Abstract
Purpose
Tuberculosis is a major global health threat claiming millions of lives each year. While the total number of tuberculosis cases has been decreasing over the last years, the rise of drug-resistant tuberculosis has reduced the chance of controlling the disease. The purpose is to implement a timely diagnosis of drug-resistant tuberculosis, which is essential to administering adequate treatment regimens and stopping the further transmission of drug-resistant tuberculosis.
Methods
A main tool for diagnosing tuberculosis is the conventional chest X-ray. We are investigating the possibility of discriminating automatically between drug-resistant and drug-sensitive tuberculosis in chest X-rays by means of image analysis and machine learning methods.
Results
For discriminating between drug-sensitive and drug-resistant tuberculosis, we achieve an area under the receiver operating characteristic curve (AUC) of up to 66%, using an artificial neural network in combination with a set of shape and texture features. We did not observe any significant difference in the results when including follow-up X-rays for each patient.
Conclusion
Our results suggest that a chest X-ray contains information about the likelihood of a drug-resistant tuberculosis infection, which can be exploited computationally. We therefore suggest to repeat the experiments of our pilot study on a larger set of chest X-rays.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Tuberculosis (TB) is a serious worldwide public health threat [1]. It is an airborne disease that is caused by mycobacterium tuberculosis (MTB) bacteria, which was first discovered in 1882 [2]. The worldwide TB mortality rate is decreasing due to a global effort to improve TB control and treatment. However, even today after the development of advanced medical treatment and diagnostic technology, TB is the leading cause of death from infectious disease in the world. About 9.6 million people are estimated to have TB, which claimed 1.5 million lives in 2014 alone.
Particularly, worrisome are the drug-resistant forms of tuberculosis. Multidrug-resistant TB (MDR-TB) is a form of tuberculosis that is resistant to treatment with one or two of the first-line anti-TB drugs (isoniazid and rifampicin). MDR-TB is concerning because it is difficult to diagnose and it takes more time (often more than two years) and cost to treat patients. About 3.3% of new TB cases and 20% of previously treated cases are estimated to have MDR-TB. Globally, the trend of drug-resistant tuberculosis has remained unchanged at best [3].
One of the major challenges for controlling MDR-TB lies in the difficulty in diagnosing drug resistance of TB-suspected patients during their first visit. Conventionally, drug susceptibility testing is performed on a sputum sample to identify the resistant status to several drugs, which requires a well-equipped laboratory facility and takes four to six weeks to obtain the laboratory results. The recent development of the Xpert MTB/RIF, a real-time test based on polymerase chain reaction (PCR) for genetic mutations in the MTB genome associated with resistance, specifically rifampicin (RIF) resistance, has greatly reduced the laboratory time needed for the detection of MDR-TB [1]. However, the test still produces a large number of inconclusive results and its deployment in resource-constrained settings is expensive. In addition, the test requires a sputum sample, which can be difficult to obtain, especially from children. Therefore, detecting MDR-TB is still a challenge and the conventional chest CXR (X-ray) remains a valuable tool in detection, screening and surveillance of MDR-TB, thanks to its widespread availability.
With the recent advances in imaging technology and computational methods for quantitative imaging, infectious disease imaging (IDI) has shown promising results in infectious disease diagnosis. IDI is an interdisciplinary field involving clinical research of infectious diseases under various imaging modalities, including CXR, computed tomography (CT), positron emission tomography (PET), magnetic resonance imaging (MRI), and other modalities. One goal is to leverage radiology for the diagnosis and treatment of emerging pathogens, epidemics and pandemics. Clinical imaging allows obtaining quantitative information and applying computer-assisted detection methods for assessing infectious disease severity and response to therapy. IDI, therefore, offers new ways of diagnosing infectious diseases effectively and accurately. For example, in H1N1 influenza diagnosis, computed tomography (CT) imaging of severe H1N1 contributed to earlier diagnosis and treatment of the infection by eliminating other possible causes of disease. For monitoring tuberculosis treatment, PET/CT scans were computationally evaluated and provided a volumetric assessment of TB-associated abnormalities, which were predictive of treatment outcomes [4].
We have structured the paper as follows: Background and previous work section describes the background of our work on discovering potential radiological features that could indicate drug resistance. Third section provides information about the set of CXRs we have acquired for our studies and presents our methods for lung segmentation, feature computation, and classification. Finally, fourth section shows our results, followed by a final conclusion summarizing the paper.
