Abstract
Introduction
Whole body magnetic resonance imaging (WB-MRI) is a promising emerging imaging technology for detecting bone and soft tissue pathology, especially in the onco-hematological field. This study aims to evaluate cancer patients' experience of WB-MRI performed on a 3T scanner compared to other diagnostic total body examinations.
Material and method
In this prospective committee-approved study, patients completed a questionnaire in person (n = 134) after undergoing a WB-MRI scan to collect data on their physical and psychological reactions during the scan, the global satisfaction level, and preference for other types of MRI or computed tomography (CT), or positron emission tomography (PET/CT). Of all patients who had performed a CT or PET/CT the previous year, 61.9% had already undergone an MRI. The most common symptoms reported were: 38.1% perceived a localized increase in temperature and 34.4% numbness and tingling of the limbs. The scan time averaged 45 min and was well tolerated by most patients (112, 85.5%). Overall, WB-MRI was appreciated by the majority (121/134—90.3%) of patients who said they would probably undergo the procedure again. Patients preferred the WB-MRI in 68.7% of cases (92/134), followed by CT in 15.7% of cases (21/134) and by PET/CT in 7.4% (10/134), with 8.4% (11/134) of patients without any preference. The preference for imaging modalities was age-dependent (p = 0.011), while (p > 0.05) was independent of sex and a primary cancer site.
Conclusion
These results demonstrate a high degree of WB-MRI acceptance from a patient's point of view.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Whole body magnetic resonance imaging (WB-MRI) is a radiation-free imaging method, generally without contrast media administration, that detects and evaluates soft tissue and bone marrow pathology in different types of cancer. WB-MRI combines high-quality morphological sequences with “functional” images based on diffusion-weighted imaging (DWI), acquired at least from skull base to mid-thigh, following the well-established practices for whole body computed tomography (CT) and positron emission tomography/computed tomography (PET/CT). Other segments can be added to the basic protocol based on clinical need.
The core sequence of WB-MRI is DWI, which provides quantitative information on the diffusivity of water molecules by calculating the Apparent Diffusion Coefficient (ADC) [1, 2]. Numerous studies have demonstrated the capabilities of MRI for monitoring the response of bone metastases to treatment and the added value of WB-MRI sequences to overcome some of the limitations of standard imaging methods like CT, Bone Scintigraphy (BS), and 18F-Fluorodeoxyglucose (FDG) PET/CT in disease assessment and evaluation response to anticancer therapy [1,2,3]
Standard imaging methods have shown substantial limitations in the detection and assessment of bone disease, even though bone metastases from prostate and breast cancer are very common. [4, 5]. In response evaluation criteria in solid tumors (RECIST) version 1.1, bone metastases are considered non-measurable lesions [6]. Increased sclerosis and the sclerotic response of bone metastases can be difficult to distinguish with CT [5]. Bone Scintigraphy with technetium 99 m (99mTc)–methylene diphosphonate often results in underestimation of the disease extent, and difficulties in interpretation of serial bone scans are well described as “healing or flare response” of the bone [7].
High-quality morphological sequences are also useful in the detection, characterization, and response assessment of bone marrow. In this setting, T1-weighted images obtained with gradient-echo (GRE) Dixon acquisitions are usually performed to generate in- and opposed-phase images, permitting the calculation of fat-only and water-only images as well as the relative Fat Fraction map (rFF%) [8].
Some parameters of WB-MRI, in particular values from the Apparent Diffusion Coefficient (ADC) map and the relative Fat Fraction (rFF%) map, are emerging as possible MR imaging biomarkers at diagnosis and during therapy response [9, 10].
The development of WB-MRI has led to a new dimension for evaluating bone marrow involvement in patients affected by immune plasma cell disorders. For the assessment of bone disease, the International Myeloma Working Group (IMWG) suggests a variety of imaging assessments, including low-dose CT, (FDG)PET/CT, and MRI. Given WB-MRI's high sensitivity, it has been recommended for patients affected by bone solitary plasmocitoma and for patients suspected of having non-IgM monoclonal gammopathy of undetermined significance (MGUS), smouldering multiple myeloma or multiple myeloma and who underwent low-dose WB-CT or (FDG)PET/CT with negative or inconclusive findings [11, 12].
