in the United States
As shown in Fig. 1, racism is posed to sustain, and be sustained by, itself through the diversity of social structures in which it is embedded, the dynamics among them, and the actions and behaviors of individuals within them (e.g., Ray 2019). Consequently, researchers have uncovered “Black–White” disparities pretty much wherever they have looked, whether in different social contexts, over different levels of analysis, across disciplines, or spanning areas within research disciplines (Hardeman et al. 2022). Such inequities are ubiquitous, and there is no single “node” in the network of social systems and structures by which the challenges that racism poses can be eliminated through one decisive policy or set of actions, even if the “causal effect” of any single arrowed pathway could be identified and intervened upon (Stewart 2023). Figure 1 can therefore be read as illustrating, in part, how the stories White people have been telling about Black people are sustained: a disparity in one area is (circularly) taken as proof justifying disparities in other areas—criminality\(\leftrightarrow\)low intelligence\(\leftrightarrow\)poor work ethic\(\leftrightarrow\)etc. The outcome disparities described in life chances, broadly construed, arise not just from the localized dynamics of the nodes depicted in Fig. 1 but also from the system-sustaining collective interplay among them. Health is of particular concern because the embodiment of this social structure is costly in terms of morbidity and, ultimately, loss of life and loved ones earlier in the life course (Umberson et al. 2017).
To put a sense of scale to the consequences of systemic racism in the United States, the accrued loss of life over the voting years is sufficient to alter national election outcomes in favor of Republican candidates (Rodriguez et al. 2015; see also Montez et al. 2021), members of the party waging an ongoing public war of denial against CRT throughout the United States (Alexander et al. 2023). Importantly, the consequences of these mortality differentials are apparent even when accounting for the mass incarceration of Black Americans, a system likened to a “New Jim Crow” era of intensive racial profiling, mandatory minimum sentences, felony disenfranchisement of voting, and discrimination in housing and employment (Alexander 2020; Rodriguez et al. 2015), consistent with the depiction in Fig. 1. To provide another view, there has recently been a growing concern for “White deaths of despair” reflecting the rise in White mortality in recent years. While recognizing the importance of these trends, which are not limited to only Whites in recent cohorts (Gaydosh et al. 2019), it is also important to note that Black–White disparities remain large, even after years of improving Black mortality rates (Woolf et al. 2022). In fact, the COVID-19 pandemic turned out to be telling. Wrigley-Field (2020) estimated that 400,000 excess White deaths would be needed to equal the best mortality ever recorded among Black Americans outside of the pandemic, such that the White mortality levels would have needed to increase by a factor of nearly 6 at the time the study was conducted. Indeed, White life expectancy in 2020 was predicted to remain higher than the best recorded Black life expectancy ever, barring nearly 700,000 excess White deaths. In short, Black disadvantage every year was larger than Whites’ experience of COVID-19 in 2020 in the United States.
These excess deaths are the realization of the tolls that systemic racism takes upon multiple physiological systems across interacting levels of biological organization (McEwen 1998; Bobba-Alves et al. 2022; Goosby et al. 2018). To give a broad overview of morbidity and mortality differentials, racial health disparities have been found for cardiometabolic conditions including cardiovascular disease, type 2 diabetes, hypertension, and adiposity, along with rates of certain cancers, low-birth-weight births, and infant mortality (Bailey et al. 2017). A key aspect of these Black–White morbidity and mortality differentials is the immune system, particularly inflammatory processes. Inflammation is increasingly recognized as playing numerous roles related to health morbidities and mortality (Ferrucci and Fabbri 2018; Furman et al. 2019). For Black Americans, the systemic embedding of adverse social conditions and experiences elevates risks for numerous inflammatory conditions (see Goosby et al. 2018). Notably, the complex, reinforcing systems that shape how these morbidity risks operate are analogous to the complexity of the immune system, which when adapting to such ecological conditions elevates the likelihood of chronic inflammation and the subsequent morbidities noted above. Our next sections introduce the immune system as a complex system, followed by a discussion of the links between racism, immunity, and Black–White health inequities.
3 The Immune System as a Complex System
3.1 Introduction
The immune system is our first line of defense against foreign or noxious invaders such as bacteria and viruses, as well as the body’s own damaged cells, whose dysfunction can cause havoc (e.g., cancer). A critical function of immune activity is inflammation, which includes the processes by which immune and nonimmune cells are put into action to protect an organism by both eliminating pathogens (or disease-causing threats) and promoting tissue repair and healing (Netea et al. 2017). Inflammation draws upon two distinct but synergistic immune system branches: the innate (i.e., immediate, nonspecific, inherited immunity) and the adaptive (i.e., acquired through experience) immune systems (Bennett et al. 2018). Therefore, we begin here first. Because we introduce some terms that may not be familiar to readers, Table 1 provides a glossary of terms used in what follows.
3.2 Innate and Adaptive Immunity
Innate immunity is the first line of defense, providing rapid responses to pathogen exposure. This system involves not only immune cell defense but physical and chemical barriers (e.g., skin, mucous membranes in the respiratory system; Bennett et al. 2018). Innate immune activity is nonspecific, defensive, and general in the sense that it does not “memorize” or “learn” specific antigens (i.e., features of the molecular structure of the invader or toxin) to distinguish “self” from “nonself” (Marshall et al. 2018; McDade et al. 2016).Footnote 3 Rather than modeling and identifying specific antigens, the innate immune system uses more general, less specific pattern recognition receptors (PRRs) to detect groups of pathogens that share common molecular structures, called pathogen-associated molecular patterns (PAMPs; Marshall et al. 2018). In its role as the first responder, innate immunity embodies general hypotheses about what kinds of pathogens it might encounter, allowing it to mobilize quickly to broad classes of invaders.
Like a key fitting into its lock, an invading antigen is a molecular structure that can bind to a receptor, itself a molecular configuration on a cell, such as a B cell or T cell of the immune system, with its own structure and electrical properties (Marshall et al. 2018). Receptors on the surface of a cell are its sensors of its environment, so an antigen binding to a compatible receptor constitutes a signal that can alter a cell’s activity. By virtue of this interaction, the cell acquires new information on what it should be doing and what its state should be (e.g., changes in gene expression; Cheung and Spielman 2009). The immune system surveils and identifies invaders using both nonspecific and specific antigen profiles using the PRRs, found on the surface of immune cells, such as macrophages and dendritic cells, that are responsible for recognizing specific PAMPs on invaders (nonself) and damage-associated molecular patterns (DAMPs) on cells (self; Gong et al. 2020). Humans genetically inherit antigen profiles responded to by nonspecific innate immunity, as well as specific antigen profiles based on different exposures throughout their lives that shape their adaptive immunity. This is why some people may be more susceptible to certain infections or diseases, whereas others may be naturally resistant due to their unique antigen profile.Footnote 4
The innate immune system, while kickstarting the general immune response, also initiates the adaptive immune response. Adaptive immunity (sometimes called acquired immunity), in comparison to innate immunity, is antigen (e.g., invader) specific. It provides the slower and more precise activity of the immune system, learning from exposure by embodying predictions about which pathogens might be encountered again in the future and the tools to defeat them (Bhat et al. 2021). Adaptive immunity is primarily responsible for distinguishing and identifying “self” versus “nonself” antigens via the generation of pathogen-specific pathways, which work to eliminate specific pathogens or pathogen-infected cells (Bennett et al. 2018). Upon initial pathogen exposure, the adaptive immune response develops an immunologic memory, a process that unfolds over several days but can later be used to more quickly eliminate the pathogen should it invade again (Marshall et al. 2018).
Adaptive immunity is therefore conditional on the exposures one has over the life course. Responsivity is therefore slow at first exposure as the immune system is “trained” to respond to the vicissitudes of its body’s environment, and then it becomes much quicker, more targeted, and specific as those immunologic memories embody predictions about which challenges and threats are likely to be encountered again. Such predictions are encoded in special memory B cells through the identification of the specific molecular profiles of a pathogen and the subsequent production of cellular defenses in the form of T lymphocytes (T cells), a type of white blood cell specific to that antigen. These cells are produced in bone marrow, mature in the thymus gland, and are built up and mobilized for specific immune events. The actual adaptive immune processes unfold via the initiation of certain mature T helper cells (i.e., CD4+ cells) that play important roles in coordinating signaling proteins called cytokines that facilitate intracellular communication, such as activating B lymphocytes (B cells), also a type of white blood cell, which produce the antibodies that recognize and neutralize specific pathogens (e.g., viruses; Barrows et al. 2019; Turnbull and Rivier 1999). Thus, this cascade leads to the neutralization and destruction of the pathogen via the production of antibodies matched to its specific antigen profile, followed by the creation of memory B cells that can recognize the pathogen if reintroduced again in the futureFootnote 5 (Marshall et al. 2018).
3.3 The Importance of Cytokines
Cytokines are signaling proteins produced by immune and other cells (e.g., endothelial cells, fibroblasts, epithelial cells) that make up the signal networks both within the immune system and with other cells and tissues. Cytokines can have both proinflammatory and anti-inflammatory roles, depending on their function and the context in which they are produced. Some cytokines, such as interleukin‑1 (IL-1), interleukin‑6 (IL-6), and tumor necrosis factor-alpha (TNF-α), are proinflammatory and promote the activation and proliferation of immune cells, as well as the recruitment of immune cells to sites of infection or injury (Bennett et al. 2018). Other cytokines, such as interleukin-10 (IL-10) and transforming growth factor-beta (TGF-β), are anti-inflammatory and help to limit the immune response and prevent excessive inflammation (Bennett et al. 2018). Cytokines also play roles in other physiological processes, such as cell growth and differentiation, wound healing, and regulation of red blood cell production (hematopoiesis) (Turnbull and Rivier 1999).
Overall, cytokines are important mediators of immune activity and play critical roles in maintaining regulatory balance between proinflammatory and anti-inflammatory activity (immune homeostasis), as well as protection from infection, disease, and cellular dysfunction. By providing the communication backbone of the immune system while being measurable, cytokines play a key role in measurement and assessment of the immune system in terms of “what is happening” in the body in sociological and population health research (Furman et al. 2019). To provide an analogy, this approach, for all its sophistication, would be a bit like sampling a limited range of audio frequencies every few minutes during a symphony and then attempting to transcribe the symphony from this limited information.
