Abstract
Purpose
To compare the positive predictive values (PPVs) of BI-RADS categories used to assess pure mammographic calcifications in women with and without a previous history of breast cancer (PHBC).
Materials and methods
In this retrospective study, all consecutive pure mammographic calcifications (n = 320) undergoing a stereotactic biopsy between 2016 and 2018 were identified. Mammograms were evaluated in consensus by two radiologists according to BI-RADS and blinded to patient history and pathology results. Final pathologic results were used as the standard of reference. PPV of BI-RADS categories were compared between the two groups. Data were evaluated using standard statistics, Mann–Whitney U tests and Chi-square tests.
Results
Two hundred sixty-eight patients (274 lesions, median age 54 years, inter-quartile range, 50–65 years) with a PHBC (n = 46) and without a PHBC (n = 222) were included. Overall PPVs were the following: BI-RADS 2, 0% (0 of 56); BI-RADS 3, 9.1% (1 of 11); BI-RADS 4a, 16.2% (6 of 37); BI-RADS 4b, 37.5% (48 of 128); BI-RADS 4c, 47.3% (18 of 38) and BI-RADS 5, 100% (4 of 4). The PPV of BI-RADS categories was similar in patients with and without a PHBC (P = .715). Calcifications were more often malignant in patients with a PHBC older than 10 years (47.3%, 9 of 19) compared to 1–2 years (25%, 1 of 4), 2–5 years (20%, 2 of 10) and 5–10 years (0%, of 13) from the first breast cancer (P = .005).
Conclusion
PPV of mammographic calcifications is similar in women with or without PHBC when BI-RADS classification is strictly applied. A higher risk of malignancy was observed in patients with a PHBC longer than 10 years.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Women surviving a first breast cancer remain at risk to develop a subsequent local or regional recurrence in the same breast or a new primary cancer in the contralateral breast. In this circumstance, an increased rate of distant metastases and breast cancer mortality has been observed [1, 2]. Based on the evidence that mammography in the screening as well as in the surveillance setting reduces breast cancer mortality, current surveillance guidelines recommend annual mammography to asymptomatic patients with a personal history of breast cancer [3,4,5,6,7,8].
Breast-conserving therapy instead of mastectomy has become the treatment of choice for early-stage breast cancer, given equivalent survival rates [9, 10]. However, due to the effect of the combination of post-surgical changes and radiotherapy, e.g., architectural distortion, skin thickening and dystrophic calcifications, image interpretation can be more challenging. In general, 2–3 years are necessary to achieve the stability of the post-treatment-induced modifications [11].
Calcifications represent about 30% of suspicious findings leading to recall in population-based screening [12]. Assessment of calcifications is commonly based on radiologist evaluation according to the Breast Imaging-Reporting and Data System (BI-RADS) [13]. Evaluation of morphology and distribution of calcifications along with their variations over time should ensure an accurate categorization of the calcifications, but in practice, differentiation of benign and malignant disease remains challenging with high interobserver variability and false-positive biopsy rates of up to 87% [14,15,16]. BI-RADS classification is based on the imaging evaluation and should be applied regardless of personal factors such as a personal history of breast cancer. Nevertheless, evaluation of calcifications may be biased when a personal history of breast cancer (PHBC) is known. Moreover, considering a higher cancer rate than in women without PHBC and an interval cancer rate up to 35%, a biopsy could be more often recommended also in case of calcifications at low risk of malignancy [17,18,19].
We hypothesized that, if BI-RADS categorization is strictly applied in the assessment of calcifications, no differences in the clinical outcome are present between patients with and without a PHBC. The purpose of this study is to compare the positive predictive values (PPVs) of the BI-RADS categories used to assess mammographic calcifications in women with and without a PHBC.
Material and methods
The institutional review board approved this retrospective study. The requirement for written informed consent was waived.