Moreover, according to the European Union directive 2013/59/Euratom, concerns have arisen over radiation exposure from imaging examinations, which has led to the E.U. expressing interest in WB-MRI as an alternative to standard imaging procedures, especially in young cancer patients with a long-life expectancy.
As a result, WB-MRI is currently implemented in several professional society guidelines, including advanced prostate cancer [13, 14], multiple myeloma [11], and cancer screening in a high-risk population for genetic predisposition [15]. A recent expert review panel [16] found a consensus supporting WB-MRI as a first-line imaging approach in patients with multiple myeloma and pregnancy, as well as a well-established screening tool in patients with cancer risk factors (strong evidence for the Li-Fraumeni syndrome) [17], and also useful in assessing patients with known bone and visceral metastases [16]. Moreover, WB-MRI has a key role in patients affected by known metastatic disease, non-avid FDG lymphomas, or bone neoplasm. Finally, there is an increasing number of studies that report its use for cancer screening in the general population [18]
However, MRI is generally considered more stressful than other imaging modalities [19, 20], such as CT and PET/CT; due to its longer acquisition times, WB-MRI could be even more stressful, thus jeopardizing the image quality and discouraging the adoption in clinical routine. In particular, compared to the other whole body imaging modalities, acquisition times of WB-MRI are longer: a complete WB-MRI takes around 35–50 min, in which the patient should lie still, tightly wrapped in the body coils, inside a narrow tube with a loud background noise.
In general, there is no evidence of negative effects associated with performing MRI on 1.5T or 3T scanners, but magnetic field strength was found to be statistically associated with new-onset dizziness; Weintraub et al. found that most patients of subjects (86%) did not notice a difference between 1.5T and 3T scan but a 14% of subjects experienced sensory stimulation (new or altered symptoms) in both 3T and 1.5T units, predominantly in women, indicating the existence of a threshold of magnetic susceptibility and sexual vulnerability [21].
WB-MRI is usually used on cancer patients, who are often older than the general population, have age-related disabilities, are more likely to develop painful bone metastases, and are subjected to higher physiological pressures. All of these factors can affect a patient's ability to perform a WB-MRI scan.
The effects of the interaction between patients and imaging are often overlooked in favor of evaluating diagnostic efficacy, and, despite the improvements, there is the possibility that imaging creates a major psychological and physical burden especially on cancer patients. As various whole body imaging modalities can be used for diagnosis and follow-up in different settings, understanding the patient experience may be beneficial in particular in modern healthcare where it is crucial to recognize and meet patients' needs and preferences [22]. To guarantee patient-centered care and good-quality scans, acceptance of WB-MRI is a pivotal topic and the studies available yielded somewhat divergent findings but none of them was performed exclusively on 3T MRI scanners.
Our study aimed to evaluate the patient experience and acceptability of a 3T WB-MRI in an oncological setting also with a comparison with PET/TC or Contrast Enhancement CT (CE-CT).
Materials and methods
This prospective study was approved by the Ethical Committee (IRST100.15), and all participants signed an informed consent to be enrolled in the study, in addition to the standard consent required by law for MRI scans.
From October 2020 to March 2022, all the patients who underwent a first-in-life WB-MRI at our institution for clinical reasons (cancer staging or follow-up) were asked to participate in this study for their feedback on the procedure, even if they did not complete the scan.
The patients completed the questionnaire under the Radiologist’s supervision after the WB-MRI before leaving the MRI site. The questionnaire was divided into several parts: the first included demographic information and the examination date.
The second part concerned the patient’s experience: the physical and psychological reactions during the scan, such as dizziness, involuntary muscle contraction, tingling, tickles, increased temperature, sweating, fatigue, fear, headache, nausea, and tachycardia. All the data were evaluated using a four-point scale (0 not present; 1 present; 2 unpleasant, but tolerable; 3 intolerable).
The third part evaluated the global level of satisfaction of WB-MRI considering exam duration, noise, the narrowness of the tube, and comfort of positioning (1 at ease; 2 low uneasiness; 3 moderate uneasiness; 4 strong uneasiness). Finally, in patients who had already performed other total body examinations, preference between WB-MRI and other diagnostic modalities was investigated.