Background and previous work
Drug resistance
Tuberculosis is a curable infection. However, it requires a long treatment with several drugs (www.tbfacts.org). There are currently more than 20 drugs in use against TB. The five most commonly used drugs, which are also called first-line drugs, are typically used for TB patients without prior TB drug treatment. This includes the drugs isoniazid, rifampicin, and three others. It is essential that several TB drugs are being taken together to avoid becoming resistant to an individual drug. To avoid drug resistance, it is also very important that the patient adheres strictly to the treatment regimen over several months without interruptions.
The drugs for the treatment of drug-resistant TB are more expensive and have more side effects. They are grouped according to their effectiveness and experience of use, and belong to the so-called second-line drugs, which are the reserve drugs for treating drug resistance.
A patient with TB is drug-susceptible if the TB bacteria causing the infection respond to all drugs. If a patient has contracted drug-resistant TB, either from the direct transmission from another infected person or due to improper treatment, the TB bacteria will not respond to at least one of the main drugs. Two main types of drug resistance are MDR-TB and XDR-TB. MDR-TB, or multidrug resistant TB, is defined as resistance to at least isoniazid or rifampicin, which are two of the most effective first-line TB drugs. XDR-TB, or extensively drug-resistant TB, is caused by bacteria that, in addition to resistance against isoniazid or rifampicin, are resistant to additional drugs, including at least one of the second-line drugs. These are the two main types of TB drug resistance, although additional categories are sometimes used depending on the number of drugs that the bacteria do not respond to, including resistance against individual drugs and resistance against most of the existing drugs. Treatment of the latter is extremely difficult.
According to the latest WHO update on MDR-TB, there were an estimated 480,000 new cases of MDR-TB in 2015 [3]. Almost 10% of these cases are extensively drug-resistant (XDR-TB). To date, 117 countries have reported at least one XDR-TB case.
Previous work
There is evidence that differentiating between MDR-TB and drug-sensitive TB may be possible in computed tomography (CT). For example, Yeom et al. [5] found significant correlation of bilateral and multiple findings such as segmental or lobar consolidation and cavities with primary MDR-TB patients. Findings such as bilateral consolidations and multiple cavities were also evident in the CXRs of our MDR-TB patients, making them an ideal cohort for discrimination analysis (see “Methods and procedures” section).
Chen et al. [4] correlated PET/CT imaging with treatment outcome in patients with multidrug-resistant TB. They assessed changes at 2 and 6 months (CT only) in a cohort of 28 subjects with multidrug-resistant TB, who were treated with second-line TB therapy for 2 years and then followed for an additional 6 months. CT scans were read semiquantitatively by radiologists and were computationally evaluated using custom software to provide volumetric assessment of TB-associated abnormalities. Their results show that CT scans at 6 months (but not 2 months) assessed by radiologist readers were predictive of outcomes, and changes in computed abnormal volumes were predictive of drug response at both time points. In their cohort, some radiologic markers were more sensitive than conventional sputum microbiology in distinguishing successful from unsuccessful treatment. While these results support the potential of imaging scans, the authors admit that larger cohorts confirming these results are needed.
An early study by Cha et al. [6] was designed to describe radiological findings of XDR-TB and to compare the observed findings with the findings of drug-sensitive and MDR-TB in non-AIDS patients. Their conclusion was that by observation of multiple cavities, nodules, and bronchial dilatation as depicted in CT in young patients, the presence of MDR-TB or XDR-TB rather than drug-sensitive TB can be suggested. There was no significant difference in imaging findings between patients with XDR-TB and MDR-TB.
The result of Cha et al. confirmed the result of an even earlier study by Kim et al. [7], who observed that patients with MDR-TB had visible cavity formations on CT and concluded that multiple cavities suggest the possibility of MDR-TB. This is also consistent with a study by Chung et al. [8]. However, Lee et al. [9] concluded later that CT findings of XDR-TB are indeed similar to those of MDR-TB, but XDR-TB tends to have more extensive consolidation and tree-in-bud appearance.
Very little work has been done to discriminate between drug-sensitive and drug-resistant TB automatically by computational means, let alone achieving this for the common CXR. In an early pilot study, Kovalev et al. [10] observed statistically significant links between computerized features of radiological images and drug resistance status of TB patients. In a second study, the authors achieved an accuracy of more than 75% but only when combining CXR with CT features [11]. The performance for CXR features alone was much lower.
