Abstract
Objective
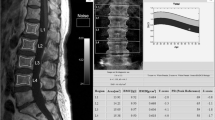
To develop a novel magnetic resonance imaging (MRI) phantom for producing F-score (for fat) and W-score (for water) and to evaluate the performance of these scores in assessing osteoporosis and related vertebral fractures.
Materials and methods
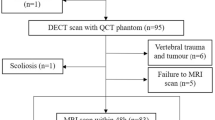
First, a real-time phantom consisting of oil and water tubes was manufactured. Then, 30 female volunteers (age: 62.3 ± 6.3 years) underwent lumbar spine examination with MRI (using a novel phantom) and dual-energy X-ray absorptiometry (DXA), following ethical approval. MRI phantom-based F-score and W-score were defined by normalizing the vertebral signal intensities (SIs) by the oil and water SIs of the phantom on T1- and T2-weighted images, respectively. The diagnostic performances of the new scores for assessing osteoporosis and vertebral fractures were examined using receiver operating characteristic analysis and compared with DXA-measured areal bone mineral density (DXA-aBMD).
Results
The F-score and W-score were greater in the osteoporotic patients (3.93 and 2.29) than the non-osteoporotic subjects (3.05 and 1.79) and achieved AUC values of 0.85 and 0.74 (p < 0.05), respectively, when detecting osteoporosis. Similarly, F-score and W-score had greater values for the fracture patients (3.94 and 2.53) than the non-fracture subjects (3.14 and 1.69) and produced better AUC values (0.90 for W-score and 0.79 for F-score) compared to DXA-aBMD (AUC: 0.27, p < 0.05). In addition, the F-score and W-score had a strong correlation (r = 0.77; p < 0.001).
Conclusion
A novel real-time lumber spine MRI phantom was developed, based upon which newly defined F-score and W-score were able to detect osteoporosis and demonstrated an improved ability over DXA-aBMD in differentiating patients with vertebral fractures.






Similar content being viewed by others
References
Compston JE, McClung MR, Leslie WD (2019) Osteoporosis. Lancet 393(10169):364–376
de Villiers TJ, Goldstein SR (2022) Bone health 2022: an update. Climacteric 25(1):1–3
Gao X et al (2023) Biomechanical MRI detects reduced bone strength in subjects with vertebral fractures. Bone 173:116810
Dong Y et al (2022) Global incidence, prevalence, and disability of vertebral fractures: a systematic analysis of the global burden of disease study 2019. Spine J 22(5):857–868
Ballane G et al (2017) Worldwide prevalence and incidence of osteoporotic vertebral fractures. Osteoporos Int 28(5):1531–1542
Wang L et al (2021) Prevalence of osteoporosis and fracture in China: the China osteoporosis prevalence study. JAMA Netw Open 4(8):e2121106–e2121106
Salari N et al (2021) Global prevalence of osteoporosis among the world older adults: a comprehensive systematic review and meta-analysis. J Orthop Surg Res 16(1):669
Jain RK, Vokes T (2017) Dual-energy X-ray Absorptiometry. J Clin Densitom 20(3):291–303
Sollmann N et al (2021) MRI-based quantitative osteoporosis imaging at the spine and femur. J Magn Reson Imaging 54(1):12–35
Kadri A et al (2022) Clinical risk factor status in patients with vertebral fracture but normal bone mineral density. Spine J 22(10):1634–1641
Messina C et al (2015) Prevalence and type of errors in dual-energy x-ray absorptiometry. Eur Radiol 25(5):1504–1511
Link TM, Kazakia G (2020) Update on imaging-based measurement of bone mineral density and quality. Curr Rheumatol Rep 22(5):13
Zou D et al (2019) The use of CT Hounsfield unit values to identify the undiagnosed spinal osteoporosis in patients with lumbar degenerative diseases. Eur Spine J 28(8):1758–1766
Din RU, Cheng X, Yang H (2021) diagnostic role of magnetic resonance imaging in low back pain caused by vertebral endplate degeneration. J Magn Resonance Imaging 55:755
Shraim BA et al (2021) The association between early MRI and length of disability in acute lower back pain: a systematic review and narrative synthesis. BMC Musculoskelet Disord 22(1):983
Liew I et al (2018) Requesting spinal MRIs effectively from primary care referrals. Eur Spine J 27(10):2436–2441
Bandirali M et al (2015) A new diagnostic score to detect osteoporosis in patients undergoing lumbar spine MRI. Eur Radiol 25(10):2951–2959
Shen W et al (2012) Relationship between MRI-measured bone marrow adipose tissue and hip and spine bone mineral density in African-American and Caucasian participants: the CARDIA study. J Clin Endocrinol Metab 97(4):1337–1346
Li R et al (2022) MRI-based vertebral bone quality score effectively reflects bone quality in patients with osteoporotic vertebral compressive fractures. Eur Spine J 31(5):1131–1137
Roch PJ et al (2023) Combination of vertebral bone quality scores from different magnetic resonance imaging sequences improves prognostic value for the estimation of osteoporosis. Spine J 23(2):305–311
Saad MM et al (2019) Role of lumbar spine signal intensity measurement by MRI in the diagnosis of osteoporosis in post-menopausal women. Egypt J Radiol Nuclear Med 50(1):1–7
Ehresman J et al. (2019) A novel MRI-based score assessing trabecular bone quality to predict vertebral compression fractures in patients with spinal metastasis. J Neurosurg Spine, 1–8.