It is important to note that innate and adaptive immune functions operate with different temporal parameters and modes of action, but they are jointly crucial to the effectiveness of inflammatory activity when things go wrong in the body, and not just to invaders. In addition to the “military” role of the immune system, it is important to recognize that it provides “policing” roles within the body as well. Acute inflammatory activity is kickstarted by PAMPs recognition identifying a “nonself” invader, which comes along with DAMPs initiated when cells signal that they have been damaged or are in distress (Gong et al. 2020). DAMPs, which are structurally and functionally diverse, are not caused by pathogenic infections directly but instead by noninfectious physical, chemical, or metabolic agents, and are thus described as “sterile” because they are noninfectious (Behnia et al. 2016). DAMPs signal that cells have been damaged and so play key roles in signaling to the innate immune system that something is wrong with the body itself and that inflammatory activity needs to be increased (Roh and Sohn 2018). Elevation in inflammatory activity is meant to be short term, however, and is intended to be downregulated in response to anti-inflammatory signals once the threat is resolved (McDade 2023). The goal of achieving balanced pro- and anti-inflammatory activity is restoration of immunologic homeostasis, sometimes referred to as inflammatory equilibrium (Eberl 2016). Inflammation that persists in the absence of pathogens or cellular damage is termed chronic low-grade inflammation (Furman et al. 2019), and it is known to elevate risk for inflammation-related diseases, which will be addressed in later sections.
3.4 The Immune System as a Complex System
A key challenge to both understanding and describing the immune system is that it has many parts with many interactions and supporting numerous functions, including its own regulatory mechanisms; it can be likened to a complex dynamic system that learns and adapts to its environment and itself (Ahmed and Hashish 2006; Thomas-Vaslin 2017). We note at the outset that considerable effort is still being given to mapping the immune system over its many cells, constituents, processes, and dynamics (Bonaguro et al. 2022; McDade 2023; McDade et al. 2021). There is no manual yet, and its intricacies continue to be explored and are often complicated. Most sociologically relevant work on inflammation and the immune system follows mechanistic models by which biological measures, usually of cytokines or C‑reactive protein, an upstream inflammatory marker representing the different parts of the immune communication network, are analyzed independently or are indexed in small clusters of biomarkers that predict, or are predicted by, individual and social variables (e.g., Cuevas et al. 2020; Harris and Schorpp 2018). Much research on inflammation therefore principally emphasizes signaling among the different components of the immune system statically and without capturing dynamics (McDade et al. 2021; McDade 2023).
A depiction of the immune system as a complex dynamic system idea is presented in Fig. 2a (Stanley and Lacy 2010; Jawa et al. 2011; Chen et al. 2012), which shows a cytokine signaling network among immune cell families. There are numerous chemical messaging mediators and communication pathways governing immune system coordination. For example, after recognizing the presence of pathogens (i.e., “not self”) by binding to surface or secreted proteins, the immune system coordinates messenger cascades that modulate cellular activities (Stanley and Lacy 2010). These cells play different roles and communicate with each other via cytokines, which control proliferation, differentiation, and function of immune system cells, increasing or decreasing inflammation depending upon the resulting actions of pro- and anti-inflammatory cytokines (Jawa et al. 2011). While it is tempting to think in terms of an immune event and the resource martialing cascades that follow, it is more theoretically profitable to recognize that such activity is ongoing and inherent—the world outside is always trying to get in, and cells in the body are always breaking down and misbehaving.Footnote 6 The immune system thus manages a diversity of ongoing activities across diverse fronts, seeking to slow down, obfuscate, and destroy what is not self and that which was but functionally no longer is.
Cytokine communication networks. a Examples of cytokine signaling pathways among immune cell types (Protein Lounge 2024). b The cancer immune system (26 nodes, 107 interaction links) among cells (blue ovals) and cytokines (yellow diamonds). Interactions include cell–cell activation (black arrows) and inhibition (black lines), cytokine–cell activation (red dashed arrows) and inhibition (red dashed lines), and cell–cytokine production (green). (Reproduced from Wenbo and Wang (2017). Used with permission)
As a companion representation, Fig. 2b shows a focal empirical cancer immune system network over 26 cells and 107 interaction links, revealing complex cell–cell regulatory relations in black (solid: activation; dashed: inhibition), cytokine activation (solid) and inhibition (dashed) in red, and cellular cytokine production in green (Wenbo and Wang 2017, Fig. 1, p. 2). These figures make the point that the kinds of immune markers increasingly available for assaying and modeling in social science data sets are not independent, either with what has been measured within this system (e.g., IL-6) or interdependent processes that have not been measured. This, at its core, is a challenge of attempting to measure and model or predict with subsets of a complex system. Immune function and inflammatory activity are ongoing and continuous dynamics of cellular activities and signaling and regulatory cascades, which proliferate and differentiate akin to the example of systemic racism in Fig. 1. As discussed above, immune activity is about more than merely responding to invaders in the body or parts of the body that are broken or not working properly (e.g., cancer); immune activity and communication are part of the normal, routine, constant dialogue of bodily systems with each other. Immune activity is thus always happening, making communication and regulatory dynamics key features of the system. Our bodies are awash in communication signals, and the songs of the immune system are expressed in these “frequencies.”
3.5 Immune Dynamics, the Brain, and Allostatic Regulation
The view of the immune system, say from the perspective of combatting and eliminating a virus such as SARS-CoV‑2 (and its many lineages), which causes COVID-19, tends to emphasize the peripheral immune system largely independent of its bodily context, just as we described when introducing the innate and adaptive immune systems. To help clarify what we mean, we provide a conceptual model in Fig. 3, showing a direct path from the environment and into the body. There is much here of considerable sociological interest as this pathway speaks directly to environmental inequalities and the direct effects they can have upon the body, as with the kinds of environmental racism (Henderson and Wells 2021; Lord et al. 2023) that systemic racism gives rise to. Managing and restricting the harms of such insults is a key feature of the peripheral immune system, whose regulatory dynamics (Fig. 2) are referenced via the self-loop in Fig. 3. When a new invader from the environment comes on board and is recognized (i.e., PRRs and specific B cell receptors), innate and adaptive immune systems initiate the processes of inflammation, and a communication cascade of cytokines calls attention to the problem and kickstarts the cascades of cellular actions and subsequent signals that work to amplify and regulate the inflammatory response.
Returning to the self-regulatory component in Fig. 3, in the immediate response to detection of an antigen indicating the presence of a toxin or foreign substance, it is the immune system signaling cascades that mobilize and coordinate immune activity, sending cells to the site of damage while producing antibodies (proteins) that circulate in the blood to recognize foreign substances such as bacteria and viruses to neutralize them (Marshall et al. 2018). This form of acute inflammation arises in response to an injury or infection, and antibodies produced by B cells continue to circulate throughout the body after pathogen exposure to protect against that antigen in the future. All of this activity can be dangerous to other cells in the body, which white blood cells called T regulatory cells (Tregs) regulate to protect the body from immune overactivity. Circulating Tregs control inflammation to prevent tissue damage in the presence of foreign external antigens (i.e., external sources such as wounds) and internally produce antigens such as those from early cancer cells (Schmidt et al. 2011). In short, Tregs help to downregulate activity of other immune cells to prevent the development of autoimmune diseases or allergies while also protecting unharmed tissue around infections to keep them healthy (Dolina et al. 2022). This immediate activity then instantiates systemic neuroendocrine and other neuronal actions that, if successful, eventually resolve the recovery process, moving the immune system into its baseline, day-to-day, homeostatic activity state balancing pro- and anti-inflammatory activity (Bennett et al. 2018).
At this point, we have described the immune system working independently of the central nervous system, and now we move to the neuroimmune loop in Fig. 3. The brain contains its own immune processes that produce cytokines and are responsible for functional and structural interactions between endothelial cells, glia, and neurons (Dantzer 2018). Cytokines, present in the brain, regulate and curate neuronal structures and plasticity. In this way, immune signals can influence the brain’s immune system via a downregulating neuroendocrine feedback loop involving cytokine action on the brain’s self-regulatory immune processes (Quadt et al. 2018). Thus, the brain’s immune system operates both as a self-contained self-monitoring system studied by neuroimmunologists and as part of an external regulatory loop that makes use of the central nervous system and its means of communication with the rest of the body, including the autonomic and neuroendocrine systems.
The brain also plays a pivotal role in immune function for other reasons. A rapidly expanding literature is demonstrating the various pathways through which the immune system communicates with the brain, both altering inflammatory activity within it and altering immune activity outside of it (D’Mello and Swain 2017). This loop is depicted in terms of allostasis (predictive regulation from brain to body; Sterling 2012) and interoception (from body to brain; Chen et al. 2021). Although it was once thought that the brain was immune privileged or protected from damage that could be caused by inflammatory responses to pathogen exposure (Hong and Van Kaer 1999), this assumption was rejected with the discovery that antigens can access the brain and travel outside of it. When the immune system detects the presence of DAMPs or PAMPs, immune cells release inflammatory cytokines, which are then communicated to the brain via neural (i.e., nervous system), humoral (i.e., extracellular fluid circulation), and cellular pathways to the brain, wherein the brain can adjust or amplify broader inflammatory activity in the body (Savitz and Harrison 2018).
For example, communications to the brain ascend via innervated visceral organs (e.g., heart, lungs, digestive organs) that send signals from cytokines through visceral afferents (i.e., neurons linked to visceral organs) via the vagus nerve (D’Mello and Swain 2017), the brain–body information superhighway. Humoral pathways are slower but provide another route of movement throughout the body, including extracellular fluids accessing the brain through circumventricular organs (i.e., structures in the brain with permeable capillaries, unlike the other tissues that reside within the blood–brain barrier) that can access the portion of the brain that lacks the blood–brain barrier. Another cellular pathway impacting the brain can, for example, occur through circulating immune cells (i.e., microglia) within the brain that have proinflammatory cytokine receptors on their surface. When the organism is healthy, microglia are critical in synaptic pruning, neural plasticity, and learning (Savitz and Harrison 2018). Microglia, immune cells in the brain that initiate cytokine activity, can be activated through peripheral inflammation when cytokines cross the blood–brain barrier, leading to the release of proinflammatory cytokines such as TNF‑α, IL-1β, and IL‑6, according to animal studies (D’Mello and Swain 2017). Although much of the literature on inflammation within the brain is based on animal models, a growing body of research is finding that prolonged activation of circulating proinflammatory cytokines (e.g., TNF‑α, IL-1β, and IL-6) is associated with behavior, mood, psychiatric, and neurodegenerative diseases (Kipnis and Filiano 2018).