Methods and procedures
We process CXR images through a pipeline consisting of lung segmentation, feature computation, and classification.
Image acquisition and annotation
For our study, we are using CXR images from a patient database of the Republic of Belarus, where MDR/XDR-TB and HIV/TB are prevalent. In addition to the CXR images of all patients, the database includes laboratory work and clinical data. All images have been collected as part of Belarus’ compulsory lung screening program, in which the population is regularly screened for lung diseases. All patients had been admitted to the MDR-TB department of the Republic’s Scientific and Practical Center of Pulmonology and Tuberculosis (RSPCPT) with either already diagnosed or suspected MDR-TB. Each patient received a radiological examination not long after the date of registration. For image acquisition, the KODAK Point of Care 260 CR System with the KODAK Quality Control Software (Version 2.1.2.0.) has been used.
The 135 cases investigated in this paper consist of 45% sensitive (61) amd 54% MDR (74) cases. The gender distribution is 59% males (80) and 40% females (55). Among these patients, 61% (83) are younger than 50 years and 39% (52) are older than 50 years. Table 1 lists the data stratified according to age, gender, and type of resistance.
The data given in Table 1 will be the basis for our first experiment later in the paper, in which we use the initial CXR of each patient to discriminate between sensitive TB and MDR-TB. For these data, we measured no significant difference between the age and gender distributions among sensitive and resistant TB (z-test, with \(p=0.57\) and \(p=0.77\), respectively).
In our second experiment, we include the follow-up CXRs for each patient. Table 2 lists the number of CXRs of the second experiment stratified according to age, gender, and type of resistance. For the data of the second experiment, we measured again no significant difference between the age and gender distributions among sensitive and resistant TB (z-test, with \(p=0.19\) and \(p=0.71\), respectively).
Patients who had follow-up visits took additional CXRs during the visits. Sensitive patients had about four CXRs on average, and MDR-TB patients had an average of roughly three CXRs taken in comparison, see Table 3.
The time interval between CXRs is given in Table 4 as days between follow-up visits. On average, the sensitive TB patients had about 45-day intervals between visits and the MDR-TB patients had an average of 38 days between visits. Follow-up times vary depending on patients.
The sensitive TB patients received the standard WHO recommended TB regimens: ethambutol (e), isoniazid (h), rifampicin (r), and pyrazinamide (z) (Table 5).
For the MDR-TB patients, treatment regimens were prescribed based on drug-resistant tests in a microbiology laboratory. Therefore, each MDR-TB patient’s prescription differs and is a combination of several TB drugs, excluding regimens that were resistant. Frequently prescribed treatments were capreomycin (cm), cycloserine (cs), levofloxacin (lfx), p-aminosalicylic acid (pas), protionamide (pto), and pyrazinamide (z) (Table 6). Most of these patients were resistant to ethambutol (e), isoniazid (h), and rifampicin (r) of the standard TB regimen.
Lung segmentation
We detect lung boundaries in our CXRs using an atlas-based lung segmentation algorithm [12]. The algorithm uses existing CXRs and their manually delineated lung boundaries as models and estimates the unknown lung boundary of a patient’s CXR by registering the existing models to the patient’s CXR. As models, we use our public CXR dataset with reference lung boundaries [12, 13]. For a patient CXR, the algorithm first finds the most similar CXRs in the model set. We measure the similarity between CXRs by comparing the horizontal and vertical intensity histograms, which serve as rough shape descriptors of the lung, using the Bhattacharyya distance as a similarity measure. The main purpose of measuring the similarity is to limit the actual registration to the most similar models in order to reduce computational costs. After the model selection, we compute the correspondences between the model CXRs and the patient CXR. To do so, we create a correspondence map by first describing the patient CXR using local image features and then finding the most similar locations with a matching algorithm, following the SIFT flow approach [14]. The SIFT flow algorithm models local gradient information of the observed image using the scale-invariant feature transform (SIFT) [15]. Once we have calculated the SIFT features, the registration algorithm computes pixel-to-pixel correspondences by matching the SIFT features. The computed map of corresponding pixels between images then serves as a transformation matrix that we use to generate the approximate lung model for the patient CXR. We have shown that this algorithm produces state-of-the-art results for lung boundary detection on the public JSRT set [16], among others. For more details about the algorithm, we refer to [12]. Figure 1 shows two examples of lung boundaries detected by our method.