WB-MRI protocol at our institution
Patient candidates for WB-MRI are carefully evaluated and selected by the prescribing physician. He gives potential candidates an in-depth explanation of the technique and possible benefits on patient management deriving from the diagnostic result of this method; informed consent is acquired. Moreover, patient characteristics may influence the exam modality. For example, patients with claustrophobia or MRI-unsafe devices must undergo a CT or PET/CT and are excluded. In case of pain or anxiety, appropriate therapy is given. Immediately before the exam, the radiologist explains the exam procedure to the patients again and administers additional medication if needed to alleviate pain and anxiety.
All the WB-MRI were performed on a 3T MRI scanner (Ingenia Philips, Eindhoven, Netherlands).
A head/neck helmet-like coil and a flexible surface body coil are applied to patients for WB-MRI scans.
Both earplugs and earmuffs are put on patients, and the patient's favorite music is played.
Fasting is not required for WB-MRI without intravenous contrast media, but patients are advised to have only a light meal before the exam.
The WB-MRI basic protocols at our institution are based on MET-RADS [23] and MY-RADS [24] and consist of sagittal T1-weighted and sagittal STIR T2-weighted sequences of the entire spine, axial diffusion-weighted whole body imaging with background body signal suppression (DWIBS) technique at two b-Value (b50 e b800), axial GRE T2 and axial T1 Gradient Echo (GRE) mDixon sequences from vertex to mid-thighs (from vertex to knees for multiple myeloma). From the DWI and the Dixon-type images, the Apparent Diffusion Coefficient (ADC) map and the relative Fat Fraction (rFF%) maps are, respectively, reconstructed,
Usually, patients are prepared for the intravenous contrast medium only in case of known or suspected brain metastasis, according to clinical needs, particularly in patients with melanoma [25]. Dedicated brain assessment is performed with axial FLAIR, pre- and post-contrast 3D T1W GRE.
At the time of writing, the ONCO-RADS [26] acquisition protocol was used only for some very young patients affected by metastatic paraganglioma/pheochromocytoma in follow-up after therapy due to radiation protection. Detailed parameters of the most common protocols used at our institution are described in Table 1 whereas the sequence parameters are described in Table 2. An example of images acquired is shown in Fig. 1.
The imaging protocol can also be “tailored” depending on clinical needs, adding other specific imaging targets.
Statistical analysis
Statistical analyses were performed using the statistical and data management package MedCalc for Windows (Version 5.0.1.0 Ostend, Belgium). ANOVA or Pearson's Chi-squared test was performed to investigate the influence of age (ANOVA), sex (Chi-squared), and primary cancer (Chi-squared) on the acceptance of WB-MRI compared to other total body imaging modalities (CT or PET). Statistical significance was set at P < 0.05 for all tests. Descriptive data are reported as frequencies or mean and standard deviation (± s.d.).
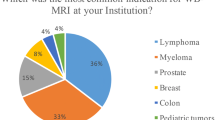
A total of 134 patients (73 males, 61 females) with a mean age of 61.3 ± 13.8 years were enrolled in this study (Fig. 2).
Multiple myeloma (56/134—41.8%) and prostate cancer (20/134—14.9%) were the most common cancer types among patients, followed by melanoma (16/134—11.9%) and breast cancer (14/134—10.4%); all the other patients included in the study are shown in Table 3.
All patients had already performed other total body imaging techniques the previous year (CT and PET/CT); 83 patients (61.9%) had already performed MRI in different body districts with a similar scanner 1.5T or 3T, and only one patient had already undergone WB-MRI in another hospital on 1.5T scanner.
In response to an open-ended question, none of these patients reported differences in symptoms or approval compared to previous MRIs.
The most frequent symptom reported by the patients was a localized increase in temperature (51/134—38.1%), which was deemed tolerable in all cases, whereas sweating was reported in only nine cases (9/134—6.7%) and always tolerable (Fig. 3). Numbness and tingling of the limbs were both reported in 46 (46/134—34.4%) cases and were deemed unpleasant or intolerable in 9 (9/46—19.6%) and 3 (3/46—6.5%) cases, respectively.
Patients reported involuntary muscle movements and dizziness in 7/134 (5.2%) and 4/134 (3%) cases. Eight patients experienced fear (8/134—6.0%) at the beginning of the procedure but disappeared throughout the examination. Moreover, two patients (2/134—1.5%) described palpitations.