Through allostatic regulatory mechanisms, the brain also engages in actions that are critical for regulating the immune system, as shown with the descending pathway in Fig. 3. The body tends not toward independence of systems but coordinated interdependencies that collaborate through signaling cascades and prioritize resource sharing (Sterling 2015, 2020). A primary means of brain to immune system collaboration is via the hypothalamic–pituitary–adrenal (HPA) axis and autonomic nervous system (ANS) outputs. The HPA axis neuroendocrine cascade (Turnbull and Rivier 1999) is the most heavily examined set of pathways evaluated in the biosocial literature in the context of stress-related activity (Hostinar and Gunnar 2017; Smith and Vale 2006; Turner et al. 2020). Importantly, the HPA axis and the ANS work together dynamically to regulate the immune system during stress exposure. Specifically, within the two branches of the ANS—the sympathetic nervous system (SNS; “fight or flight”) and the parasympathetic nervous system (PNS; “rest and digest”)—SNS arousal increases cellular and systemic immune activation, while the PNS and the HPA axis inhibit inflammatory responses (Bennett et al. 2018).
Though much of the stress regulation literature does not specifically address the role of the brain beyond appraisal of a situation as stressful or the chronicity of experiencing stressors, neuroscientist Bruce McEwen, who coined the term allostatic load, early on noted that the brain plays a key role in regulating the immune system (McEwen 1998; McEwen and Gianaros 2010). Specifically, he outlined how neural networks, including the hippocampus, amygdala, and prefrontal cortex, coordinate with the neuroendocrine, autonomic, and immune functions when adapting to stressful environmental and psychosocial challenges. Moreover, in our own work addressing the stress-related pathways undergirding the role of stress in discrimination exposure, we note that discrimination is a form of social threat of exclusion and that anticipation of exclusion initiates a cascade via specific brain regions (Goosby et al. 2018) activating the ANS and the HPA axis (Goosby et al. 2018; Jelsma et al. 2021; see also Zhang et al. 2021).
The HPA axis entails an interconnected system of direct and feedback loops between the hypothalamus and pituitary glands in the brain and the adrenal glands located on top of the kidneys, in service to regulating metabolic resources (Turnbull and Rivier 1999). When additional metabolic resources are needed, the HPA axis signals to increase circulating hormone levels by activating corticotropin-releasing hormone, which initiates the release of adrenocorticotropic hormone into the bloodstream. In turn, adrenocorticotropic hormone signals for the release of glucocorticoid hormones, including cortisol, a key energy mediator and ultimately much more integral moment-to-moment in life than just being “the stress hormone,” as it is often referred to. Basal cortisol secretion is on a stable diurnal cycle but is also released based upon the demands and conditions of the moment and those anticipated in the near future. For example, circulating cortisol can be increased when immune activity is high, just as when external conditions such as perceived social stressors are present (Bennett et al. 2018). In a healthy immune system, immune cells express glucocorticoid receptors that allow the immune system to inhibit immune cell activation and proinflammatory cytokine circulation (Dantzer 2018). When stress is chronic, elevated circulating cortisol can lead to downregulation or reduction of glucocorticoid receptor expression and thus elevate proinflammatory cytokine circulation. Changing receptor densities or sensitivities on cells means quite literally to alter the responsivity of the communication network, in this case decreasing cellular receptivity so that inflammation is increased.
The SNS innervation of the brain signals the body to make energy available and to prepare it for “fight or flight” (Bennett et al. 2018). The hypothalamus, located within the limbic system of the brain, manages key aspects of SNS activity and is called the sympathetic–adrenal–medullary system (Cohen et al. 2007; see Goosby et al. 2018). SNS-triggered sympathetic–adrenal–medullary arousal engages in allostatic regulatory patterns which, via the adrenal medulla, release the energetic hormones in the form of catecholemines, in this case epinephrine and norepinephrine, to increase heart rate, blood circulation, and respiration and to divert blood from nonessential organs to major muscle groups and the brain (Bennett et al. 2018). The release of catecholamines and norepinephrine are pro-inflammatory. For example, epinephrine signaling increases the production and circulation of IL‑6 and TNF‑α cytokines (van der Heijden et al. 2020). Conversely, the PNS acts to downregulate the SNS by slowing the heart rate, increasing digestion, and calming mood, and it can alter inflammatory expression to decrease cytokine production. In the presence of elevated chronic stress, the ability of the PNS to downregulate immune proinflammatory activity becomes diminished as SNS activation becomes more dominant, consequently leading to more ongoing proinflammatory signaling.
In short, and as shown in Figs. 2 and 3, the immune system is governed by interactions with itself and other bodily systems. What we have depicted is inclusive but far from complete. Rather, it speaks to the notion that the immune system is not just a set of mechanisms but an interactive and dynamic network of them. Mechanistic research, by nature, tends to emphasize specific, localized mechanisms at one level, often seeking more “precise” mechanistic explanation at lower levels of physical reality. A healthy, well-functioning immune system is not just a collection of mechanisms per se; rather, it is a complex system comprising a vast array of interacting mechanisms. The capacities of this system change over time based partly on their constitution (i.e., genetics) in combination with the history of environmental demands (e.g., chronic stress, pathogens). Moreover, immune activity and inflammation reflect both the multitude of mechanisms that constitute the system and the dynamics by which the immune system interacts with itself and other bodily systems. It is for this reason that we have sought to emphasize the immune system as a complex system rather than strictly as a collection of different mechanisms, and also why we have sought to present it in parallel to how sociologists might consider the interactive dynamics among social structures holistically, as with systemic racism.
3.6 Discussion of Inflammation and Its Implications for Health Morbidities and Mortality Risks
As mentioned above, the immune system attempts to achieve a balance between pro- and anti-inflammatory activity, healing, and then restoration activity to the basal levels needed to support the organism. But what happens when inflammatory equilibrium is not restored? Social, psychological, environmental, and biological factors can shift acute inflammation to low-grade, noninfective systemic chronic inflammation (SCI), drawing a direct line between social conditions and the systems and capacities the body uses to protect itself from invaders. This persistent proinflammatory activity can have various collateral consequences for the body and may be particularly insidious among people from Western, educated, industrialized, rich, and democratic (WEIRD; Gurven and Lieberman 2020) societies (McDade 2023). A key consequence of SCI is increased physiological wear and tear via tissue and organ damage, which elevates numerous morbidity risks (Furman et al. 2019).
In fact, immune system processes are so integral to the dynamics of the body that approximately 50% of all deaths worldwide are now linked to diseases with inflammatory components (Furman et al. 2019; Himmelstein et al. 2015). Common physical morbidities associated with inflammation include physical ailments such as diabetes, cardiovascular disease, cancer, and autoimmune and neurodegenerative disorders, as well as psychological morbidities such as depression, anxiety, and post-traumatic stress disorder (Netea et al. 2017; Quadt et al. 2018; Savitz and Harrison 2018). Inflammatory health conditions are linked to a variety of noxious inputs, including exposure to not only viral, bacterial, or physical trauma but also to other environmental conditions, including exposure to toxins, lack of access to safe physical spaces and healthy foods, and, just as important, psychological stress exposure and socially graded forms of stigmatization and marginalization (Ajilore and Thames 2020; Furman et al. 2019). In the United States, while chronic disease continues to rise among many social groups, racialized and stigmatized groups remain at disproportionately higher risk for experiencing many of these conditions, including more severe depression and anxiety along with post-traumatic stress disorder (Al Kibria 2019; McLaughlin et al. 2019; Uchima et al. 2019).
Social structures and conditions can regulate the risk of exposure to factors that initiate SCI (Glass and McAtee 2006; Goosby et al. 2018), and the chronicity of repeated exposures to stressors is thought to be a pathway through which the transition from acute inflammation shifts to SCI via ongoing regulatory demands and burdens (Arnaldo et al. 2022; Bobba-Alves et al. 2022; McEwen 1998; Rohleder 2019). As mentioned in the previous section, in addition to viral and bacterial exposures, noninfective conditions can also initiate the inflammatory neuromodulated cascade. Social scientists interested in the consequences of social conditions such as marginalization, isolation, and discrimination have noted that ongoing, unremitting exposures to such social stressors can lead to chronic upregulation of the body’s neuroendocrine (e.g., HPA axis) and inflammatory systems, over time elevating the risk for inflammation-related disease and behavior (Clark et al. 1999; Eisenberger et al. 2017; Eisenberger and Cole 2012; Yang et al. 2016). Chronic stress exposures can have long-term implications for inflammatory morbidity, with exposure to stressors during childhood and adulthood (e.g., poverty, maltreatment, racial discrimination) linked to psychiatric disorders, metabolic syndrome, and coronary heart disease later in life (Hobson et al. 2022; Nusslock and Miller 2016), for example.Footnote 7
Through the process of allostasis the body calibrates bodily systems via anticipatory adaptation to metabolic demands from internal and external inputs for optimal bodily function (Sterling 2012; Schulkin and Sterling 2019). Chronic stress takes what is an evolutionarily adaptive response of preparing the body to protect itself from threat and injury by mobilizing action in the here and now, but which is also costly, and eventually wears down the body through the burden placed on it by persistent stress-induced energetic and immunologic demands (Bobba-Alves et al. 2022; Arnaldo et al. 2022). The consequences of chronic stress for inflammatory-related condition risk are well established, involving dysregulation of physiological pathways connecting the brain, the ANS, and the neuroendocrine and immune systems to risks for hypertension, diabetes, neurodegeneration, and depression, to name but a few (Barrows et al. 2019; Byrne et al. 2016; Kinney et al. 2018; Muriach et al. 2014; Osei and Gaillard 2017). Below we outline an example of how chronic stress can elevate the risk for inflammation-related health conditions.
3.7 From Acute to Chronic Stress: The Path to Immunologic Morbidity
Under regular circumstances (i.e., acute stress), increased energetic demand is linked to an initial uptick in SNS arousal (i.e., elevated blood pressure, circulation, blood glucose release), increased inflammatory activity to protect against potential wounds and initiate healing, and neuroendocrine cascades (e.g., glucocorticoid release, inflammatory inhibition, dampening of insulin receptors). The HPA axis increases cortisol release, thereby boosting access to energy by dampening cellular sensitivity to insulin (i.e., increasing insulin resistance), the signaling hormone responsible for the storage of blood glucose in cells, among other metabolic processes. Cortisol, as previously mentioned, is also anti-inflammatory, making it critical for reducing longer-term inflammatory activity by downregulating proinflammatory cytokine activity. This series of allostatic adaptations makes energy available for action—“fight or flight,” colloquially—followed by adjustment to lower-demand functioning once the situation has changed or the threat has passed. This downregulation is accomplished by the PNS (“rest and digest”), which is generally anticorrelated with the SNS, by signaling to lower the heart rate, blood pressure, and glucose production.
