Abstract
Purpose
For patients with myocardial infarction (MI), delayed enhancement (DE) cardiovascular magnetic resonance imaging (MRI) is a sensitive and well-validated technique for the detection and visualization of MI. The myocardium viability assessment with DE MRI is important in diagnosis and treatment management, where myocardium segmentation is a prerequisite. However, few academic works have focused on automated myocardium segmentation from DE images. In this study, we aim to develop an automatic myocardium segmentation algorithm that targets DE images.
Methods
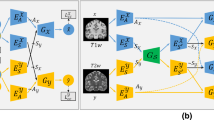
We propose a segmentation framework based on both prior shape knowledge and image intensity. Instead of the strong request of the pre-segmentation of cine MRI in the same session, we use the sparse representation method to model the myocardium shape. Data from the Cardiac MR Left Ventricle Segmentation Challenge (2009) are used to build the shape template repository. The method of guided random walks is used to integrate the shape model and intensity information. An iterative approach is used to gradually improve the results.
Results
The proposed method was tested on the DE MRI data from 30 MI patients. The proposed method achieved Dice similarity coefficients (DSC) of 74.60 ± 7.79% with 201 shape templates and 73.56 ± 6.32% with 56 shape templates, which were close to the inter-observer difference (73.94 ± 5.12%). To test the generalization of the proposed method to routine clinical images, the DE images of 10 successive new patients were collected, which were unseen during the method development and parameter tuning, and a DSC of 76.02 ± 7.43% was achieved.
Conclusion
The authors propose a novel approach for the segmentation of myocardium from DE MRI by using the sparse representation-based shape model and guided random walks. The sparse representation method effectively models the prior shape with a small number of shape templates, and the proposed method has the potential to achieve clinically relevant results.






Similar content being viewed by others
References
Kim HW, Farzaneh-Far A, Kim RJ (2009) Cardiovascular magnetic resonance in patients with myocardial infarction: current and emerging applications. J Am Coll Cardiol 55(1):1–16
Beek AM, van Rossum AC (2010) Cardiovascular magnetic resonance imaging in patients with acute myocardial infarction. Heart 96(3):237–243
Flett AS, Hasleton J, Cook C, Hausenloy D, Quarta G, Ariti C, Muthurangu V, Moon JC (2011) Evaluation of techniques for the quantification of myocardial scar of differing etiology using cardiac magnetic resonance. JACC Cardiovasc Imaging 4(2):150–156
Metwally MK, El-Gayar N, Osman NF (2010) Improved technique to detect the infarction in delayed enhancement image using k-mean method. In: Campilho A, Kamel M (eds) Image analysis and recognition. Springer, Berlin, pp 108–119. https://doi.org/10.1007/978-3-642-13775-4_12
Valindria VV, Angue M, Vignon N, Walker PM, Cochet A, Lalande A (2011) Automatic quantification of myocardial infarction from delayed enhancement MRI. In: 7th international conference on signal-image technology and internet-based systems (SITIS). IEEE, pp 277–283
Elagouni K, Ciofolo-Veit C, Mory B (2010) Automatic segmentation of pathological tissues in cardiac MRI. In: IEEE international symposium on biomedical imaging: from nano to macro (ISBI). IEEE, pp 472–475
Hennemuth A, Seeger A, Friman O, Miller S, Klumpp B, Oeltze S, Peitgen H-O (2008) A comprehensive approach to the analysis of contrast enhanced cardiac MR images. IEEE Trans Med Imaging 27(11):1592–1610