There were no reports of any additional symptoms, including nausea, metallic taste, headaches, tickles, scotomas, or muscle stimulation.
Most patients were able to tolerate the length of the WB-MRI as well as the noise and positioning. Only a few patients found the length of the examination, confined space, and positioning to be uncomfortable. In particular, 113 patients (113/134 84.3%) perceived the WB-MRI duration as tolerable, 21 patients (21/134—15.7%) as unpleasant, and three patients considered it intolerable. Additionally, 26 patients (26/134—19.4%) considered the examination tiring and 15 out of 26 said it was very exhausting (Fig. 4). Bore narrowness, noise, and positioning were considered unpleasant, respectively, by 9/134 (6.7%), 11/134 (8.2%), and 11/134 (8.2%) of patients, but never intolerable.
Figure shows the detection features of the Whole Body exam based on the level perceived by the patient. The six graphs show the percentage of patients divided according to the level of exam characteristics recorded. The Whole-Body exam features studied were: exam duration graph (A), room temperature for graph (B), narrow hole space graph (C), noise graph (D), placement graph (E), and healthcare professional interaction in graph (F)
Overall, WB-MRI was appreciated by the vast majority of patients (121/134—90.3%) who said they would probably undergo the procedure again, whereas 13/134 (9.7%) said they would not repeat the examination in the future due to the narrowness of tube (3/13), lengthy examination time (8/13), and uncomfortable positioning (2/13). When asked to express a preference between the whole body imaging modalities, patients preferred the WB-MRI in 68.7% of cases (92/134), followed by Computed Tomography in 15.7% of cases (21/134) and Positron Emission Tomography in 7.4% (10/134), with a 8.2% (11/134) of patients who said they did not have any preference.
The preference for imaging modalities was influenced by age (p = 0.011) with younger patients preferring WB-MRI, independently of sex and primary cancer (p > 0.05).
Discussion
Patient acceptability of new technologies is crucial for developing and implementing imaging methods and obtaining successful diagnostic examinations.
Low patient acceptability may lead to a lack of compliance during image acquisition, which can negatively affect the image quality [27] due to motion artifacts, especially if the examination requires a long acquisition time. Our study showed that most cancer patients of all types accept and highly appreciate WB-MRI compared to the other total body imaging modalities.
The most common symptom reported by patients in our study was a localized increase in temperature, most likely due to the high overall Specific Energy Dose (SED) of WB-MRI, which implies an increase in body temperature, sometimes associated with sweating. Thus, maintaining a medium–high ventilation level inside the bore, allowing optimal heat dissipation, is crucial.
Numbness and tingling are two more common symptoms reported by patients, which may be connected to the patient's positioning and the requirement to keep motionless. The proper acquisition of MRI images is heavily reliant on the patient's cooperation, which is more evident in WB-MRI, given the lengthy examination time, and the concatenation of sequences, which are very sensitive to voluntary and involuntary movements: It is thus critical to position the patient appropriately and comfortably, for example, with a knee cushion and armrest if available, to prevent patient movement.
The length of the examination and the need to concentrate to keep motionless following the operator's orders contribute to making the examination tiring, which is another frequent complaint made by patients; however, in our study, most of the patients that considered tiring (16/26—61.5%) or lengthy (13/21—61,9%) the examination will undergo again to WB-MRI, and some of them (9/26 and 5/21) prefer the WB-MRI to the other whole body imaging modalities, mostly due to the absence of ionizing radiations.
The examination's noise level was another issue raised frequently by patients. The loudness of several sequences—most notably DWI and T1W GRE mDixon—is quite high, and wearing both earplugs and earmuffs improve patient acceptability of the examination by reducing the perceived acoustic noise and enabling operator-patient communication, such as during breath-hold commands. Additionally, several patients suggested that listening to music could help reduce the discomfort induced by the loudness of the scan.
MRI scanners are notoriously small, and the mere thought of facing an MRI can generate anxiety in some patients. Consequently, identifying patients with claustrophobia and speaking to them beforehand are fundamental. To alleviate MRI-related anxiety, the patient is asked to keep their eyes closed for the duration of the procedure; in mildly claustrophobic individuals, a dark blindfold can be helpful.