Feature computation
For our classification experiments, we use two different feature sets as described in the following. The first set is based on color, shape, and texture, whereas the second set is based on edge orientation.
Color, shape, and texture features To describe visual patterns indicating drug resistance or drug sensitivity in a segmented lung field, we use a feature set that we have successfully used in [17] to discriminate between TB-infected and uninfected lungs. It is a combination of shape, edge, and texture descriptors [18]. For each descriptor, we compute a histogram that shows the distribution of the different descriptor values across the lung field. Each histogram bin serves as a feature, and all features of all descriptors combined represent the feature vector input to a classifier. The following is a list of all descriptors we are using, with each descriptor quantized into 32 bins (see also [19,20,21]):
-
Intensity histograms (IH)
-
Gradient magnitude histograms (GM)
-
Shape descriptor histograms (SD) [22]
$$\begin{aligned} \hbox {SD} = \tan ^{-1}\left( \frac{\lambda _1}{\lambda _2}\right) , \end{aligned}$$(1)where \(\lambda _1\) and \(\lambda _2\) are the eigenvalues of the Hessian matrix, with \(\lambda _1 \le \lambda _2\).
-
Curvature descriptor histograms (CD) [22]
$$\begin{aligned} \hbox {CD} = \tan ^{-1}\left( \frac{\sqrt{\lambda _1^2 + \lambda _2^2}}{1+I(x,y)}\right) , \end{aligned}$$(2)with \(0 \le \hbox {CD} \le \pi /2\), where I(x, y) denotes the pixel intensity for pixel (x, y). The normalization with respect to intensity makes this descriptor independent of image brightness.
-
Histogram of oriented gradients (HoG) is a descriptor for gradient orientations weighted according to gradient magnitude [22, 23].
-
Local binary patterns (LBP) are texture descriptors that code the intensity differences between neighboring pixels by a histogram of binary patterns, which are generated by thresholding the relative intensity between all pixels and their neighboring pixels [24, 25]. LBP are among the most successful features in image analysis and often used in combination with HoG [19, 20, 22].
With these six descriptors, our overall number of features is \(6*32=192\). The eigenvalues of the Hessian matrix needed for the shape and curvature descriptors in Eqs. 1 and 2 were computed using a modification of the multiscale approach by Frangi et al. [26, 27]. We first smooth the lung region using a Gaussian filter G(x, s) at each pixel x and different scales s (\(s=2, 4, 6,\ldots , 20\)) and then compute the eigenvalues of the Hessian matrix on different scales, which captures the second-order characteristics.
To capture the visual features of drug resistance, we implement the following filter F that responds to spherical shapes, using the Hessian eigenvalues \(\lambda _1\) and \(\lambda _2\):
The larger the eigenvalues, the larger the filter response. We use the eigenvalues of the scale resulting in the largest response to compute the shape and curvature descriptors above [17].
We also use Pyramid Histogram of Oriented Gradients (PHoG), which is a popular region descriptor in many object recognition systems [28,29,30,31]. PHoG represents the region by its local shape and spatial layout of the shape. Spatial layout is preserved by tiling the image into small patches at multiple resolutions. Figure 2 illustrates three-level PHoG computations for a sample lung CXR image.
Each candidate region is divided into a finer spatial grid like a quad-tree. At the lowest level of the pyramid (\(L_{0}\)), a coarse histogram descriptor encodes the entire region, while finer-region grids are covered at higher-resolution pyramid levels. The dimension of the concatenated histogram is \(K\sum _{l=0}^{L}4^{l}\), where K is the number of bins and L is the number of pyramid levels. For our experiments, we computed a three-level spatial pyramid of HoG with eight bins leading to a feature vector of dimension 680.
Classification
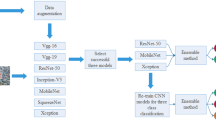
To discriminate between drug-resistant and drug-sensitive TB, we test different classifier architectures, which we list in the following.