Study population
All consecutive calcifications for which a stereotactic biopsy was performed from June 1, 2016, through May 31, 2018, at the Department of Oncologic Radiation Therapy and Diagnostic Imaging (Centro di Riferimento Oncologic, Aviano) were identified from the institutional radiology–pathology database. The following inclusion criteria were applied: (1) availability of digital mammograms or magnification views preceding the biopsy, (2) asymptomatic patients with calcifications without associated masses, asymmetries or architectural distortion, (3) patients with a PHBC with a follow-up period of at least 12 months and a first cancer stage 0–III, (4) final pathology result from either stereotactic biopsy or subsequent surgical excision for all lesions with a biopsy-proven diagnosis of malignancy, uncertain malignant potential or radiologic–pathologic discordance. The following cases were excluded: (1) patients undergoing 6-month follow-up examination for probably benign findings (BI-RADS 3), (2) patients with known BRCA mutation, (3) benign diagnosis after stereotactic biopsy with lack of imaging follow-up of at least 24 months, (4) patients with known simultaneous breast cancer in the ipsilateral or contralateral breast. Final pathologic results were used as the standard of reference.
Data collection
In women without a PHBC, the following data were collected: information regarding incident or prevalent screening, a personal history of percutaneous biopsy or surgical excision for other than malignant lesions was recorded. In patients with a PHBC, the following data were collected: time since the first breast cancer diagnosis; histologic type; cancer stage; surgical method; adjuvant radiation therapy; adjuvant chemotherapy or endocrine therapy. Information regarding menopausal status and family history, except in case of known BRCA mutation, was not always available and has therefore not been included in further analyses.
Imaging evaluation
The craniocaudal/mediolateral oblique mammogram or the magnification view containing the calcifications was evaluated in consensus by two radiologists with each 9 years of experience in breast imaging (M.M. and N.B.). The radiologists were informed about the position of the calcifications, if calcifications were a new finding or increasing compared to prior mammograms or if no previous mammograms were available for comparison. In case of multiple groups of calcifications in the same quadrant, the distance from the nipple of calcifications under investigation was also provided. A table with detailed specifications for the calcification assessment according to BI-RADS was provided (Online Appendix), and the ACR BI-RADS Atlas was available with calcification examples with corresponding categorization. The morphology and distribution of the calcifications and the corresponding BI-RADS category were annotated. No patient-related clinical information and pathology outcomes were provided.
Statistical analysis
Descriptive statistics were used to summarize the characteristics of the patients and the lesions. The Mann–Whitney U test was used to compare age of patients with and without a PHBC. Data concerning pathology at diagnosis for the two groups and data from patients with a PHBC were analyzed with Chi-square and post hoc comparison; Bonferroni correction was applied for evaluating significance (P < 0.05/10 = 0.005 and P < 0.05/8 = 0.006). The PPV for calcification morphology, distribution and BI-RADS classifications was calculated by dividing the number of cases of malignancy (invasive or ductal in situ cancer) by the total number of cases in each category. The Wilcoxon signed rank test was used to compare the PPVs of calcification morphology and distribution as well as the PPV of the BI-RADS categories in patients with and without history of breast cancer. The PPV of the dataset from the original read-out (PPV1) was calculated by dividing the number of cases of malignancy (invasive cancer or ductal carcinoma in situ (DCIS)) by the total number of cases which underwent biopsy. All statistical calculations were performed using SPSS software (SPSS, version 22.0; SPSS), and P < 0.05 was considered to indicate statistical significance except for the Bonferroni corrections.