The patients' comments highlight the importance of the staff's involvement in explaining the procedure by assisting the patient in coping with intrinsic problems of WB-MRI to complete the examination and obtain reliable images. Furthermore, careful patient selection based on clinical circumstances is essential, making collaboration with oncologists even more critical.
This study also found that many patients prefer WB-MRI over other whole body imaging modalities, such as PET/CT and CT, since it is contrast-free and ionizing radiation-free, despite lasting longer, loudness, complete body and head immersion inside a tight "tube," and usage of receiver coils.
To our knowledge, only a few studies have investigated the patient experience of WB-MRI and compared it to other total body imaging modalities; they have shown some results on the acceptance of WB-MRI performed on 1.5T scanners, but none have focused on 3T scanners alone.
In our experience, the majority (90.3%) of patients appreciated WB-MRI and said they would probably undergo the procedure again. These data are in line with the studies by Adams et al. [28] and Oliveri et al. [29] in cancer patients and with those of Busacchio et al. [30] in self-referring asymptomatic subjects screening. In these studies, the WB-MRI performed on 1.5T scanners was well-accepted and considered more tolerable than other total body imaging modalities by most patients.
They discovered that a higher WB-MRI load was related to significant distress and comorbidities. In the experience of patients who had WB-MRI for screening, 98.5% felt high to a very high degree of usefulness, and 95.4% would repeat the examination [30].
Oliveri et al. [29] found that the level of WB-MRI acceptance was > 81% high or higher. Adam et al. found that WB-MRI was less concerning than CT, less unpleasant, and finally, patients felt better after WB-MRI.
Evans et al. [31, 32] investigated patient experience and acceptability of WB-MRI compared to standard staging imaging methods in patients affected by lung or colon rectal cancer enrolled in the Streamline line L and the Streamline line C trials, respectively. The overall satisfaction was lower for WB-MRI than PET/CT and, above all, compared to CE-CT. They also noted that WB-MRI is generally perceived as more stressful than other imaging techniques partly because of the potential, perceived by patients, to be able to detect a cancer diagnosis or additional elements associated with already known diagnoses that may result in a worse prognosis and different treatment implications (viewed both positively and negatively).
According to the study of Dyrberg et al. on the pleasure of WB-MRI in prostate cancer patients, WB-MRI had a satisfactory overall enjoyment level [33].
The Ryder A et al. study regarding patients affected by Myeloma demonstrated a high level of the overall satisfaction for both WB-MRI and other methods [34].
Our study and previous research showed that duration and noise are factors that negatively affect the WB-MRI experience, particularly in patients with pulmonary symptoms, pain, and/or claustrophobia, whereas staff support and information, as well as comfort during acquisition (posture and mental relaxation also through listening to music), are factors that increase the overall enjoyment of the method. Additionally, psychological assistance and relaxation techniques may be helpful.
Scan acceptability is greater in younger patients probably due to awareness of the long-life expectancy and risks associated with the use of ionizing radiation also known in the general population.
One potential limitation of this study is that even if we asked all patients who had undergone the WB-MRI to participate in the study, all those who interrupted the procedure refused to fill the questionnaire. Thus, the experience and acceptance of the techniques in this study population were probably more favorable compared to a background population. Another limitation of the study is that it did not investigate the relationship between acceptability and pantient’s level of education.
Conclusions
Our study reveals that WB-MRI exams are well-accepted by adult patients suffering from various types of malignancies and bone disorders. This is a good starting point when thinking about how to apply the technology in clinical practice because WB-MRI seems to be just as pleasant as other total body imaging modalities (PET/CT, CE-CT).
Evaluating a new imaging method through the eyes of the patients is an important factor in successfully developing and implementing WB-MRI in clinical practice. This analysis is essential to make our procedures more patient-friendly and offer a more patient-centered approach.
