Abstract
Purpose
To assess the role of contrast-enhanced mammography (CEM) in predicting the malignancy of breast calcifications.
Material and methods
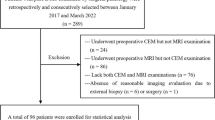
We retrospectively evaluated patients with suspicious calcifications (BIRADS 4) who underwent CEM and stereotactic vacuum-assisted biopsy (VAB) at our institution. We assessed the sensitivity (SE), specificity (SP), positive predictive value (PPV) and negative predictive value (NPV) of CEM in predicting malignancy of microcalcifications with a 95% confidence interval; we performed an overall analysis and a subgroup analysis stratified into group A-low risk (BIRADS 4a) and group B-medium/high risk (BIRADS 4b–4c). We then evaluated the correlation between enhancement and tumour proliferation index (Ki-67) for all malignant lesions.
Results
Data from 182 patients with 184 lesions were collected. Overall the SE of CEM in predicting the malignancy of microcalcifications was 0.70, SP was 0.85, the PPV was 0.82, the NPV was 0.76 and AUC was 0.78. SE in group A was 0.89, SP was 0.89, PPV was 0.57, NPV was 0.98 and AUC was 0.75. SE in group B was 0.68, SP was 0.80, PPV was 0.87, NPV was 0.57 and AUC was 0.75. Among malignant microcalcifications that showed enhancement (N = 52), 61.5% had Ki-67 ≥ 20% and 38.5% had low Ki-67 values. Among the lesions that did not show enhancement (N = 22), 90.9% had Ki-67 < 20% and 9.1% showed high Ki-67 values 20%.
Conclusions
The absence of enhancement can be used as an indicative parameter for the absence of disease in cases of low-suspicious microcalcifications, but not in intermediate-high suspicious ones for which biopsy remains mandatory and can be used to distinguish indolent lesions from more aggressive neoplasms, with consequent reduction of overdiagnosis and overtreatment.


Similar content being viewed by others
References
Grimm LJ, Destounis SV, Rahbar H, Soo MS, Poplack SP (2020) Ductal carcinoma in situ biology, language, and active surveillance: a survey of breast radiologists’ knowledge and opinions. J Am Coll Radiol 17(10):1252–1258. https://doi.org/10.1016/j.jacr.2020.03.004
Sickles EA, D’Orsi CJ, Bassett LW, Appleton CM, Berg WA, Burnside ES. ACR BI-RADS Atlas, Breast imaging reporting and data system. 5th ed. Reston, Virginia: American College of Radiology; 2013.
Bennani-Baiti B, Baltzer PA (2017) MR imaging for diagnosis of malignancy in mammographic microcalcifications: a systematic review and meta-analysis. Radiology 283(3):692–701. https://doi.org/10.1148/radiol.2016161106
Salvatorelli L, Puzzo L, Vecchio GM, Caltabiano R, Virzì V, Magro G (2020) Ductal carcinoma in situ of the breast: an update with emphasis on radiological and morphological features as predictive prognostic factors. Cancers (Basel) 12(3):609. https://doi.org/10.3390/cancers12030609
Grimm LJ, Rahbar H, Abdelmalak M, Hall AH, Ryser MD (2022) Ductal carcinoma in situ: state-of-the-art review. Radiology 302(2):246–255. https://doi.org/10.1148/radiol.211839
Rominger M, Wisgickl C, Timmesfeld N (2012) Breast microcalcifications as type descriptors to stratify risk of malignancy: a systematic review and meta-analysis of 10665 cases with special focus on round/punctate microcalcifications. Rofo 184(12):1144–1152. https://doi.org/10.1055/s-0032-1313102
D’Orsi CJ (2010) Imaging for the diagnosis and management of ductal carcinoma in situ. J Natl Cancer Inst Monogr 2010(41):214–217. https://doi.org/10.1093/jncimonographs/lgq037
Azam S, Eriksson M, Sjölander A, Gabrielson M, Hellgren R, Czene K, Hall P (2021) Mammographic microcalcifications and risk of breast cancer. Br J Cancer 125(5):759–765. https://doi.org/10.1038/s41416-021-01459-x
van Leeuwen MM, Doyle S, van den Belt-Dusebout AW et al (2023) Clinicopathological and prognostic value of calcification morphology descriptors in ductal carcinoma in situ of the breast: a systematic review and meta-analysis. Insights Imaging 14:213. https://doi.org/10.1186/s13244-023-01529-z