In the context of social conditions in which stressors are chronic, however, patterns of SNS arousal and upregulation of HPA axis activity, including elevated levels of cortisol secretion and proinflammatory activation, become consequential. For those exposed to chronic stress, physiological regulation is targeted to the expectation of increased demands, and so higher than normal blood pressure is maintained, leading to wear and tear on arteries and initiating inflammatory damage, elevating the risk for hypertension (i.e., chronic high blood pressure) and cardiovascular diseases (e.g., arterial sclerosis; Barrows et al. 2019; Youwakim and Girouard 2021). Moreover, ongoing chronic stress may elevate cortisol levels for extended periods while simultaneously reducing glucocorticoid receptor expression, leading to excessive levels of circulating proinflammatory cytokines and insulin resistance, a precursor to type 2 diabetes (Dantzer 2018). This point is important because changing cellular sensitivity alters both cell activity and the way information is processed within intercellular communication networks. In the case of the glucocorticoid cortisol, chronic stress can lead to excessive circulation of proinflammatory cytokines resistant to circulating cortisol levels (Nusslock and Miller 2016) or to secretion of excess cortisol, dampening cortisol receptor receptivity and reducing receptors through an interactive pathway resulting in glucocorticoid resistance (Zefferino et al. 2021). This process also leaves individuals vulnerable to risk for cardiovascular disease and type 2 diabetes, a condition of insulin-resistant elevated high blood glucose (Iob and Steptoe 2019; Joseph and Golden 2017).
There are also consequences of SCI for human behavior, psychiatric conditions, and neurodegeneration. The production and metabolism of neurotransmitters such as serotonin and dopamine, which play critical roles in motivation, mood, and emotion, can be influenced by proinflammatory cytokine circulation (Bennett et al. 2018; Renna 2021). Such changes, in turn, have implications for behavioral and psychosocial outcomes. For example, continuous elevated circulation of proinflammatory cytokines in the brain and throughout the body can cause the initiation of sickness behaviors (Eisenberger et al. 2017). Sickness behaviors include symptoms such as social withdrawal, fatigue, anhedonia, and physical pain, and these conditions are associated with elevated levels of depression and anxiety. Evolutionarily, sickness behavior is a protective survival response allowing for withdrawal to avoid injury and reduce the risk of infecting others while allowing for healing. Social stressors, however, can also elevate sickness behaviors, and as a consequence, there is evidence that those who are more inflamed are more sensitive to social stressors such as rejection (Eisenberger et al. 2017; Eisenberger and Cole 2012). These sickness behaviors are also highly correlated with both psychopathologies and neurodegeneration (Quadt et al. 2018).
A growing literature is also linking allostasis (the predictive and coordinated regulation of expected homeostatic set points; Arnaldo et al. 2022; Sterling 2012) and interoception (the sensing and perception of bodily processes; Chen et al. 2021) to the risk for mood disorders such as major depression, anxiety, and post-traumatic stress disorder (e.g., Barrett 2017; Barrett et al. 2016; Savitz and Harrison 2018; Zheng et al. 2021). The experience of trauma and other forms of acute and chronic stressors is associated with elevated circulating levels of proinflammatory markers, including IL-1β, IL‑6, TNF‑α, and C‑reactive protein (Michopoulos et al. 2017). As previously noted, the immune system communicates with the brain through humoral, neural, and other cellular messengers. Under the strain of chronic stress, cytokines sent to the brain can initiate monocyte production of proinflammatory cytokines within the brain, which then initiate impairments in portions of the brain linked to reward and motivation processing, possibly contributing to depression (Byrne et al. 2016; Savitz and Harrison 2018). Importantly, in line with emerging models of depression as a problem of allostasis and interoception, there is increasing evidence that therapeutic treatments that lower levels of inflammation contribute to intervention effectiveness for psychiatric morbidities (Franklin et al. 2018).
3.8 The Relationship Between Racism and Immune Function: A Review of Studies
Racial and ethnic disparities in inflammatory conditions are persistent, widespread consequences of chronic exposures to multiple forms of racism, from structural organization (i.e., segregation) to interpersonal social interactions (i.e., microaggressions) in the United States. Specifically, Black Americans, American Indians, Alaska Natives, and members of certain Hispanic groups are at disproportionately higher risk for inflammatory conditions including metabolic syndrome, diabetes, hypertension, cardiovascular disease, and obesity (see Goosby et al. 2018). In addition to linking interpersonal and self-reported discrimination to risk for these inflammatory conditions, the disparities literature has also linked discrimination to inflammatory biomarkers that are considered risk factors for, or indicators of, chronic disease. Specifically, interpersonal discrimination has been associated with several biomarkers of inflammation (e.g., C‑reactive protein, IL‑6, soluble urokinase plasminogen activator receptor, and composite indices of proinflammatory cytokines; Chen et al. 2022; Cuevas et al. 2020; Goosby et al. 2015; Toussaint et al. 2022). More recent literature has begun linking explicit indicators of systemic racism to inflammatory conditions. For instance, some of these inflammatory outcomes (e.g., depression, cancer, asthma) have been linked to indicators such as neighborhood deprivation due to enforced neighborhood racial segregation, historical redlining, neighborhood-level racism (Bailey et al. 2021; Plascak et al. 2022; Russell et al. 2018); environmental racism and pollutant exposure (Martinez et al. 2021); police violence and contact with the carceral state (Bailey et al. 2021; Sewell 2017; Sewell et al. 2021); and racialized political disenfranchisement (Homan and Brown 2022).Footnote 8
For many of these studies, the theoretical underpinnings integrate a chronic stress perspective, which proposes bodies with patterns of upregulated physiological systems in preparation for the uncertainties and vicissitudes that come with a life circumscribed and channeled by the perniciousness of racism and discrimination. When bodies fail to be successfully “down regulated”, systematic wear and tear can give rise to allostatic load (Chae et al. 2011, 2019) and eventually to allostatic overload (Bobba-Alves et al. 2022). Consequently, SCI entails the shift from short-term to long-term immune activation, causing potentially damaging alterations to tissues and organs (Furman et al. 2019). In this and other ways, adverse social conditions are realized in bodies, adding to burdens and increasing life challenges. Returning to Fig. 1, social systems underwrite environmental conditions, opportunities, and affordances that place demands upon bodies both directly and through brain-mediated experiences, as depicted in Fig. 3 (see Cheadle et al. 2024, this issue). Consequently, the adversities from outside the body become embodied, shaping both the way individuals experience their social realities and the changing capacities of their bodies through time as the diverse signaling dynamics of the immune and other systems (e.g., Fig. 2), which attempt to protect the body, instead come to take a toll, too often realized in patterns of physiological and psychological weathering (e.g., Geronimus et al. 2006).
4 Discussion
We began with the notions of CRT and systemic racism in part because they cannot be understood just in parts; to be fully appreciated, they must also be understood as complex systems (Stewart 2023), a gestalt. While it is certainly possible to study how racism in one system affects the groups and individuals within and passing through it, the theoretical richness of the conception must at some point transition from a deliberation on specific processes and mechanisms to a rumination on how they integrate and form a system in its entirety (e.g., McGilchrist 2019). In modeling complex phenomena, there is typically a trade-off between generality and precision of explanation. Highly specific models can often provide more detailed and accurate explanations in specific contexts, but at the cost of limited generalizability across phenomena. In contrast, more general models may better represent overall patterns and trends, but with less detail and accuracy, and potentially at the cost of precise causal inferences. This trade-off exists not only in modeling the physical mechanisms of social and cultural processes (e.g., micro, meso, and macro levels of analysis),- but also in modeling bodies (i.e., cellular mechanisms of a disease, the genetic substrates of cellular mechanisms), which are also cross- and multiscalar, complex, and dynamic. Like a society, bodies are themselves systems of systems, and the immune system seeks to maintain bodily integrity by limiting harms and protecting the body from the many ways the outside attempts to get in or from its own cells going off-script, while also fostering healing.
Social conditions, such as those organized for Black Americans by systemic racism, frequently enter the body through the brain by virtue of brain–body allostatic regulatory patterns, in addition to direct challenges from viruses, bacteria, toxins, damaged cells, etc. Why this happens has been expressed in the notion that “zebras don’t get ulcers” because their stress-regulation patterns are grounded in the moment and are thus temporally limitedFootnote 9 (Sapolsky 2004). Their experience at a narrow set of points in time is proposed to be a far cry from the kinds of chronic stressors over time that are common in the human world. Human stressors, whether ruminative, immediate, or prospective, are ultimately rooted in how the brain integrates information about the world outside with its understanding of its own states (i.e., interoception), which is reflected in the idea that the purpose of the brain is to anticipate the body’s needs to meet them before they arise (Sterling 2012; Hutchinson and Barrett 2019). One consequence of this capacity for humans with long memories and anticipatory brains that are frequently engaged with simulating potential futures (Seth 2021) is that the body is regulated for the potential that it will come to harm. Whatever cognitions we hold, this, at its core, is why stress is physiological. A key part of this regulatory dynamic is that the immunologic systems protecting the body from that which is outside are modulated as if there is potential for injury, even if the stressor is psychological in nature and existential, with the risk of actual physical harm being low.
A critical component of biologically informed health inequities research has been the integration of biological markers into population health research, by which inflammatory markers have become an important topic of sociological inquiry (Harris and Schorpp 2018). The inspiration for much of this work has been an expanding body of evidence elaborating the biology of chronic disease pathways and the development of low-cost, generally noninvasive biomarkers. The inclusion of expanding panels of available biomarkers has led to insights into health as outcome and consequence, and as predictor and mediator, of chronic morbidity and mortality. Consequently, social science researchers are growing more comfortable analyzing inflammatory markers (e.g., cytokines) while incorporating some of the underlying mechanistic explanations for why some markers appear to vary along social gradients and why they matter for morbidity and mortality. These findings, which can be complex and are not always intuitive, are critical for elaborating the linkages between social conditions (e.g., racism and discrimination) and health. However, it is not completely clear what is missing with a narrow focus on either cross-sectional biomarkers or by measuring only a few markers separated over long periods of calendar time, measurements that are thus dissociated from both system and temporal dynamics and contexts.