References
Tunariu N, Blackledge M, Messiou C, Petralia G, Padhani A, Curcean S, Curcean A, Koh DM (2020) What’s new for clinical whole-body MRI (WB-MRI) in the 21st century. Br J Radiol 93(1115):20200562. https://doi.org/10.1259/bjr.20200562
Donners R, Blackledge M, Tunariu N, Messiou C, Merkle EM, Koh DM (2018) Quantitative whole-body diffusion-weighted MR imaging. Magn Reson Imaging Clin N Am 26(4):479–494. https://doi.org/10.1016/j.mric.2018.06.002
Petralia G, Padhani AR (2018) Whole-body magnetic resonance imaging in oncology: uses and indications. Magn Reson Imaging Clin N Am 26(4):495–507. https://doi.org/10.1016/j.mric.2018.06.003
Gennari A, Andre F, Barrios CH, Cortes J, de Azambuja E, DeMichele A, Dent R, Fenlon D, Gligorov J, Hurvitz SA, Im SA, Krug D, Kunz WG, Loi S, Penault-Llorca F, Ricke J, Robson M, Rugo HS, Saura C, Schmid P, Singer CF, Spanic T, Tolaney SM, Turner NC, Curigliano G, Loibl S, Paluch-Shimon S, Harbeck N (2021) ESMO Clinical Practice Guideline for the diagnosis, staging and treatment of patients with metastatic breast cancer. Annals of oncology : official journal of the European Society for Medical Oncology 32(12):1475–1495. https://doi.org/10.1016/j.annonc.2021.09.019
Mottet N, van den Bergh RCN, Briers E, Van den Broeck T, Cumberbatch MG, De Santis M, Fanti S, Fossati N, Gandaglia G, Gillessen S, Grivas N, Grummet J, Henry AM, van der Kwast TH, Lam TB, Lardas M, Liew M, Mason MD, Moris L, Oprea-Lager DE, van der Poel HG, Rouvière O, Schoots IG, Tilki D, Wiegel T, Willemse PM, Cornford P (2021) EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer-2020 update. Part 1: screening, diagnosis, and local treatment with curative intent. Eur Urol 79(2):243–262. https://doi.org/10.1016/j.eururo.2020.09.042
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, Rubinstein L, Shankar L, Dodd L, Kaplan R, Lacombe D, Verweij J (2009) New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer 45(2):228–247. https://doi.org/10.1016/j.ejca.2008.10.026
Padhani AR, Koh DM (2011) Diffusion MR imaging for monitoring of treatment response. Magn Reson Imaging Clin N Am 19(1):181–209. https://doi.org/10.1016/j.mric.2010.10.004
Summers P, Saia G, Colombo A, Pricolo P, Zugni F, Alessi S, Marvaso G, Jereczek-Fossa BA, Bellomi M, Petralia G (2021) Whole-body magnetic resonance imaging: technique, guidelines and key applications. Ecancermedicalscience 15:1164. https://doi.org/10.3332/ecancer.2021.1164
Koutoulidis V, Terpos E, Papanikolaou N, Fontara S, Seimenis I, Gavriatopoulou M, Ntanasis-Stathopoulos I, Bourgioti C, Santinha J, Moreira JM, Kastritis E, Dimopoulos MA, Moulopoulos LA (2022) Comparison of MRI features of fat fraction and ADC for early treatment response assessment in participants with multiple myeloma. Radiology 304(1):137–144. https://doi.org/10.1148/radiol.211388
van Vucht N, Santiago R, Lottmann B, Pressney I, Harder D, Sheikh A, Saifuddin A (2019) The Dixon technique for MRI of the bone marrow. Skeletal Radiol 48(12):1861–1874. https://doi.org/10.1007/s00256-019-03271-4
Hillengass J, Usmani S, Rajkumar SV, Durie BGM, Mateos MV, Lonial S, Joao C, Anderson KC, Garcia-Sanz R, Riva E, Du J, van de Donk N, Berdeja JG, Terpos E, Zamagni E, Kyle RA, San Miguel J, Goldschmidt H, Giralt S, Kumar S, Raje N, Ludwig H, Ocio E, Schots R, Einsele H, Schjesvold F, Chen WM, Abildgaard N, Lipe BC, Dytfeld D, Wirk BM, Drake M, Cavo M, Lahuerta JJ, Lentzsch S (2019) International myeloma working group consensus recommendations on imaging in monoclonal plasma cell disorders. Lancet Oncol 20(6):e302–e312. https://doi.org/10.1016/S1470-2045(19)30309-2