Baltzer PAT, Bennani-Baiti B, Stöttinger A, Bumberger A, Kapetas P, Clauser P (2018) Is breast MRI a helpful additional diagnostic test in suspicious mammographic microcalcifications? Magn Reson Imaging 46:70–74. https://doi.org/10.1016/j.mri.2017.10.012
Bennani-Baiti B, Dietzel M, Baltzer PA (2017) MRI for the assessment of malignancy in BI-RADS 4 mammographic microcalcifications. PLoS ONE 12(11):e0188679. https://doi.org/10.1371/journal.pone.0188679
Fueger BJ, Clauser P, Kapetas P, Pötsch N, Helbich TH, Baltzer PAT (2021) Can supplementary contrast-enhanced MRI of the breast avoid needle biopsies in suspicious microcalcifications seen on mammography? System Rev Meta-Anal Breast 56:53–60. https://doi.org/10.1016/j.breast.2021.02.002
Bhimani C, Matta D, Roth RG, Liao L, Tinney E, Brill K, Germaine P (2017) Contrast-enhanced spectral mammography: technique, indications, and clinical applications. Acad Radiol 24(1):84–88. https://doi.org/10.1016/j.acra.2016.08.019
Jochelson MS, Lobbes MBI (2021) Contrast-enhanced mammography: state of the art. Radiology 299(1):36–48. https://doi.org/10.1148/radiol.2021201948
Lobbes MB, Lalji U, Houwers J, Nijssen EC, Nelemans PJ, van Roozendaal L, Smidt ML, Heuts E, Wildberger JE (2014) Contrast-enhanced spectral mammography in patients referred from the breast cancer screening programme. Eur Radiol 24(7):1668–1676. https://doi.org/10.1007/s00330-014-3154-5
Cheung YC, Lin YC, Wan YL, Yeow KM, Huang PC, Lo YF, Tsai HP, Ueng SH, Chang CJ (2014) Diagnostic performance of dual-energy contrast-enhanced subtracted mammography in dense breasts compared to mammography alone: interobserver blind-reading analysis. Eur Radiol 24(10):2394–2403. https://doi.org/10.1007/s00330-014-3271-1
Cheung YC, Juan YH, Lin YC, Lo YF, Tsai HP, Ueng SH, Chen SC (2016) Dual-energy contrast-enhanced spectral mammography: enhancement analysis on BI-RADS 4 non-mass microcalcifications in screened women. PLoS ONE 11(9):e0162740. https://doi.org/10.1371/journal.pone.0162740
Covington MF, Pizzitola VJ, Lorans R, Pockaj BA, Northfelt DW, Appleton CM, Patel BK (2018) The future of contrast-enhanced mammography. AJR Am J Roentgenol 210(2):292–300. https://doi.org/10.2214/AJR.17.18749
Depretto C, Borelli A, Liguori A, Presti G, Vingiani A, Cartia F, Ferranti C, Scaperrotta GP (2020) Contrast-enhanced mammography in the evaluation of breast calcifications: preliminary experience. Tumori 106(6):491–496. https://doi.org/10.1177/0300891620919170
Goldhirsch A, Winer EP, Coates AS, Gelber RD, Piccart-Gebhart M, Thürlimann B, Wood WC (2013) Personalizing the treatment of women with early breast cancer: highlights of the St Gallen international expert consensus on the primary therapy of early breast cancer 2013. Annals Oncol 24(9):2206–2223. https://doi.org/10.1093/annonc/mdt303
Mordang JJ, Gubern-Mérida A, Bria A, Tortorella F, Mann RM, Broeders MJM, den Heeten GJ, Karssemeijer N (2018) The importance of early detection of calcifications associated with breast cancer in screening. Breast Cancer Res Treat 167(2):451–458. https://doi.org/10.1007/s10549-017-4527-7
Gosling SB, Arnold EL, Davies SK et al (2023) Microcalcification crystallography as a potential marker of DCIS recurrence. Sci Rep 13:9331. https://doi.org/10.1038/s41598-023-33547-8
Fauveau LR, Dao TN, Wallace LB et al (2023) Positive surgical margins after breast-conserving surgery for ductal carcinoma in-situ: does histologic grade or estrogen receptor status matter? Breast Cancer Res Treat 199:215–220. https://doi.org/10.1007/s10549-023-06905-3
Cheung YC, Tsai HP, Lo YF, Ueng SH, Huang PC, Chen SC (2016) Clinical utility of dual-energy contrast-enhanced spectral mammography for breast microcalcifications without associated mass: a preliminary analysis. Eur Radiol 26(4):1082–1089. https://doi.org/10.1007/s00330-015-3904-z