Hennemuth A, Friman O, Huellebrand M, Peitgen H-O (2012) Mixture-model-based segmentation of myocardial delayed enhancement MRI. In: Camara O, Mansi T, Pop M, Rhode K, Sermesant M, Young A (eds) Statistical atlases and computational models of the heart. Imaging and modelling challenges. Springer, Berlin, pp 87–96. https://doi.org/10.1007/978-3-642-36961-2_11
Tao Q, Milles J, Zeppenfeld K, Lamb HJ, Bax JJ, Reiber JH, van der Geest RJ (2010) Automated segmentation of myocardial scar in late enhancement MRI using combined intensity and spatial information. Magn Reson Med 64(2):586–594
Tao Q, Piers SRD, Lamb HJ, van der Geest RJ (2015) Automated left ventricle segmentation in late gadolinium-enhanced MRI for objective myocardial scar assessment. J Magn Reson Imaging 42(2):390–399. https://doi.org/10.1002/jmri.24804
Queirós S, Barbosa D, Heyde B, Morais P, Vilaça JL, Friboulet D, Bernard O, D’hooge J (2014) Fast automatic myocardial segmentation in 4D cine CMR datasets. Med Image Anal 18(7):1115–1131. https://doi.org/10.1016/j.media.2014.06.001
Liu Y, Captur G, Moon JC, Guo SX, Yang XP, Zhang SX, Li CM (2016) Distance regularized two level sets for segmentation of left and right ventricles from cine-MRI. Magn Reson Imaging 34(5):699–706. https://doi.org/10.1016/j.mri.2015.12.027
Engan K, Naranjo V, Eftesol T, Orn S, Woie L (2013) Automatic segmentation of the epicardium in late gadolinium enhanced cardiac MR images. Paper presented at the computing in cardiology conference
Wu KC, Zerhouni EA, Judd RM, Lugo-Olivieri CH, Barouch LA, Schulman SP, Blumenthal RS, Lima JAC (1998) Prognostic significance of microvascular obstruction by magnetic resonance imaging in patients with acute myocardial infarction. Circulation 97(8):765–772. https://doi.org/10.1161/01.cir.97.8.765
El-Berbari R, Kachenoura N, Frouin F, Herment A, Mousseaux E, Bloch I (2009) An automated quantification of the transmural myocardial infarct extent using cardiac DE-MR images. In: Conference proceedings of IEEE engineering in medicine and biology society, pp 4403–4406
Dikici E, O’Donnell T, Setser R, White RD (2004) Quantification of delayed enhancement MR images. In: Medical image computing and computer-assisted intervention (MICCAI). Springer, pp 250–257
Xu RS, Athavale P, Lu Y, Radau P, Wright GA (2013) Myocardial segmentation in late-enhancement MR images via registration and propagation of cine contours. In: IEEE 10th international symposium on biomedical imaging (ISBI). IEEE, pp 856–859
Ciofolo C, Fradkin M, Mory B, Hautvast G, Breeuwer M (2008) Automatic myocardium segmentation in late-enhancement MRI. In: 5th IEEE international symposium on biomedical imaging: from nano to macro (ISBI). IEEE, pp 225–228
Wei D, Sun Y, Ong S-H, Chai P, Teo LL, Low AF (2013) Three-dimensional segmentation of the left ventricle in late gadolinium enhanced MR images of chronic infarction combining long-and short-axis information. Med Image Anal 17(6):685–697
Kurzendorfer T, Brost A, Forman C, Maier A (2017) Automated left ventricle segmentation in 2-D LGE-MRI. In: IEEE 14th international symposium onbiomedical imaging (ISBI), pp 831–834
Liu J, Zhuang X, Wu L, An D, Xu J, Peters T, Gu L (2017) Myocardium segmentation from DE MRI using multi-component gaussian mixture model and coupled level set. IEEE Trans Biomed Eng 64(11):2650–2661. https://doi.org/10.1109/TBME.2017.2657656
Yushkevich PA, Piven J, Hazlett HC, Smith RG, Ho S, Gee JC, Gerig G (2006) User-guided 3D active contour segmentation of anatomical structures: significantly improved efficiency and reliability. Neuroimage 31(3):1116–1128. https://doi.org/10.1016/j.neuroimage.2006.01.015