Huang W et al (2023) Use of MRI-based vertebral bone quality score (VBQ) of S1 body in bone mineral density assessment for patients with lumbar degenerative diseases. Eur Spine J 32:1553
Hansen CB et al. (2019) Consideration of Cerebrospinal Fluid Intensity Variation in Diffusion Weighted MRI. Proc SPIE Int Soc Opt Eng, 10948.
Karampinos DC et al (2018) Quantitative MRI and spectroscopy of bone marrow. J Magn Reson Imaging 47(2):332–353
Takatsu Y et al (2013) Study of skin markers for magnetic resonance imaging examinations. Jpn J Radiol Technol 69(3):264–270
de Bazelaire CM et al (2004) MR imaging relaxation times of abdominal and pelvic tissues measured in vivo at 3.0 T: preliminary results. Radiology 230(3):652–9
Association NEM (2012) Determination of signal-to-noise ratio (SNR) in diagnostic magnetic resonance imaging. In: NEMA Standards Publication 2012, National Electrical Manufacturers Association: Virginia. pp 1–13
Shen Y et al (2022) The global burden of osteoporosis, low bone mass, and its related fracture in 204 countries and territories, 1990–2019. Front Endocrinol (Lausanne) 13:882241
Li X, Schwartz AV (2020) MRI assessment of bone marrow composition in osteoporosis. Curr Osteoporos Rep 18(1):57–66
Ali D et al (2022) The pathophysiology of osteoporosis in obesity and type 2 diabetes in aging women and men: the mechanisms and roles of increased bone marrow adiposity. Front Endocrinol (Lausanne) 13:981487
Beekman KM et al (2023) Osteoporosis and bone marrow adipose tissue. Curr Osteoporos Rep 21(1):45–55
Jara HJ (2013) Theory of quantitative magnetic resonance imaging. World Scientific Publishing Company, Singapore
Bani Hassan E et al (2019) Bone marrow adipose tissue quantification by imaging. Curr Osteoporos Rep 17(6):416–428
Atashi F, Modarressi A, Pepper MS (2015) The role of reactive oxygen species in mesenchymal stem cell adipogenic and osteogenic differentiation: a review. Stem Cells Dev 24(10):1150–1163
Liu X-G et al (2022) A superior articular process morphology of 5th lumbar vertebra prone to screws placement failure: an anatomical study of 299 patients. J Orthop Surg Res 17(1):505
Johnson M et al (2022) Actual applications of magnetic resonance imaging in dentomaxillofacial region. Oral Radiol 38(1):17–28
Yoshizawa E, Yamada A (2021) MRI-derived proton density fat fraction. J Med Ultrason 48(4):497–506
Mauch J et al (2018) Review of the imaging features of benign osteoporotic and malignant vertebral compression fractures. Am Soc Neuroradiology 39(9):1584–1592
Hammood SMA et al (2022) The role of Fast spin-echo T2-weighted and diffusion-weighted imaging for spine bone marrow changes evaluation in postmenopausal women with osteoporosis. Egypt J Radiol Nuclear Med 53(1):158
Funding
Funding from the National Natural Science Foundation of China (12272017) and Beijing Natural Science Foundation (L232058) is acknowledged.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors of this manuscript declare no relationships with any companies, whose products or services may be related to the subject matter of the article.
Ethical approval
This research involving human participants was conducted as per the Declaration of Helsinki, and informed consent was taken.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Din, R.U., Nishtar, T., Cheng, X. et al. Assessing osteoporosis in postmenopausal women: preliminary results using a novel lumbar spine phantom-based MRI scoring method. Radiol med (2024). https://doi.org/10.1007/s11547-024-01814-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11547-024-01814-x