Results
Patient characteristics and pathology results
A flowchart of the cases included for analysis is shown in Fig. 1. A total of 268 women (median age, 54 years [interquartile range (IQR), 50–65 years]) with 274 lesions were included in this study. A PHBC was present in 46 of 268 (17.1%) patients (61 years, [IQR, 54–71 years]), and no PHBC was present in 222 of 268 (82.9%) patients (54 years, [IQR, 49–64 years]) (P = 0.0002). In patients with a PHBC, the median age was not significantly different between the subgroup with newly diagnosed malignancy (60.5 years, [IQR, 54–71 years]) and the subgroup with a benign histologic diagnosis (62.5 years, [IQR, 54–71 years](P = 0.881). Similarly, in patients without a PHBC, the median age was not significantly different between the subgroup with newly diagnosed malignancy (54 years, [IQR, 54–71 years]) and the subgroup with a benign histologic diagnosis (53 years, [IQR, 50–67 years](P = 0.881).
In patients without a PHBC mammography was performed as prevalent screening in 31 of 222 (14.0%) cases and as incident screening in 191 of 222 (86.0%) cases. A biopsy was performed bilaterally in 6 of 222 (2.7%) cases. A previous history of surgical excision for other than malignant lesions was present in 14 of 222 (6.3%) of patients, and the stereotactic biopsy was performed in the contralateral and in the ipsilateral breast in 4 of 14 (28.6%) and 10 of 14 (71.4%) cases, respectively.
In patients with a PHBC, 2 of 46 (4.3%) had a previous synchronous bilateral carcinoma, 3 of 46 (6.5%) had a history of bilateral breast cancer in 10-, 13- and 18-years’ time interval between the two cancers, and 1 of 46 (2.2%) had a history of local recurrence after 5 years from the first breast cancer diagnosis. Mastectomy was performed in 10 of 46 (21.7%) patients. In 22 (47.8%) cases, calcifications were also present at previous cancer diagnosis; in 18 (39.2%) cases no calcifications were present, whereas in 6 (13.0%) cases no information regarding imaging features of previous cancer was available.
Pathology results after either stereotactic biopsy or subsequent surgical excision are reported in Table 1. DCIS (67 of 274 lesions, 24.5%) was overall the most frequent diagnosis followed by atypical ductal hyperplasia (64 of 274 lesions, 23.3%). Sclerosing adenosis (12 of 46 lesions, 17.5%) was the most frequent diagnosis in women with a PHBC followed by DCIS and usual ductal hyperplasia (both 10 of 46 lesions, 21.7%). Atypical ductal hyperplasia (60 of 228 lesions, 26.3%) was the most frequent diagnosis in women without a PHBC followed by DCIS (57 of 228 lesions, 25%).
Imaging findings and BI-RADS categorization
Calcifications were new compared to a previous examination in 92 of 274 (33.6%) cases, 14 of 46 (30.4%) patients with a PHBC and 78 of 228 (34.2%) patients without a PHBC. Calcifications were increasing in number compared to a previous examination in 137 of 274 (50%) cases, 30 of 46 (65.2%) patients with a PHBC and 107 of 228 (46.9%) patients without a PHBC. No previous examinations were available for comparison in 45 of 274 (16.4%) cases, 2 of 46 (4.4%) patients with a PHBC and 43 of 228 (18.9%) patients without a PHBC.
Morphology and distribution of calcifications as well as the corresponding PPV are reported in Table 2. Calcifications classified according to morphology and distribution had a similar proportion of cases in patients with or without a PHBC (P = .917 and P = .686, respectively). The PPV of morphology and distribution in patients with or without a PHBC was similar (P = .434 and .089, respectively).
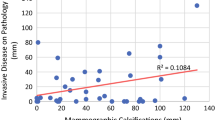
Overall PPVs were the following: BI-RADS 2, 0% (0 of 56); BI-RADS 3, 9.1% (1 of 11, Fig. 2); BI-RADS 4a, 16.2% (6 of 37); BI-RADS 4b, 37.5% (48 of 128); BI-RADS 4c, 47.3% (18 of 38); and BI-RADS 5, 100% (4 of 4). The PPV of BI-RADS categories was similar in patients with and without a PHBC (P = .715, Table 3). Considering all lesions with risk of malignancy >2% (BI-RADS 4 and 5 category) the PPV was 36.7% (76 malignancy of 207 cases) overall, 40% (12 malignancy out of 30 cases) in patients with a PHBC and 36.1% (64 malignancy out of 177 cases) in patients without a PHBC (P = .687). Considering the dataset from the original read-out of calcifications which underwent stereotactic biopsy (i.e., including BI-RADS category 2 and 3), the PPV1 was 28.1% (77 malignancy out of 274 lesions) overall, 26.1% (12 malignancy out of 46 cases) in patients with a PHBC and 28.5% (65 malignancy out of 228 cases) in patients without a PHBC (P=.858).