Support vector machine We use a binary linear support vector machine (SVM), which classifies the computed feature vectors into one of the natural two classes, sensitive or resistant [32, 33]. The SVM computes the best separating hyperplane, which is the hyperplane with the largest distance to the nearest training data point of any class, between the feature vectors of both classes, as presented in a training set. The advantage of an SVM classifier compared to other recent classification methods, such as deep learning in particular, is that it can achieve a very good performance when trained on a small training set. It does not need as many training samples as required by deep learning for example. Mathematically, the majority of the feature vectors representing lungs with manifestations of drug resistance will be on the one side of the hyperplane, while feature vectors for lungs with drug-sensitive TB will be on the other side. Therefore, we are using the signed distance to the hyperplane as our confidence in a lung showing signs of drug resistance.
Artificial neural network (ANN) We used MATLAB standard pattern recognition neural network which is a two-layer feedforward network with a sigmoid transfer function in the hidden layer and a softmax transfer function in the output layer. The number of hidden neurons is comparable with the feature vector size.
Deep learning Deep learning has recently become a very popular classification scheme in medical applications and computer-aided diagnosis (CAD) in particular [34, 35]. It usually requires very large training sets but can often outperform traditional classification approaches [36]. It is an extension of traditional artificial neural networks in that networks typically have deeper structures with different types of network layers. We run deep learning experiments with both a pre-trained network and a customized network.
-
VGG-v16 For our pre-trained network, we use the VGG-v16 network architecture, which was introduced by Simonyan and Zisserman in 2014 for image classification [37]. It is characterized by its simplicity, using only 33 convolutional layers stacked on top of each other in increasing depth. Reducing volume size is handled by max pooling. Two fully connected layers, each with 4096 nodes, are then followed by a softmax classifier. The VGG-v16 has been pre-trained on more than a million images and has therefore learned rich feature representations for a wide range of images. We train this network and adapt it to our data, which is also called transfer learning.
-
CNN For our customized network, we follow a general network architecture for convolutional neural networks. Our network starts from a convolutional layer, which convolves the input feature maps with a number of convolutional kernels and yields a corresponding number of output feature maps. In order to perform a nonlinear transformation from the input to the output space, we adopt the rectified linear unit (ReLu) nonlinearity for each convolution [38]. Following each convolutional layer, a max-pooling layer is introduced to select feature subsets. The last convolutional feature map is connected to two fully connected layers with 512 and 2 hidden units, respectively. Between the two fully connected layers, we use a dropout layer with a dropout ratio of 0.4 to reduce overfitting (Fig. 3).
Results
In our first experiment, we test our classifiers on the 135 patients from Belarus, including 61 CXRs from patients with drug-sensitive TB and 74 CXRs from patients with MDR-TB and no follow-up CXRs.
Our customized CNN architecture for chest CXR classification. The numbers above the cuboid indicate the dimensions of the feature maps. The numbers below the green dotted lines represent the convolutional kernel size and the size of the max-pooling region. The output layer is a softmax layer that predicts the probability of drug sensitivity
In particular, we list the AUC for six different classifiers, namely the ANN with our shape and texture features, our customized CNN, SVM with shape and texture features, ANN with PHoG, SVM with PHoG, and a classifier based on a pre-trained VGG-v16 network (Table 7). The ANN with shape and texture features shows the best performance on Experiment 1, with an AUC of \(65\%\), whereas the other classifiers provide a much lower performance. The traditional ANN outperforms the customized CNN network, which we attribute to the small training set, which has been a known problem of large deep learning networks with many variables.
Table 8 shows the accuracy and \(F_\mathrm{measure}\) for the ANN classifier trained with shape and texture features based on fivefold cross-evaluation. The results for Experiment 1 are on the left-hand side of Table 8. For each fold, Table 8 reports the number of true positives (TP), false positives (FP), true negatives (TN), false negatives (FN), accuracy, and \(F_\mathrm{measure}\), where accuracy and \(F_\mathrm{measure}\) are computed as follows:
According to Table 8, we achieve an average accuracy of \(60\%\) and an average \(F_\mathrm{measure}\) of \(62\%\) for the ANN classifier, with shape and texture features, for Experiment 1.
The left-hand side of Fig. 4 shows our classification performance for the first experiment, measured as the area under the receiver operating characteristic curve (AUC) for the ANN classifier with shape and texture features. Due to the smaller training and test set size in Experiment 1, the ROC curves in Fig. 4a have a staircase shape and vary largely. For Experiment 1, Table 9 lists the results of the ANN classifier on shape and texture features, including AUC and accuracy (ACC), separated according to gender and age.