Long R, Cao K, Cao M, Li XT, Gao F, Zhang FD, Yu YZ, Sun YS (2021) Improving the diagnostic accuracy of breast BI-RADS 4 microcalcification-only lesions using contrast-enhanced mammography. Clin Breast Cancer 21(3):256-262.e2. https://doi.org/10.1016/j.clbc.2020.10.011
Houben IP, Vanwetswinkel S, Kalia V, Thywissen T, Nelemans PJ, Heuts EM, Smidt ML, Meyer-Baese A, Wildberger JE, Lobbes M (2019) Contrast-enhanced spectral mammography in the evaluation of breast suspicious calcifications: diagnostic accuracy and impact on surgical management. Acta Radiol 60(9):1110–1117. https://doi.org/10.1177/0284185118822639
Ma T, Semsarian CR, Barratt A, Parker L, Pathmanathan N, Nickel B, Bell KJL (2023) Should low-risk DCIS lose the cancer label? An evidence review. Breast Cancer Res Treat 199(3):415–433. https://doi.org/10.1007/s10549-023-06934-y
Elshof LE, Tryfonidis K, Slaets L, van Leeuwen-Stok AE, Skinner VP, Dif N, Pijnappel RM, Bijker N, Rutgers EJ, Wesseling J (2015) Feasibility of a prospective, randomised, open-label, international multicentre, phase III, non-inferiority trial to assess the safety of active surveillance for low risk ductal carcinoma in situ–The LORD study. Eur J Cancer 51(12):1497–1510. https://doi.org/10.1016/j.ejca.2015.05.008
Francis A, Thomas J, Fallowfield L, Wallis M, Bartlett JM, Brookes C, Roberts T, Pirrie S, Gaunt C, Young J, Billingham L, Dodwell D, Hanby A, Pinder SE, Evans A, Reed M, Jenkins V, Matthews L, Wilcox M, Fairbrother P, Bowden S, Rea D (2015) Addressing overtreatment of screen detected DCIS; the LORIS trial. Eur J Cancer 51(16):2296–2303. https://doi.org/10.1016/j.ejca.2015.07.017
Hwang ES, Hyslop T, Lynch T, Frank E, Pinto D, Basila D, Collyar D, Bennett A, Kaplan C, Rosenberg S, Thompson A, Weiss A, Partridge A (2019) The COMET (Comparison of operative versus monitoring and endocrine therapy) trial: a phase III randomised controlled clinical trial for low-risk ductal carcinoma in situ (DCIS). BMJ Open 9(3):e026797. https://doi.org/10.1136/bmjopen-2018-026797
Hiroji I (2021) Single-arm confirmatory trial of endocrine therapy alone for estrogen receptor-positive, low-risk ductal carcinoma in situ of the breast (JCOG1505, LORETTA trial). https://upload.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno = R000032260. Accessed July 14
Kraby MR, Krüger K, Opdahl S, Vatten LJ, Akslen LA, Bofin AM (2015) Microvascular proliferation in luminal A and basal-like breast cancer subtypes. J Clin Pathol 68(11):891–897. https://doi.org/10.1136/jclinpath-2015-203037
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Author information
Authors and Affiliations
Contributions
CD was responsible for the conception of the study. E. D’Ascoli evaluated the literature, collected data and wrote the first draft of the manuscript. GDP performed analysis and interpretation of results. DB, AB and EA collected data. CDB and GI evaluated the literature and contributed to the finalisation of the manuscript. CF and GPS provided expertise, mentorship and final revision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
This study was approved by the institutional review board. All procedures performed in the studies involving human participants were in accordance with the ethical standards of the Institution “Fondazione IRCCS Istituto Nazionale dei Tumori” of Milan and with the 1964 Helsinki Declaration and its later amendments.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Consent to publish
Participants provided informed consent for publication of the images in Fig. 1 and 2.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Depretto, C., D’Ascoli, E., Della Pepa, G. et al. Assessing the malignancy of suspicious breast microcalcifications: the role of contrast enhanced mammography. Radiol med (2024). https://doi.org/10.1007/s11547-024-01813-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11547-024-01813-y