For example, McDade (2023) recently provided a compelling argument that community studies around the world demonstrate that conclusions based on affluent, industrialized populations cannot be applied globally and that the assumptions that aging processes leading to morbidity and mortality begin in middle age and that inflammation is pathological are probably wrong. Instead, he argues that there is substantial variation in levels of inflammation and patterns of association with disease by virtue of differing nutritional, microbial, and psychosocial environments in infancy and childhood, which play important roles in shaping inflammatory phenotypes and their contributions to diseases of aging. Key to his argument is the demonstration, when more measures are collected over time (e.g., multiple assays over a month), of acute patterns of inflammatory activity with rapid rises and decreases when compared to Western industrialized patterns of flat, low-grade inflammation. Moreover, more advanced technologies such as field-friendly cell culture methods, which are both needed and coming online, determine how immunity functions dynamically in the presence of real-world environmental conditions in the natural setting (McDade et al. 2021). Moreover, it was not until relatively recently that cytokines and other inflammatory markers were broadly available for use in the kinds of large data collections many sociologists prioritize (McDade et al. 2007). In addition, advances in immunomics and bioinformatics may provide new ways to both model inflammatory systems and draw causal inferences about those dynamics with respect to specific outcomes (Bonaguro et al. 2022).
Notably absent in the research on inflammation, however, has been a larger integration that interweaves two of the most complex and deeply interconnected systems in the human bodyFootnote 10: the immune system and the brain, the latter playing a key role in preparing the body for the world the brain attempts to anticipate. Theoretically, such a conceptualization is key to understanding both how a brain maintains its body and how social environments affect that interplay, and how such patterns influence feeling and behavior—which is to motivate a nondualistic view of the mind and body and thus physical and mental health. In many respects, we have simply sought to reemphasize the immune system in relation to its larger systemic integrations, a view inspired by McEwen (1998)Footnote 11 but which, in our view, has been largely deprioritized and undertheorized in favor of the ease with which his work motivates summary statistics of composite biological variables (i.e., allostatic load; Carbone et al. 2022; McEwen 1998).
5 Conclusion
As sociology increasingly borrows from and incorporates insights from the biological and biomedical sciences, we hope sociologists will continue to consider complex system dynamics, not just socially but also in terms of bodies within social structures and social systems. At the outset, this task is complicated by the complexity of the details. At the same time, the disciplines that have contributed the most information on the immune system, for example, also tend to emphasize and prioritize mechanisms at ever smaller scales as technology makes more precise experimental designs and greater control feasible, in service to causal inference. But there are complex interplays among processes and mechanisms within and across systems that cannot be seen only by zooming in, and which, as with sociology, can be understood only by zooming out. Biosociological perspectives have promise for providing important insights into how immune activity both contributes to disease risk and influences how we experience the world as expressed through the material reality of our bodies, but that is often a problem not of independent mechanisms but of interdependent mechanisms. Our social worlds are written upon us through the ways our bodies are regulated vis-à-vis the demands of the environments we inhabit and pass through, including how we prepare for those milieus we expect to encounter in the future, altering the very systems that comprise us and thus our health (Arnaldo et al. 2022; Bobba-Alves et al. 2022). This conception of immune system and inflammatory activity is necessary for creating an integrative biosocial theory that is transportable and applies across—and to some extent mirrors—different domains of the larger sociological project.
Notes
The goal of these methods is improved causal inference and precision medicine (De Domenico et al. 2020).
While this review focuses explicitly on CRT as it relates to the conditions of Black Americans’ unique experiences, it is important to note that adaptations of this framework were developed, in parallel and not long after, to theoretically examine the oppressive social structures of other racialized and ethnic minorities (e.g., LatCrit for Latine populations integrating concepts of immigration and nativism, and Tribal Crit for situating the legacy of colonization and genocide). Although these frameworks are beyond the scope of this paper, it is worth noting that the scale of the economic, political, and other consequences, particularly among Indigenous Americans (e.g., morbidity and mortality rates, economic marginalization, carceral contact), are also profound.
Though the innate system has been characterized as unable to “memorize” the characteristics of new pathogens, there is increasing evidence indicating that innate immunity also has adaptive characteristics, termed trained immunity (Netea et al. 2016, 2017). This literature is still in its early stages but indicates how our understanding of the immune system is far from complete and is continuing to evolve and perhaps even transform.
Pattern recognition receptors function largely like an ecology of Lego pieces, some of which fit together (i.e., receptors). Each one has its own unique set of immune blocks (i.e., immune diversity) that can interact with the structures of other “objects,” identifying invasive antigens via PRRs and attacking those antigens with specific profiles based on innate and adaptive immunity.
In some cases, the immune system mistakenly identifies its own receptors, or other self-proteins, as foreign and launches attacks upon them, initiating autoimmune diseases that lead to chronic inflammation and tissue damage in various parts of the body. The immune system may also mistakenly attack enzymes or structural proteins. The mechanisms underlying autoimmune diseases are complex and multifactorial, and different autoimmune diseases can involve different types of immune cells and molecular pathways.
The adult human body contains roughly 28 and 36 trillion cells for females and males, respectively, and roughly 17 trillion in children (Hatton et al. 2023), so it is not surprising that things are going wrong all the time.
The concept of “inflammaging” is employed to characterize chronic low-grade sterile inflammation with circulating blood levels of inflammatory markers and immune proteins to evaluate organ and system functioning and morbidity and mortality risks (Ferrucci and Fabbri 2018; Franceschi et al. 2018). In both animal and human models, the biological linkages of social conditions and relationships to health and longevity via immunologic function are strongly supported (Snyder-Mackler et al. 2020).
There is a growing literature employing epigenetic aging clocks as indicators of biological aging via DNA methylation and indicators of morbidity and mortality risk, but these are beyond the scope of this paper. Some of the racial differences in these clocks as outcomes are associated with socially inequitable conditions such as school segregation, poor living, neighborhood circumstances, and stressful life events (Martz et al. 2024; Raffington et al. 2023; Sumner et al. 2023). There is recent support that methylation profiled trained on CpG sites associated adult CRP contributed to the relationship between stressful life events and cognitive outcomes in children and adolescents. Predictive links between methylation profiles and morbidity over the life course are mixed (Meier et al. 2023) but speak to the importance of understanding these dynamics over the life course and across systems.
This idea is perhaps an idealization based on long periods of environmental stability. A zebra, like any other organism, in times of rapid ecological change when fitness is challenged no doubt experiences chronic stress, a dire situation in many ecologies due to human encroachment and climate change. Humans, even with physical needs met, have the capacity for all kinds of distress simply by imagining potential futures or exhuming the past.
Absent here but relevant is the gut or “second brain” and microbiome. For a sociological perspective, see Ignatow (2021).
Here it is worth noting that we also have important differences from McEwen’s work, which tends toward pathologizing health physiology. We find Sterling (2012) to be more compelling in this regard with his emphasis that bodies do what they are supposed to do given the conditions in their embedding environments. In other words, the problem is in the social systems and patterns of inequalities that make demands that human brains and bodies are generally not adapted for, and so the actual pathologies underlying much health inequity are social. For a recent elaboration on this perspective, see Sterling (2020).
References
Ahmed, E., and A. H. Hashish. 2006. On modelling the immune system as a complex system. Theory in Biosciences 124(3):413–418.
Ajilore, Olusola, and April D. Thames. 2020. The Fire This Time: The Stress of Racism, Inflammation and COVID-19. Brain, Behavior, and Immunity 88:66–67.
Al Kibria, Gulam Muhammed. 2019. Racial/Ethnic Disparities in Prevalence, Treatment, and Control of Hypertension among US Adults Following Application of the 2017 American College of Cardiology/American Heart Association Guideline. Preventive Medicine Reports 14:100850.
Alexander, Michelle. 2020. The New Jim Crow: Mass Incarceration in the Age of Colorblindness. New York: The New Press.
Alexander, Taifha, LaToya Baldwin Clark, Kyle Reinhard and Noah Zatz. 2023. CRT Forward: Tracking the Attack on Critical Race Theory. Los Angeles, CA: UCLA School of Law, Critical Race Studies.
Aneshensel, Carol S., and Uchechi A. Mitchell. 2014. The Stress Process: Its Origins, Evolution, and Future. In Sociology of Mental Health: Selected Topics from Forty Years 1970s–2010s, SpringerBriefs in Sociology, eds. Robert R. Johnson, R. Jay Turner and Bruce G. Link, 53–74. Cham: Springer International Publishing.
Arnaldo, Irene, Andrew W. Corcoran, Karl J. Friston and Maxwell J. D. Ramstead. 2022. Stress and Its Sequelae: An Active Inference Account of the Etiological Pathway from Allostatic Overload to Depression. Neuroscience & Biobehavioral Reviews 135:104590.
Bailey, Zinzi D., Nancy Krieger, Madina Agénor, Jasmine Graves, Natalia Linos and Mary T. Bassett. 2017. Structural Racism and Health Inequities in the USA: Evidence and Interventions. The Lancet 389(10077):1453–1463.
Bailey, Zinzi D., Justin M. Feldman and Mary T. Bassett. 2021. How Structural Racism Works—Racist Policies as a Root Cause of U.S. Racial Health Inequities. New England Journal of Medicine 384(8):768–773.
Barrett, Lisa Feldman. 2017. How Emotions Are Made: The Secret Life of the Brain. Boston: Houghton Mifflin Harcourt.
Barrett, Lisa Feldman, Karen S. Quigley and Paul Hamilton. 2016. An Active Inference Theory of Allostasis and Interoception in Depression. Philosophical Transactions of the Royal Society B: Biological Sciences 371(1708):20160011.
Barrows, Ian R., Ali Ramezani and Dominic S. Raj. 2019. Inflammation, Immunity, and Oxidative Stress in Hypertension—Partners in Crime? Advances in Chronic Kidney Disease 26(2):122–130.
Behnia, Faranak, Samantha Sheller and Ramkumar Menon. 2016. Mechanistic Differences Leading to Infectious and Sterile Inflammation. American Journal of Reproductive Immunology 75(5):505–518.
Bennett, Jeanette M., Glenn Reeves, George E. Billman and Joachim P. Sturmberg. 2018. Inflammation–Nature’s Way to Efficiently Respond to All Types of Challenges: Implications for Understanding and Managing ‘the Epidemic’ of Chronic Diseases. Frontiers in Medicine 5:316.
Bhat, Anjali, Thomas Parr, Maxwell Ramstead and Karl Friston. 2021. Immunoceptive Inference: Why Are Psychiatric Disorders and Immune Responses Intertwined? Biology & Philosophy 36(3):27.