In a second experiment, we add the follow-up CXRs for all patients to the set, which increases the number of CXRs to 327, including 157 CXRs with drug-sensitive TB and 170 CXRs with drug-resistant TB (MDR). Table 2 lists the numbers of CXRs stratified according to age, gender, and resistance for Experiment 2. The right-hand side of Table 7 shows the AUC results of each of our classifiers for Experiment 2. Again, the ANN with shape and texture features performs the best, with an AUC of \(66\%\). This result differs only little from the performance in the first experiment, indicating that including follow-up CXRs does not add more information for discriminating between sensitive and MDR-TB.
On the right-hand side of Table 8, we list the accuracy and \(F_\mathrm{measure}\) for the ANN classifier trained with shape and texture features and fivefold cross-evaluation in Experiment 2. Similar to Table 7, the results are very close to the results observed for Experiment 1.
On the right-hand side of Fig. 4, we show the ROC curves for the ANN classifier for each fold in the second experiment. Compared to the curves on the left-hand side from Experiment 1, the variance is much lower due to the larger training set including follow-up CXRs.
Finally, Table 10 presents the AUC and accuracy for the ANN classifier trained with shape and texture features in Experiment 2, and stratified according to gender and age.
Conclusion
We investigate the possibility of using the conventional CXR to discriminate between drug-sensitive and drug-resistant forms of TB. For our experiments, we use different classifiers and features, including shape and texture features that have provided good results for computer-aided TB screening in CXRs, which assures us that the features we use can pick up TB-relevant textures and shapes in the lung field.
We perform two experiments: The first experiment includes only the initial CXR of each patient, whereas in the second experiment, we also include the follow-up CXRs for each patient. For both experiments, we train our classifiers and evaluated them by fivefold cross-evaluation. As features, we use our established set of texture and shape features and the PHoG descriptor. The best performance is achieved by a traditional neural network classifier (ANN) in combination with shape and texture features, which results in an AUC of \(65\%\) for the first experiment and \(66\%\) for the second experiment. We also experimented with two deep learning networks, a pre-trained VGG-v16 network and a customized convolutional neural network (CNN). Both networks do not perform better than our ANN. We attribute this to our relatively small training set size, which poses a problem for deep learning networks with many variables.
For both experiments, we stratified the data according to gender and age and present the corresponding AUC values and accuracies of our best performing ANN classifier.
Our approach relies solely on 2D CXR features and is in line with the few publications in the literature that can only report higher performance when including 3D information from CTs. In summary, our experiments provide evidence that automatic discrimination between drug-sensitive and drug-resistant TB can be possible in the conventional chest CXR. Generally speaking, automated screening for drug resistance in radiographs is still an open problem. Our results indicate that CXRs contain information about drug resistance. Describing the nature of this information will be the subject of future research. We can already say that discriminating between drug-resistant TB and drug-sensitive TB based on a CXR alone is difficult, and a much harder problem than detecting TB for which we obtain higher performance values. To obtain better results, it is therefore very promising to repeat this pilot study on larger training sets.