Messiou C, Porta N, Sharma B, Levine D, Koh DM, Boyd K, Pawlyn C, Riddell A, Downey K, Croft J, Morgan V, Stern S, Cheung B, Kyriakou C, Kaczmarek P, Winfield J, Blackledge M, Oyen WJG, Kaiser MF (2021) Prospective evaluation of whole-body MRI versus FDG PET/CT for Lesion detection in participants with myeloma. Radiol Imaging Cancer 3(5):e210048. https://doi.org/10.1148/rycan.2021210048
Lowrance WT, Breau RH, Chou R, Chapin BF, Crispino T, Dreicer R, Jarrard DF, Kibel AS, Morgan TM, Morgans AK, Oh WK, Resnick MJ, Zietman AL, Cookson MS (2021) Advanced prostate cancer: AUA/ASTRO/SUO guideline part I. J Urol 205(1):14–21. https://doi.org/10.1097/JU.0000000000001375
Lowrance WT, Breau RH, Chou R, Chapin BF, Crispino T, Dreicer R, Jarrard DF, Kibel AS, Morgan TM, Morgans AK, Oh WK, Resnick MJ, Zietman AL, Cookson MS (2021) Advanced prostate cancer: AUA/ASTRO/SUO guideline part II. J Urol 205(1):22–29. https://doi.org/10.1097/JU.0000000000001376
Risks of antihypertensive therapy (1986). Lancet 2 (8515):1075–1076
Ahlawat S, Debs P, Amini B, Lecouvet FE, Omoumi P, Wessell DE (2022) Clinical applications and controversies of whole-body MRI: AJR expert panel narrative review. AJR Am J Roentgenol. https://doi.org/10.2214/AJR.22.28229
Petralia G, Zugni F, Summers PE, Colombo A, Pricolo P, Grazioli L, Colagrande S, Giovagnoni A, Padhani AR, Resonance IWGoM, (2021) Whole-body magnetic resonance imaging (WB-MRI) for cancer screening: recommendations for use. Radiol Med 126(11):1434–1450. https://doi.org/10.1007/s11547-021-01392-2
Zugni F, Padhani AR, Koh DM, Summers PE, Bellomi M, Petralia G (2020) Whole-body magnetic resonance imaging (WB-MRI) for cancer screening in asymptomatic subjects of the general population: review and recommendations. Cancer Imaging 20(1):34. https://doi.org/10.1186/s40644-020-00315-0
Carlsson S, Carlsson E (2013) “The situation and the uncertainty about the coming result scared me but interaction with the radiographers helped me through”: a qualitative study on patients’ experiences of magnetic resonance imaging examinations. J Clin Nurs 22(21–22):3225–3234. https://doi.org/10.1111/jocn.12416
Tornqvist E, Mansson A, Larsson EM, Hallstrom I (2006) It’s like being in another world–patients’ lived experience of magnetic resonance imaging. J Clin Nurs 15(8):954–961. https://doi.org/10.1111/j.1365-2702.2006.01499.x
Weintraub MI, Khoury A, Cole SP (2007) Biologic effects of 3 Tesla (T) MR imaging comparing traditional 1.5 T and 0.6 T in 1023 consecutive outpatients. J Neuroimaging 17(3):241–245. https://doi.org/10.1111/j.1552-6569.2007.00118.x
Itri JN (2015) Patient-centered radiology. Radiographics 35(6):1835–1846. https://doi.org/10.1148/rg.2015150110
Padhani AR, Lecouvet FE, Tunariu N, Koh DM, De Keyzer F, Collins DJ, Sala E, Schlemmer HP, Petralia G, Vargas HA, Fanti S, Tombal HB, de Bono J (2017) METastasis reporting and data system for prostate cancer: practical guidelines for acquisition, interpretation, and reporting of whole-body magnetic resonance imaging-based evaluations of multiorgan involvement in advanced prostate cancer. Eur Urol 71(1):81–92. https://doi.org/10.1016/j.eururo.2016.05.033
Messiou C, Hillengass J, Delorme S, Lecouvet FE, Moulopoulos LA, Collins DJ, Blackledge MD, Abildgaard N, Ostergaard B, Schlemmer HP, Landgren O, Asmussen JT, Kaiser MF, Padhani A (2019) Guidelines for acquisition, interpretation, and reporting of whole-body MRI in myeloma: myeloma response assessment and diagnosis system (MY-RADS). Radiology 291(1):5–13. https://doi.org/10.1148/radiol.2019181949
Petralia G, Padhani A, Summers P, Alessi S, Raimondi S, Testori A, Bellomi M (2013) Whole-body diffusion-weighted imaging: is it all we need for detecting metastases in melanoma patients? Eur Radiol 23(12):3466–3476. https://doi.org/10.1007/s00330-013-2968-x