Bobba-Alves, Natalia, Robert-Paul Juster and Martin Picard. 2022. The Energetic Cost of Allostasis and Allostatic Load. Psychoneuroendocrinology 146:105951.
Bonaguro, Lorenzo, Jonas Schulte-Schrepping, Thomas Ulas, Anna C. Aschenbrenner, Marc Beyer and Joachim L. Schultze. 2022. A Guide to Systems-Level Immunomics. Nature Immunology 23(10):1412–1423.
Bonilla-Silva, Eduardo. 1997. Rethinking Racism: Toward a Structural Interpretation. American Sociological Review 62(3):465–480.
Bonilla-Silva, Eduardo. 2015. The Structure of Racism in Color-Blind, ‘Post-Racial’ America. American Behavioral Scientist 59(11):1358–1376.
Bonilla-Silva, Eduardo. 2019. Toward a New Political Praxis for Trumpamerica: New Directions in Critical Race Theory. American Behavioral Scientist 63(13):1776–1788.
Byrne, Michelle L., Sarah Whittle and Nicholas B. Allen. 2016. The Role of Brain Structure and Function in the Association Between Inflammation and Depressive Symptoms: A Systematic Review. Psychosomatic Medicine 78(4):389–400.
Carbone, Jason T., Jenifer Clift and Nicholas Alexander. 2022. Measuring Allostatic Load: Approaches and Limitations to Algorithm Creation. Journal of Psychosomatic Research 163:111050.
Chae, David, Amani Nuru-Jeter, Karen Lincoln and Darlene Francis. 2011. Conceptualizing Racial Disparities in Health. Du Bois Review: Social Science Research on Race 8:63–77.
Chae, David H., Connor D. Martz, Thomas E. Fuller-Rowell, Erica C. Spears, Tianqi Tenchi Gao Smith, Evelyn A. Hunter, Cristina Drenkard and S. Sam Lim. 2019. Racial Discrimination, Disease Activity, and Organ Damage: The Black Women’s Experiences Living With Lupus (BeWELL) Study. American Journal of Epidemiology 188(8):1434–1443.
Cheadle, Jacob E., Bridget J. Goosby, Joseph C. Jochman, Cara C. Tomaso, Chelsea B. Kozikowski Yancey and Timothy D. Nelson. 2020. Race and Ethnic Variation in College Students’ Allostatic Regulation of Racism-Related Stress. Proceedings of the National Academy of Sciences 117(49):31053–31062.
Cheadle, Jacob E., K. J. Davidson-Turner and Bridget J. Goosby. 2024. Active Inference and Social Actors: Towards a Neuro-Bio-Social Theory of Brains and Bodies in Their Worlds. This issue.
Chen, Shyi-Jou, Yen-Ling Wang, Hueng-Chuen Fan, Wen-Tsung Lo, Chih-Chien Wang and Huey-Kang Sytwu. 2012. Current Status of the Immunomodulation and Immunomediated Therapeutic Strategies for Multiple Sclerosis. Clinical & Developmental Immunology 1–16.
Chen, Edith, Tianyi Yu, Gene H. Brody, Phoebe H. Lam, Bridget J. Goosby and Gregory E. Miller. 2022. Discrimination and Inflammation in Adolescents of Color. Biological Psychiatry Global Open Science 3(2):204–212.
Chen, Wen G., Dana Schloesser, Angela M. Arensdorf, Janine M. Simmons, Changhai Cui, Rita Valentino, James W. Gnadt, Lisbeth Nielsen, Coryse St Hillaire-Clarke, Victoria Spruance, Todd S. Horowitz, Yolanda F. Vallejo and Helene M. Langevin. 2021. The Emerging Science of Interoception: Sensing, Integrating, Interpreting, and Regulating Signals within the Self. Trends in Neurosciences 44(1):3–16.
Cheung, Vivian G., and Richard S. Spielman. 2009. Genetics of Human Gene Expression: Mapping DNA Variants That Influence Gene Expression. Nature Reviews Genetics 10(9):595–604.
Clark, Rodney, Norman B. Anderson, Vernessa R. Clark and David R. Williams. 1999. Racism as a Stressor for African Americans: A Biopsychosocial Model. American Psychologist 54(10):805–816.
Cohen, Sheldon, Denise Janicki-Deverts and Gregory E. Miller. 2007. Psychological Stress and Disease. JAMA 298(14):1685–1687.
Cuevas, Adolfo G., Anthony D. Ong, Keri Carvalho, Thao Ho, Sze Wan (Celine) Chan, Jennifer D. Allen, Ruijia Chen, Justin Rodgers, Ursula Biba and David R. Williams. 2020. Discrimination and Systemic Inflammation: A Critical Review and Synthesis. Brain, Behavior, and Immunity 89:465–479.
Dantzer, Robert. 2018. Neuroimmune Interactions: From the Brain to the Immune System and Vice Versa. Physiological Reviews 98(1):477–504.
De Domenico, Elena, Lorenzo Bonaguro, Jonas Schulte-Schrepping, Matthias Becker, Kristian Händler and Joachim L. Schultze. 2020. Optimized Workflow for Single-Cell Transcriptomics on Infectious Diseases Including COVID-19. STAR Protocols 1(3):100233.
Delgado, Richard, and Jean Stefancic. 2023. Critical Race Theory, Fourth Edition: An Introduction. 4th edition. New York: NYU Press.
D’Mello, Charlotte, and Mark G. Swain. 2017. Immune-to-Brain Communication Pathways in Inflammation-Associated Sickness and Depression. In Inflammation-Associated Depression: Evidence, Mechanisms and Implications, Current Topics in Behavioral Neurosciences, eds. Robert Dantzer and Lucile Capuron, 73–94. Cham: Springer International Publishing.
Dolina, Joseph S., Joey Lee, Eugene L. Moore, Jennifer L. Hope, Donald T. Gracias, Takaji Matsutani, Ashu Chawla, Jason A. Greenbaum, Joel Linden and Stephen P. Schoenberger. 2022. Developmentally Distinct CD4+ Treg Lineages Shape the CD8+ T Cell Response to Acute Listeria Infection. Proceedings of the National Academy of Sciences 119(10):e2113329119.
Eberl, Gérard. 2016. Immunity by Equilibrium. Nature Reviews Immunology 16(8):524–532.
Eisenberger, Naomi I., and Steve W. Cole. 2012. Social Neuroscience and Health: Neurophysiological Mechanisms Linking Social Ties with Physical Health. Nature Neuroscience 15(5):669–674.
Eisenberger, Naomi I., Mona Moieni, Tristen K. Inagaki, Keely A. Muscatell and Michael R. Irwin. 2017. In Sickness and in Health: The Co-Regulation of Inflammation and Social Behavior. Neuropsychopharmacology 42(1):242–253.
Ferrucci, Luigi, and Elisa Fabbri. 2018. Inflammageing: Chronic Inflammation in Ageing, Cardiovascular Disease, and Frailty. Nature Reviews Cardiology 15(9):505–505.
Franceschi, Claudio, Paolo Garagnani, Paolo Parini, Cristina Giuliani and Aurelia Santoro. 2018. Inflammaging: A New Immune–Metabolic Viewpoint for Age-Related Diseases. Nature Reviews Endocrinology 14(10):576–590.
Franklin, Tina C., Chelsea Xu and Ronald S. Duman. 2018. Depression and Sterile Inflammation: Essential Role of Danger Associated Molecular Patterns. Brain, Behavior, and Immunity 72:2–13.
Furman, David, Judith Campisi, Eric Verdin, Pedro Carrera-Bastos, Sasha Targ, Claudio Franceschi, Luigi Ferrucci, Derek W. Gilroy, Alessio Fasano, Gary W. Miller, Andrew H. Miller, Alberto Mantovani, Cornelia M. Weyand, Nir Barzilai, Jorg J. Goronzy, Thomas A. Rando, Rita B. Effros, Alejandro Lucia, Nicole Kleinstreuer and George M. Slavich. 2019. Chronic Inflammation in the Etiology of Disease across the Life Span. Nature Medicine 25(12):1822–1832.
Gaydosh, Lauren, Robert A. Hummer, Taylor W. Hargrove, Carolyn T. Halpern, Jon M. Hussey, Eric A. Whitsel, Nancy Dole and Kathleen Mullan Harris. 2019. The Depths of Despair Among US Adults Entering Midlife. American Journal of Public Health 109(5):774–780.
Geronimus, Arline T., Margaret Hicken, Danya Keene and John Bound. 2006. ‘Weathering’ and Age Patterns of Allostatic Load Scores Among Blacks and Whites in the United States. American Journal of Public Health 96(5):826–833.
Glass, Thomas A., and Matthew J. McAtee. 2006. Behavioral Science at the Crossroads in Public Health: Extending Horizons, Envisioning the Future. Social Science & Medicine 62(7):1650–1671.
Gong, Tao, Lei Liu, Wei Jiang and Rongbin Zhou. 2020. DAMP-Sensing Receptors in Sterile Inflammation and Inflammatory Diseases. Nature Reviews Immunology 20(2):95–112.
Goosby, Bridget J., Sarah Malone, Elizabeth Richardson, Jacob E. Cheadle, and Deadric Williams. 2015. Perceived Discrimination and Markers of Cardiovascular Risk among Low-Income African American Youth. American Journal of Human Biology 27(4):546–552.
Goosby, Bridget J., Jacob E. Cheadle and Colter Mitchell. 2018. Stress-Related Biosocial Mechanisms of Discrimination and African American Health Inequities. Annual Review of Sociology 44(1):319–340.
Graves Jr., Joseph L. 2001. The Emperor’s New Clothes: Biological Theories of Race at the Millennium. 1st edition. New Brunswick, NJ: Rutgers University Press.
Gurven, Michael D., and Daniel E. Lieberman. 2020. WEIRD Bodies: Mismatch, Medicine and Missing Diversity. Evolution and Human Behavior 41(5):330–340.
Hardeman, Rachel R., Patricia A. Homan, Tongtan Chantarat, Brigette A. Davis and Tyson H. Brown. 2022. Improving The Measurement Of Structural Racism To Achieve Antiracist Health Policy. Health Affairs 41(2):179–186.
Harris, Kathleen Mullan, and Kristen M. Schorpp. 2018. Integrating Biomarkers in Social Stratification and Health Research. Annual Review of Sociology 44(1):361–386.