References
W.H.O. (2015) Global tuberculosis report (World Health Organization)
Barberis I, Bragazzi NL, Galluzzo L, Martini M (2017) The history of tuberculosis: from the first historical records to the isolation of koch’s bacillus. J Prev Med Hyg 58:E9
W.H.O.: Multidrug-resistant tuberculosis (MDR-TB) 2016 update (World Health Organization)
Chen RY, Dodd LE, Lee M, Paripati P, Hammoud DA, Mountz JM, Jeon D, Zia N, Zahiri H, Coleman MT, Carroll MW, Lee JD, Jeong YJ, Herscovitch P, Lahouar S, Tartakovsky M, Rosenthal A, Somaiyya S, Lee S, Goldfeder LC, Cai Y, Via LE, Park SK, Cho SN, Barry CE III (2014) PET/CT imaging correlates with treatment outcome in patients with multidrug-resistant tuberculosis. Sci Transl Med 6:265166
Yeom JA, Jeong YJ, Jeon D, Kim KI, Kim CW, Park HK, Kim YD (2009) Imaging findings of primary multidrug-resistant tuberculosis: a comparison with findings of drug-sensitive tuberculosis. J Comput Assist Tomogr 33:956–960
Cha J, Lee HY, Lee KS, Koh WJ, Kwon OJ, Yi CA, Kim TS, Chung MJ (2009) Radiological findings of extensively drug-resistant pulmonary tuberculosis in non-aids adults: comparisons with findings of multidrug-resistant and drug-sensitive tuberculosis. Korean J Radiol 10:207–216
Kim HC, Goo JM, Lee HJ, Park SH, Park CM, Kim TJ, Im JG (2004) Multidrug-resistant tuberculosis versus drug-sensitive tuberculosis in human immunodeficiency virus-negative patients: computed tomography features. J Comput Assist Tomogr 28:366–371
Chung MJ, Lee KS, Koh WJ, Kim TS, Kang EY, Kim SM, Kwon OJ, Kim S (2006) Drug-sensitive tuberculosis, multidrug-resistant tuberculosis, and non-tuberculous mycobacterial pulmonary disease in non-aids adults: comparisons of thin-section CT findings. Eur Radiol 16:1934–1941
Lee ES, Park CM, Goo JM, Yim JJ, Kim HR, Lee HJ, Lee IS, Im JG (2010) Computed tomography features of extensively drug-resistant pulmonary tuberculosis in non-HIV-infected patients. J Comput Assist Tomogr 34:559–563
Kovalev V, Liauchuk V, Safonau I, Astrauko A, Skrahina A, Tarasau A (2013) Is there any correlation between the drug resistance and structural features of radiological images of lung tuberculosis patients. Int J Comput Assist Radiol Surg 8:S18–S20
Kovalev V, Liauchuk V, Kalinouski A, Rosenthal A, Gabrielian A, Skrahina A, Astrauko A, Tarasau A (2015) Utilizing radiological images for predicting drug resistance of lung tuberculosis. In: Computer Assisted Radiology-27th International Congress and Exhibition (CARS-2015), vol 10, pp 129–130
Candemir S, Jaeger S, Palaniappan K, Musco JP, Singh RK, Xue Z, Karargyris A, Antani S, Thoma G, McDonald CJ (2014) Lung segmentation in chest radiographs using anatomical atlases with nonrigid registration. IEEE Trans Med Imaging 33:577–590
Ginneken B, Stegmann M, Loog M (2006) Segmentation of anatomical structures in chest radiographs using supervised methods: a comparative study on a public database. Med Image Anal 10:19–40
Liu C, Yuen J, Torralba A (2011) SIFT flow: Dense correspondence across different scenes and its applications. IEEE Trans Pattern Anal Mach Intell 33(5):978–994
Lowe DG (2004) Distinctive image features from scale-invariant keypoints. Int J Comput Vis 60:91–110
Shiraishi J, Katsuragawa S, Ikezoe J, Matsumoto T, Kobayashi T, Komatsu K, Matsui M, Fujita H, Kodera Y, Doi K (2000) Development of a digital image database for chest radiographs with and without a lung nodule: receiver operating characteristic analysis of radiologists detection of pulmonary nodules. Am J Roentgenol 174:71–74
Jaeger S, Karargyris A, Candemir S, Folio L, Siegelman J, Callaghan F, Xue Z, Palaniappan K, Singh RK, Antani S, Thoma G, Wang YX, Lu PX, McDonald CJ (2014) Automatic tuberculosis screening using chest radiographs. IEEE Trans Med Imaging 33:233–245
Jaeger S, Karargyris A, Antani S, Thoma G (2012) Detecting tuberculosis in radiographs using combined lung masks. In: International conference of IEEE engineering in medicine and biology society (EMBS), pp 4978–4981
Jaeger S, Casas-Delucchi C, Cardoso M, Palaniappan K (2010) Dual channel colocalization for cell cycle analysis using 3D confocal microscopy. In: International conference on pattern recognition, pp 2580–2583
Jaeger S, Casas-Delucchi C, Cardoso M, Palaniappan K (2010) Classification of cell cycle phases in 3D confocal microscopy using PCNA and chromocenter features. In: Indian conference on computer vision, graphics, and image processing, pp 412–418