Petralia G, Koh DM, Attariwala R, Busch JJ, Eeles R, Karow D, Lo GG, Messiou C, Sala E, Vargas HA, Zugni F, Padhani AR (2021) Oncologically relevant findings reporting and data system (ONCO-RADS): guidelines for the acquisition, interpretation, and reporting of whole-body MRI for cancer screening. Radiology 299(3):494–507. https://doi.org/10.1148/radiol.2021201740
Dantendorfer K, Amering M, Bankier A, Helbich T, Prayer D, Youssefzadeh S, Alexandrowicz R, Imhof H, Katschnig H (1997) A study of the effects of patient anxiety, perceptions and equipment on motion artifacts in magnetic resonance imaging. Magn Reson Imaging 15(3):301–306. https://doi.org/10.1016/s0730-725x(96)00385-2
Adams HJ, Kwee TC, Vermoolen MA, Ludwig I, Bierings MB, Nievelstein RA (2014) Whole-body MRI vs. CT for staging lymphoma: patient experience. Eur J Radiol 83(1):163–166. https://doi.org/10.1016/j.ejrad.2013.10.008
Oliveri S, Pricolo P, Pizzoli S, Faccio F, Lampis V, Summers P, Petralia G, Pravettoni G (2018) Investigating cancer patient acceptance of whole body MRI. Clin Imaging 52:246–251. https://doi.org/10.1016/j.clinimag.2018.08.004
Busacchio D, Mazzocco K, Gandini S, Pricolo P, Masiero M, Summers PE, Pravettoni G, Petralia G (2021) Preliminary observations regarding the expectations, acceptability and satisfaction of whole-body MRI in self-referring asymptomatic subjects. Br J Radiol 94(1118):20191031. https://doi.org/10.1259/bjr.20191031
Evans R, Taylor S, Janes S, Halligan S, Morton A, Navani N, Oliver A, Rockall A, Teague J, Miles A (2017) Patient experience and perceived acceptability of whole-body magnetic resonance imaging for staging colorectal and lung cancer compared with current staging scans: a qualitative study. BMJ Open 7(9):e016391. https://doi.org/10.1136/bmjopen-2017-016391
Evans RE, Taylor SA, Beare S, Halligan S, Morton A, Oliver A, Rockall A, Miles A (2018) Perceived patient burden and acceptability of whole body MRI for staging lung and colorectal cancer; comparison with standard staging investigations. Br J Radiol 91(1086):20170731. https://doi.org/10.1259/bjr.20170731
Dyrberg E, Larsen EL, Hendel HW, Thomsen HS (2018) Diagnostic bone imaging in patients with prostate cancer: patient experience and acceptance of NaF-PET/CT, choline-PET/CT, whole-body MRI, and bone SPECT/CT. Acta Radiol 59(9):1119–1125. https://doi.org/10.1177/0284185117751280
Ryder A, Parsons C, Hutchinson CE, Greaney B, Thake CD (2021) A survey study investigating perceptions and acceptance of the whole-body imaging techniques used for the diagnosis of myeloma. Radiography (Lond) 27(4):1149–1157. https://doi.org/10.1016/j.radi.2021.06.002
Funding
This study was partly funded by the Italian Ministry of Health for Institutional Research (Ricerca Corrente) within the research line "Innovative therapies, phase I-III clinical trials, and therapeutic strategy trials based on preclinical models, onco-immunological mechanisms, and nano vectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study's conception and design. A.R., D.D., and E.S. wrote the first draft of the study, which was edited and commented on by all the authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval and Consent to participate
This prospective study was approved by the Ethical Committee (IRST100.15), and all participants signed an informed consent form to be enrolled.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rossi, A., Prochowski Iamurri, A., Diano, D. et al. Patient centered radiology: investigating 3 Tesla whole body MRI acceptance in cancer patients. Radiol med 128, 960–969 (2023). https://doi.org/10.1007/s11547-023-01665-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-023-01665-y