Hatton, Ian A., Eric D. Galbraith, Nono S. C. Merleau, Teemu P. Miettinen, Benjamin McDonald Smith and Jeffery A. Shander. 2023. The Human Cell Count and Size Distribution. Proceedings of the National Academy of Sciences 120(39):e2303077120.
van der Heijden, Charlotte D. C. C., Laszlo Groh, Samuel T. Keating, Charlotte Kaffa, Marlies P. Noz, Simone Kersten, Antonius E. van Herwaarden, Alexander Hoischen, Leo A. B. Joosten, Henri J. L. M. Timmers, Mihai G. Netea and Niels P. Riksen. 2020. Catecholamines Induce Trained Immunity in Monocytes In Vitro and In Vivo. Circulation Research 127(2):269–283.
Henderson, Sheree, and Rebecca Wells. 2021. Environmental Racism and the Contamination of Black Lives: A Literature Review. Journal of African American Studies 25(1):134–151.
Himmelstein, Mary S., Danielle M. Young, Diana T. Sanchez and James S. Jackson. 2015. Vigilance in the Discrimination-Stress Model for Black Americans. Psychology & Health 30(3):253–267.
Hobson, Joanna M., Myles D. Moody, Robert E. Sorge and Burel R. Goodin. 2022. The Neurobiology of Social Stress Resulting from Racism: Implications for Pain Disparities among Racialized Minorities. Neurobiology of Pain 12:100101.
Homan, Patricia A., and Tyson H. Brown. 2022. Sick And Tired Of Being Excluded: Structural Racism In Disenfranchisement As A Threat To Population Health Equity. Health Affairs 41(2):219–227.
Hong, Seokmann, and Luc Van Kaer. 1999. Immune Privilege. The Journal of Experimental Medicine 190(9):1197–1200.
Hostinar, Camelia E., and Megan R. Gunnar. 2017. Future Directions in the Study of Social Relationships as Regulators of the HPA Axis Across Development. In Future Work in Clinical Child and Adolescent Psychology, ed. Mitchell J. Prinstein, 333–344. London: Routledge.
Hutchinson, J. Benjamin, and Lisa Feldman Barrett. 2019. The Power of Predictions: An Emerging Paradigm for Psychological Research. Current Directions in Psychological Science 28(3):280–291.
Ignatow, Gabe. 2021. Cognitive Sociology after Relational Biology. Sociological Forum 36(S1):1253–1270.
Iob, Eleonora, and Andrew Steptoe. 2019. Cardiovascular Disease and Hair Cortisol: A Novel Biomarker of Chronic Stress. Current Cardiology Reports 21(10):116.
Jawa, Randeep S., Sergio Anillo, Kristin Huntoon, Heinz Baumann and Mahmoud Kulaylat. 2011. Analytic Review: Interleukin‑6 in Surgery, Trauma, and Critical Care: Part I: Basic Science. Journal of Intensive Care Medicine 26(1):3–12.
Jelsma, Elizabeth B., Bridget J. Goosby and Jacob E. Cheadle. 2021. Do Trait Psychological Characteristics Moderate Sympathetic Arousal to Racial Discrimination Exposure in a Natural Setting? Psychophysiology 58(4):e13763.
Joseph, Joshua J., and Sherita H. Golden. 2017. Cortisol Dysregulation: The Bidirectional Link between Stress, Depression, and Type 2 Diabetes Mellitus. Annals of the New York Academy of Sciences 1391(1):20–34.
Kendi, Ibram X. 2016. Stamped from the Beginning: The Definitive History of Racist Ideas in America. First Edition. New York: Bold Type Books.
Kinney, Jefferson W., Shane M. Bemiller, Andrew S. Murtishaw, Amanda M. Leisgang, Arnold M. Salazar and Bruce T. Lamb. 2018. Inflammation as a Central Mechanism in Alzheimer’s Disease. Alzheimer’s & Dementia: Translational Research & Clinical Interventions 4:575–590.
Kipnis, Jonathan, and Anthony J. Filiano. 2018. The Central Nervous System: Privileged by Immune Connections. Nature Reviews Immunology 18(2):83–84.
Link, Bruce G., and Jo Phelan. 1995. Social Conditions As Fundamental Causes of Disease. Journal of Health and Social Behavior 80–94.
Lord, Brittany D., Alexandra R. Harris and Stefan Ambs. 2023. The Impact of Social and Environmental Factors on Cancer Biology in Black Americans. Cancer Causes & Control 34(3):191–203.
Marshall, Jean S., Richard Warrington, Wade Watson and Harold L. Kim. 2018. An Introduction to Immunology and Immunopathology. Allergy, Asthma & Clinical Immunology 14(2):49.
Martinez, Adali, Rosemarie de la Rosa, Mahasin Mujahid and Neeta Thakur. 2021. Structural Racism and Its Pathways to Asthma and Atopic Dermatitis. Journal of Allergy and Clinical Immunology 148(5):1112–1120.
Martz, Connor D., Aprile D. Benner, Bridget J. Goosby, Colter Mitchell and Lauren Gaydosh. 2024. Structural Racism in Primary Schools and Changes in Epigenetic Age Acceleration among Black and White Youth. Social Science & Medicine 116724.
Massey, Douglas, and Nancy Denton. 1993. American Apartheid: Segregation and the Making of the Underclass. Cambridge, MA: Harvard University Press.
McDade, Thomas W. 2023. Three Common Assumptions about Inflammation, Aging, and Health That Are Probably Wrong. Proceedings of the National Academy of Sciences 120(51):e2317232120.
McDade, Thomas W., Sharon Williams and J. Josh Snodgrass. 2007. What a Drop Can Do: Dried Blood Spots as a Minimally Invasive Method for Integrating Biomarkers into Population-Based Research. Demography 44(4):899–925.
McDade, Thomas W., Alexander V. Georgiev and Christopher W. Kuzawa. 2016. Trade-Offs between Acquired and Innate Immune Defenses in Humans. Evolution, Medicine, and Public Health 2016(1):1–16.
McDade, Thomas W., Jacob E. Aronoff, Adam K. K. Leigh, Eric D. Finegood, Rachel M. Weissman-Tsukamoto, Gene H. Brody and Gregory E. Miller. 2021. Out of the Laboratory and Into the Field: Validation of Portable Cell Culture Protocols. Psychosomatic Medicine 83(3):283.
McEwen, Bruce S. 1998. Stress, Adaptation, and Disease: Allostasis and Allostatic Load. Annals of the New York Academy of Sciences 840(1):33–44.
McEwen, Bruce S., and Peter J. Gianaros. 2010. Central Role of the Brain in Stress and Adaptation: Links to Socioeconomic Status, Health, and Disease. Annals of the New York Academy of Sciences 1186(1):190–222.
McGilchrist, Iain. 2019. The Master and His Emissary: The Divided Brain and the Making of the Western World. 2nd edition. New Haven, CT: Yale University Press.
McLaughlin, Katie A., Kiara Alvarez, Mirko Fillbrunn, Jennifer Greif Green, James S. Jackson, Ronald C. Kessler, Ekaterina Sadikova, Nancy A. Sampson, Corrie L. Vilsaint, David R. Williams and Margarita Alegría. 2019. Racial/Ethnic Variation in Trauma-Related Psychopathology in the United States: A Population-Based Study. Psychological Medicine 49(13):2215–2226.
Meier, Helen C. S., Colter Mitchell, Thomas Karadimas and Jessica D. Faul. 2023. Systemic Inflammation and Biological Aging in the Health and Retirement Study. GeroScience 45(6):3257–3265.
Michopoulos, Vasiliki, Abigail Powers, Charles F. Gillespie, Kerry J. Ressler and Tanja Jovanovic. 2017. Inflammation in Fear- and Anxiety-Based Disorders: PTSD, GAD, and Beyond. Neuropsychopharmacology 42(1):254–270.
Mills, Charles W. 2022. The Racial Contract. 25th Anniversary edition. Ithaca, NY: Cornell University Press.
Montez, Jennifer Karas, Mark D. Hayward and Anna Zajacova. 2021. Trends in U.S. Population Health: The Central Role of Policies, Politics, and Profits. Journal of Health and Social Behavior 62(3):286–301.
Muhammad, Khalil Gibran. 2019. The Condemnation of Blackness: Race, Crime, and the Making of Modern Urban America. 1st Edition. Cambridge, MA: Harvard University Press.
Muriach, María, Miguel Flores-Bellver, Francisco J. Romero and Jorge M. Barcia. 2014. Diabetes and the Brain: Oxidative Stress, Inflammation, and Autophagy. Oxidative Medicine and Cellular Longevity 2014:e102158.
Netea, Mihai G., Leo A. B. Joosten, Eicke Latz, Kingston H. G. Mills, Gioacchino Natoli, Hendrik G. Stunnenberg, Luke A. J. O’Neill and Ramnik J. Xavier. 2016. Trained Immunity: A Program of Innate Immune Memory in Health and Disease. Science 352(6284):aaf1098.
Netea, Mihai G., Frances Balkwill, Michel Chonchol, Fabio Cominelli, Marc Y. Donath, Evangelos J. Giamarellos-Bourboulis, Douglas Golenbock, Mark S. Gresnigt, Michael T. Heneka, Hal M. Hoffman, Richard Hotchkiss, Leo A. B. Joosten, Daniel L. Kastner, Martin Korte, Eicke Latz, Peter Libby, Thomas Mandrup-Poulsen, Alberto Mantovani, Kingston H. G. Mills, Kristen L. Nowak, Luke A. O’Neill, Peter Pickkers, Tom van der Poll, Paul M. Ridker, Joost Schalkwijk, David A. Schwartz, Britta Siegmund, Clifford J. Steer, Herbert Tilg, Jos W. M. van der Meer, Frank L. van de Veerdonk and Charles A. Dinarello. 2017. A Guiding Map for Inflammation. Nature Immunology 18(8):826–831.
Nusslock, Robin, and Gregory E. Miller. 2016. Early-Life Adversity and Physical and Emotional Health Across the Lifespan: A Neuroimmune Network Hypothesis. Biological Psychiatry 80(1):23–32.
Osei, Kwame, and Trudy Gaillard. 2017. Disparities in Cardiovascular Disease and Type 2 Diabetes Risk Factors in Blacks and Whites: Dissecting Racial Paradox of Metabolic Syndrome. Frontiers in Endocrinology 8.
Plascak, Jesse J., Kirsten Beyer, Xinyi Xu, Antoinette M. Stroup, Gabrielle Jacob and Adana A. M. Llanos. 2022. Association Between Residence in Historically Redlined Districts Indicative of Structural Racism and Racial and Ethnic Disparities in Breast Cancer Outcomes. JAMA Network Open 5(7):e2220908.