Radau P, Lu Y, Connelly K, Paul G, Dick A, Wright G (2009) Evaluation framework for algorithms segmenting short axis cardiac MRI. MIDAS J 49(6)
Zhuang X, Rhode KS, Razavi RS, Hawkes DJ, Ourselin S (2010) A Registration-Based Propagation Framework for Automatic Whole Heart Segmentation of Cardiac MRI. IEEE Trans Med Imaging 29(9):1612–1625. https://doi.org/10.1109/TMI.2010.2047112
Zhuang XH, Arridge S, Hawkes DJ, Ourselin S (2011) A nonrigid registration framework using spatially encoded mutual information and free-form deformations. IEEE Trans Med Imaging 30(10):1819–1828. https://doi.org/10.1109/Tmi.2011.2150240
Cootes TF, Taylor CJ, Cooper DH, Graham J (1995) Active shape models-their training and application. Comput Vis Image Underst 61(1):38–59
Zhang S, Zhan Y, Dewan M, Huang J, Metaxas DN, Zhou XS (2012) Towards robust and effective shape modeling: sparse shape composition. Med Image Anal 16(1):265–277
Liu W, Ruan D Segmentation with a shape dictionary. In: IEEE 11th international symposium on biomedical imaging (ISBI), 2014. IEEE, pp 357–360
Efron B, Hastie T, Johnstone I, Tibshirani R (2004) Least angle regression. Ann Statist 32(2):407–499. https://doi.org/10.1214/009053604000000067
Grady L (2006) Random walks for image segmentation. IEEE Trans Pattern Anal Mach Intell 28(11):1768–1783
Eslami A, Karamalis A, Katouzian A, Navab N (2013) Segmentation by retrieval with guided random walks: application to left ventricle segmentation in MRI. Med Image Anal 17(2):236–253
Zhuang XH, Shen J (2016) Multi-scale patch and multi-modality atlases for whole heart segmentation of MRI. Med Image Anal 31:77–87. https://doi.org/10.1016/j.media.2016.02.006
Pop M, Sermesant M, Jodoin P-M, Lalande A, Zhang X, Yang G, Young A, Bernanrd O (eds) (2017) Statistical Atlases and computational models of the heart. ACDC and MMWHS challenges, vol 10663. Springer, Berlin. https://doi.org/10.1007/978-3-319-75541-0
Acknowledgements
This research is supported by the National Key Research and Development Program (2016YFC0106200), the 863 National Research Fund (2015AA043203), the Science and Technology Commission of Shanghai Municipality (17JC1401600) and the National Nature Science Foundation of China (61190120, 61190124, 61271318, 81301283 and 81511130090).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
For this type of study formal consent is not required. The testing data were collected at our institution with approval from the institutional review board.
Informed consent
This article does not contain any studies with human participants or animals performed by any of the authors.
Appendices
Appendix A: Some explanation about the derivation of solution equation
The energy function in Eq. (5) can be written as:
where \( \varvec{x} \) is the vector of the probability of all the voxels; \( \varvec{y}^{\text{shape}} \) is the prior shape for all the slices; \( \varvec{L} \) is the Laplacian matrix, as defined in Eqs. (6) and (7).
Since \( \varvec{L} \) is positive semi-definite and the value of parameter \( \gamma \) is positive, the matrix \( \left( {\varvec{L} + \frac{\gamma }{2}\varvec{I}} \right) \) is positive definite. So the only critical points of \( E\left( \varvec{x} \right) \) will be the minima. Differentiating \( E\left( \varvec{x} \right) \) with respect to \( \varvec{x} \), and the minimizer of \( E\left( \varvec{x} \right) \) is given by the linear equations in Eq. (8). By solving this system of linear equations, the probability map of myocardium can be obtained.