Poostchi M, Bunyak F, Palaniappan K, Seetharaman G (2013) Feature selection for appearance-based vehicle tracking in geospatial video. In: Geospatial InfoFusion III, vol 8747. International Society for Optics and Photonics 87470G
Palaniappan K, Bunyak F, Kumar P, Ersoy I, Jaeger S, Ganguli K, Haridas A, Fraser J, Rao R, Seetharaman G (2010) Efficient feature extraction and likelihood fusion for vehicle tracking in low frame rate airborne video. In: International conference information fusion, pp 1–8
Dalal N, Triggs B (2005) Histograms of oriented gradients for human detection. In: International conference on computer vision pattern recognition, vol 1, pp 886–893
Ojala T, Pietikäinen M, Mäenpää T (2002) Multiresolution gray-scale and rotation invariant texture classification with local binary patterns. IEEE Trans Pattern Anal Mach Intell 24:971–987
Ojala T, Pietikäinen M, Harwood D (1996) A comparative study of texture measures with classification based on feature distributions. Pattern Recognit 29:51–59
Frangi A, Niessen W, Vincken K, Viergever M (1998) Multiscale vessel enhancement filtering. In: Medical image computing and computer-assisted intervention (MICCAI), pp 130–137
Bunyak F, Palaniappan K, Glinskii O, Glinskii V, Glinsky V, Huxley V (2008) Epifluorescence-based quantitative microvasculature remodeling using geodesic level-sets and shape-based evolution. In: International conference IEEE engineering in medicine and biology society (EMBS), pp 3134–3137
Bosch A, Zisserman A, Munoz X (2007) Representing shape with a spatial pyramid kernel. In: ACM international conference on Image and video retrieval, pp 401–408
Lazebnik S, Schmid C, Ponce J (2006) Beyond bags of features: spatial pyramid matching for recognizing natural scene categories. In: IEEE CVPR, vol 2, pp 2169–2178
Poostchi M, Palaniappan K, Seetharaman G (2017) Spatial pyramid context-aware moving vehicle detection and tracking in urban aerial imagery. In: 14th IEEE international conference on advanced video and signal based surveillance (AVSS). IEEE, pp 1–6
Chauhan A, Chauhan D, Rout C (2014) Role of Gist and PHOG features in computer-aided diagnosis of tuberculosis without segmentation. PLoS ONE 9:e112980
Vapnik V (2000) The nature of statistical learning theory. Springer, Berlin
Schölkopf B, Burges C, Smola A (1999) Advances in kernel methods: support vector learning. The MIT Press, Cambridge
Albarqouni S, Fotouhi J, Navab N (2017) X-ray in-depth decomposition: Revealing the latent structures. In: International conference on medical image computing and computer-assisted intervention. Springer, pp 444–452
Parisot S, Ktena SI, Ferrante E, Lee M, Moreno RG, Glocker B, Rueckert D (2017) Spectral graph convolutions for population-based disease prediction. In: International conference on medical image computing and computer-assisted intervention. Springer, pp 177–185
Wang X, Peng Y, Lu L, Lu Z, Bagheri M, Summers RM (2017) Chestx-ray8: hospital-scale chest x-ray database and benchmarks on weakly-supervised classification and localization of common thorax diseases. In: 2017 IEEE conference on computer vision and pattern recognition (CVPR). IEEE, pp 3462–3471
Simonyan K, Zisserman A (2014) Very deep convolutional networks for large-scale image recognition. CoRR arXiv:1409.1556
Krizhevsky A, Sutskever I, Hinton GE (2012) Imagenet classification with deep convolutional neural networks. In: Proceedings of the 25th International Conference on Neural Information Processing Systems, vol 1, pp 1097–1105
Acknowledgements
This research is supported by the Intramural Research Program of the National Institutes of Health (NIH), National Library of Medicine (NLM), and Lister Hill National Center for Biomedical Communications (LHNCBC).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Dr. Folio manages a research agreement with Carestream Health, unrelated to this project. The remaining authors declare that they have no conflict of interest.
Human and animal rights
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. The datasets were de-identified by the data providers and were exempted from IRB review at their institutions and by the NIH Office of Human Research Protections Programs (No. 5357). This article does not contain any studies with animals performed by any of the authors.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Jaeger, S., Juarez-Espinosa, O.H., Candemir, S. et al. Detecting drug-resistant tuberculosis in chest radiographs. Int J CARS 13, 1915–1925 (2018). https://doi.org/10.1007/s11548-018-1857-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-018-1857-9