Protein Lounge. 2024. Pathways: Cytokine Network. https://proteinlounge.com/cytokine-network-pg-176.html (Accessed 4 Nov. 2023).
Quadt, Lisa, Hugo D. Critchley and Sarah N. Garfinkel. 2018. The Neurobiology of Interoception in Health and Disease: Neuroscience of Interoception. Annals of the New York Academy of Sciences 1428(1):112–128.
Raffington, Laurel, Peter T. Tanksley, Aditi Sabhlok, Liza Vinnik, Travis Mallard, Lucy S. King, Bridget Goosby, K. Paige Harden and Elliot M. Tucker-Drob. 2023. Socially Stratified Epigenetic Profiles Are Associated With Cognitive Functioning in Children and Adolescents. Psychological Science 34(2):170–185.
Ray, Victor. 2019. A Theory of Racialized Organizations. American Sociological Review 84(1):26–53.
Ray, Victor. 2022. On Critical Race Theory: Why It Matters & Why You Should Care. New York: Random House.
Renna, Megan E. 2021. A Review and Novel Theoretical Model of How Negative Emotions Influence Inflammation: The Critical Role of Emotion Regulation. Brain, Behavior, & Immunity—Health 18:100397.
Reskin, Barbara. 2012. The Race Discrimination System. Annual Review of Sociology 38(1):17–35.
Rodriguez, Javier M., Arline T. Geronimus, John Bound and Danny Dorling. 2015. Black Lives Matter: Differential Mortality and the Racial Composition of the U.S. Electorate, 1970–2004. Social Science & Medicine 136–137:193–199.
Roh, Jong Seong, and Dong Hyun Sohn. 2018. Damage-Associated Molecular Patterns in Inflammatory Diseases. Immune Network 18(4):e27.
Rohleder, Nicolas. 2019. Stress and Inflammation—The Need to Address the Gap in the Transition between Acute and Chronic Stress Effects. Psychoneuroendocrinology 105:164–171.
Russell, Daniel W., Frederick D. Clavél, Carolyn E. Cutrona, W. Todd Abraham and Rebecca G. Burzette. 2018. Neighborhood Racial Discrimination and the Development of Major Depression. Journal of Abnormal Psychology 127(2):150–159.
Sapolsky, Robert M. 2004. Why Zebras Don’t Get Ulcers, Third Edition. 3rd edition. New York: Holt Paperbacks.
Savitz, Jonathan, and Neil A. Harrison. 2018. Interoception and Inflammation in Psychiatric Disorders. Biological Psychiatry. Cognitive Neuroscience and Neuroimaging 3(6):514–524.
Schmidt, Angelika, Nina Oberle, Eva-Maria Weiß, Diana Vobis, Stefan Frischbutter, Ria Baumgrass, Christine S. Falk, Mathias Haag, Britta Brügger, Hongying Lin, Georg W. Mayr, Peter Reichardt, Matthias Gunzer, Elisabeth Suri-Payer and Peter H. Krammer. 2011. Human Regulatory T Cells Rapidly Suppress T Cell Receptor–Induced Ca2+, NF-κB, and NFAT Signaling in Conventional T Cells. Science Signaling 4(204):ra90–ra90.
Schulkin, Jay, and Peter Sterling. 2019. Allostasis: A Brain-Centered, Predictive Mode of Physiological Regulation. Trends in Neurosciences 42(10):740–752.
Seth, Anil. 2021. Being You: A New Science of Consciousness. London: Faber & Faber.
Sewell, Abigail A. 2017. The Illness Associations of Police Violence: Differential Relationships by Ethnoracial Composition. Sociological Forum 32(S1):975–997.
Sewell, Alyasah Ali, Justin M. Feldman, Rashawn Ray, Keon L. Gilbert, Kevin A. Jefferson and Hedwig Lee. 2021. Illness Spillovers of Lethal Police Violence: The Significance of Gendered Marginalization. Ethnic and Racial Studies 44(7):1089–1114.
Smith, Sean M., and Wylie W. Vale. 2006. The Role of the Hypothalamic-Pituitary-Adrenal Axis in Neuroendocrine Responses to Stress. Dialogues in Clinical Neuroscience 8(4):383–395.
Snyder-Mackler, Noah, Joseph Robert Burger, Lauren Gaydosh, Daniel W. Belsky, Grace A. Noppert, Fernando A. Campos, Alessandro Bartolomucci, Yang Claire Yang, Allison E. Aiello, Angela O’Rand, Kathleen Mullan Harris, Carol A. Shively, Susan C. Alberts and Jenny Tung. 2020. Social Determinants of Health and Survival in Humans and Other Animals. Science 368(6493):eaax9553.
Stanley, Amanda C., and Paige Lacy. 2010. Pathways for Cytokine Secretion. Physiology 25(4):218–229.
Sterling, Peter. 2012. Allostasis: A Model of Predictive Regulation. Physiology & Behavior 106(1):5–15.
Sterling, Peter. 2015. Principles of Neural Design. Cambridge, MA: The MIT Press.
Sterling, Peter. 2020. What Is Health? Allostasis and the Evolution of Human Design. Cambridge, MA: The MIT Press.
Stewart, Quincy Thomas. 2023. Race in the Machine: A Novel Account. 1st edition. Moorabin, VIC: Redwood Press.
Sumner, Jennifer A., Xu Gao, Simone Gambazza, Christian K. Dye, Natalie L. Colich, Andrea A. Baccarelli, Monica Uddin and Katie A. McLaughlin. 2023. Stressful Life Events and Accelerated Biological Aging over Time in Youths. Psychoneuroendocrinology 151:106058.
Thomas-Vaslin, Véronique. 2017. Understanding and Modeling the Complexity of the Immune System. In First Complex Systems Digital Campus World E‑Conference 2015, Springer Proceedings in Complexity, eds. Paul Bourgine, Pierre Collet and Pierre Parrend, 261–270. Cham: Springer International Publishing.
Toussaint, Loren L., Daniel P. Moriarity, Shanmukh Kamble, David R. Williams and George M. Slavich. 2022. Inflammation and Depression Symptoms Are Most Strongly Associated for Black Adults. Brain, Behavior, & Immunity—Health 26:100552.
Turnbull, Andrew V., and Catherine L. Rivier. 1999. Regulation of the Hypothalamic-Pituitary-Adrenal Axis by Cytokines: Actions and Mechanisms of Action. Physiological Reviews 79(1):1–71.
Turner, Anne I., Nina Smyth, Sarah J. Hall, Susan J. Torres, Mais Hussein, Sisitha U. Jayasinghe, Kylie Ball and Angela J. Clow. 2020. Psychological stress reactivity and future health and disease outcomes: A systematic review of prospective evidence. Psychoneuroendocrinology 114:104599.
Uchima, Olivia, Yan Yan Wu, Colette Browne and Kathryn L. Braun. 2019. Disparities in Diabetes Prevalence Among Native Hawaiians/Other Pacific Islanders and Asians in Hawai‘i. Preventing Chronic Disease 16:E22.
Umberson, Debra, Julie Skalamera Olson, Robert Crosnoe, Hui Liu, Tetyana Pudrovska and Rachel Donnelly. 2017. Death of Family Members as an Overlooked Source of Racial Disadvantage in the United States. Proceedings of the National Academy of Sciences of the United States of America 114(5):915–920.
Wenbo, Li, and Jin Wang. 2017. Uncovering the Underlying Mechanism of Cancer Tumorigenesis and Development under an Immune Microenvironment from Global Quantification of the Landscape. Journal of The Royal Society Interface 14:20170105.
Wheaton, Blair. 1994. Sampling the Stress Universe. In Stress and Mental Health: Contemporary Issues and Prospects for the Future, The Springer Series on Stress and Coping, eds. William R. Avison and Ian H. Gotlib, 77–114. Boston, MA: Springer US.
Williams, David R. 2018. Stress and the Mental Health of Populations of Color: Advancing Our Understanding of Race-Related Stressors. Journal of Health and Social Behavior 59(4):466–485.
Williams, Monnica T. 2020. Microaggressions: Clarification, Evidence, and Impact. Perspectives on Psychological Science 15(1):3–26.
Woolf, Steven H., Ryan K. Master and Laudan Y. Aron. 2022. Changes in Life Expectancy Between 2019 and 2020 in the US and 21 Peer Countries. JAMA Network Open 5(4):e227067.
Wrigley-Field, Elizabeth. 2020. US Racial Inequality May Be as Deadly as COVID-19. Proceedings of the National Academy of Sciences 117(36):21854–56.
Yang, Yang Claire, Courtney Boen, Karen Gerken, Ting Li, Kristen Schorpp and Kathleen Mullan Harris. 2016. Social Relationships and Physiological Determinants of Longevity across the Human Life Span. Proceedings of the National Academy of Sciences 113(3):578–583.
Youwakim, Jessica, and Hélène Girouard. 2021. Inflammation: A Mediator Between Hypertension and Neurodegenerative Diseases. American Journal of Hypertension 34(10):1014–1030.
Zefferino, Roberto, Sante Di Gioia and Massimo Conese. 2021. Molecular Links between Endocrine, Nervous and Immune System during Chronic Stress. Brain and Behavior 11(2):e01960.
Zhang, Amy, Bridget J. Goosby and Jacob E. Cheadle. 2021. In the Flow of Life: Capturing Affective Socializing Dynamics Using a Wearable Sensor and Intensive Daily Diaries. Socius 7:23780231211064009.
Zheng, Haixia, Ryan Smith, Kaiping Burrows, Rayus Kuplicki, Jerzy Bodurka, T. Kent Teague, Martin Paulus, Sahib Khalsa and Jonathan Savitz. 2021. Inflammation Is Associated With Abnormal Interoceptive Processing in Major Depressive Disorder. Biological Psychiatry 89(9, Supplement):S190–191.
Funding
This research was supported by grant P30AG066614, awarded to the Center on Aging and Population Sciences at The University of Texas at Austin by the National Institute on Aging, and by grant P2CHD042849, awarded to the Population Research Center at The University of Texas at Austin by the Eunice Kennedy Shriver National Institute of Child Health and Human Development. The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or The University of Texas at Austin.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
B. J. Goosby and J. E. Cheadle declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Goosby, B.J., Cheadle, J.E. The Immune System Is a Complex System: Inflammatory Morbidity and Systemic Racism. Köln Z Soziol (2024). https://doi.org/10.1007/s11577-024-00952-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11577-024-00952-4