Appendix B: The effects of parameters and the recommended value ranges
There are totally five parameters in the proposed method, as summarized in Table 4. Among these parameters, the threshold \( T \), which is used to generate the binary segmentation from probability map, critically affects the results. We have recorded the DSC of myocardium with the threshold \( T \) increasing from 0.3 to 0.5, and the results are demonstrated in Fig. 7. The highest average DSC is achieved when the threshold is between 0.4 and 0.42, which contradicts to the convention of setting the threshold at 0.5 for probability binarization. This result is probably due to the elongated shape and relative small area of myocardium, as well as the relative low intensity contrast between myocardium and surrounding tissues. Since there is a neighborhood-related term in the energy function of random walks method, the probabilities of myocardium are easily affected by the pixels of background, including the blood pool encountered by the endocardium and the tissues around the epicardium. Therefore, a threshold below 0.5 is helpful to prevent the myocardium from being “swallowed” by the background. Evaluated with our testing data sets, when the threshold decreases from 0.4, the DSC decreases slowly because of the tendency to wrongly classify the surrounding pixels into myocardium. When the threshold increases to 0.48, in some data sets, the myocardium begins to be incorporated into the background, which results in a low average DSC and high DSC variance. When the method is applied for myocardium segmentation and the data resolution is similar to our data sets, this value does not need to be changed. When the segmentation target is of larger pixel number, such as in the case of data with higher resolution or target tissue of larger area, the value of threshold \( T \) will have less effect to the results.
The rest of four parameters do not have significant effect to the results in relative large value ranges. We have recorded the DSC of myocardium with weighting parameter \( \gamma \) doubling from 0.005 to 0.64, as illustrated in Fig. 8. The highest average DSC is achieved when \( \gamma \) is set at 0.01, but the paired t test shows that no significant difference (p < 0.05) exists between the \( \gamma \) value of 0.01 and the rest. This demonstrates that the change of parameter \( \gamma \) in a relatively large range (from 0.005 to 0.64) does not have a great effect on the final segmentation results. When the value of parameter \( \gamma \) is small, such as 0.005, insufficient shape information is imposed and the performance of the method becomes less stable, where the DSC standard deviation is larger. When parameter \( \gamma \) is set at a large value, such as 0.64, the imposed constraint may limit the flexibility of the algorithm, which results in a poorer fitting of the results to the image intensity.
The sparse representation-based model is able to select the proper shape templates from the dictionary to model the myocardium shape. However, as the size of the dictionary increase, the computation time will also increase. So we proposed to build the target-specific dictionary, where a threshold of DSC is used to remove some irrelevant shape templates and reduce the size of the dictionary. The shape repository used in this study is relative small, so we choose a low threshold of 30%. In this study, with the shape template repository built with 201 slices from the Challenge data set, a threshold below 50% does not have effect to the accuracy of results. And with a threshold of 60%, a DSC of 73.15 ± 8.50% is achieved. When the threshold is further increased, for some slices, no shape templates will be kept or the reserved number is too small to give enough flexibility modeling the actual myocardium shape. In the clinical practice, in order to reduce the computation time, the value can be set higher (such as 50–60%). Also, if the shape repository is large and has a good variety of shape characters, a higher value should be set.
The parameter λ in the sparse representation-based shape model controls the level of sparsity. When the parameter λ is larger, the nonzero elements in the vector \( \varvec{w} \) will be less. This means that less templates in \( D_{r} \) will be effective in representing the myocardium. In this study, the value of λ changing between 0.1–1 does not have significantly effect to the results.
Another free parameter is \( \beta \) in the Gaussian weighting function. When the value of \( \beta \) increases, the sensitivity of the random walks method to the intensity contrast increases. In our empirical observations, when the value of \( \beta \) is sufficiently large, changing \( \beta \) in a large range does not affect the results. In our experiment, the square gradients are normalized to the interval of [0, 1], and good results can be achieved when \( \beta > 100 \). In a relevant work [31], a careful study of the effect of \( \beta \) was undertaken, and a similar trend was found.
Rights and permissions
About this article
Cite this article
Liu, J., Zhuang, X., Xie, H. et al. Myocardium segmentation from DE MRI with guided random walks and sparse shape representation. Int J CARS 13, 1579–1590 (2018). https://doi.org/10.1007/s11548-018-1817-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-018-1817-4