Mediolateral oblique mammogram (a) and corresponding magnification (b) of a 54-year-old woman without a personal history of breast cancer. Compared to a previous examination, new punctate calcifications (three calcifications, rectangle in A) were detected in the prepectoral region and classified as BI-RADS 3. Calcifications corresponded to low-grade ductal carcinoma in situ
Among patients with a PHBC 16 of 46 lesions (34.8%) underwent biopsy for BIRADS 2 calcifications compared to 42 of 228 lesions (18.4%) patients without a PHBC (P=.013).
Patients with personal history of breast cancer
Characteristics of women with a PHBC are reported in Table 4. In 27 of 46 (58.7%) cases, biopsy was performed in the ipsilateral and in 19 of 46 (41.3%) in the contralateral breast compared to the first breast cancer. A malignancy was diagnosed in the contralateral breast in 5 of 12 (41.7%) patients and in the ipsilateral breast in 7 of 12 (58.3%) patients. Only 1 of 12 (8.3%) patients had previous bilateral cancer.
In patients with previous breast cancer diagnosis 1–2 years before biopsy, only one contralateral malignancy was found (25%, 1 of 4 cases, Figs. 3 and 4). In patients with a previous breast cancer diagnosis 2–5 years before the biopsy, calcifications were malignant in 2 of 10 cases (20%) with one malignancy in the ipsilateral breast (10.0%) and one malignancy in the contralateral breast (10.0%). In patients with a previous breast cancer diagnosis 5–10 years before the biopsy, no calcifications were malignant (0 of 13 cases, 0%). In patients with a previous cancer diagnosis over 10 years before, calcifications were malignant in 9 of 19 (47.3%) cases, 6 of 9 (66.7%) in the ipsilateral breast and in 3 of 9 (33.3%) in the contralateral breast. No differences were observed in patients with benign and malignant calcifications diagnosis comparing the characteristics of previous breast cancer and the therapy approach (P > 0.024).
Magnification view (mediolateral oblique projection) of the upper quadrants of the right breast in a 55-year-old woman undergoing follow-up mammography one year after breast conserving surgery for invasive ductal carcinoma in the contralateral breast. Compared to a previous examination, new fine pleomorphic grouped calcifications (white arrow) were detected in the upper outer quadrant of the right breast and classified as BI-RADS 4b. Calcifications corresponded to usual ductal hyperplasia
Magnification view (craniocaudal projection) of the outer left breast in a 63-year-old woman undergoing follow-up mammography one year after breast conserving surgery for invasive lobular carcinoma in the contralateral breast. Compared to a previous examination, new fine pleomorphic grouped calcifications (white arrow) were detected in the upper outer quadrant of the left breast and classified as BI-RADS 4b. Calcifications corresponded to high-grade ductal carcinoma in situ
Discussion
BI-RADS classification of breast calcifications is based on specific imaging features and should be applied regardless of personal factors such as a personal history of breast cancer (PHBC). Nevertheless, evaluation of calcifications may be biased when a PHBC is known. Our study showed a similar PPV for each BI-RADS category in patients with and without PHBC (36.7% vs. 40%; P = .687). Comparing calcification assessment blinded to the patient history to the original evaluation in the diagnostic setting, we found that a greater percentage of cases with BI-RADS 2 calcifications has undergone biopsy in the group of patients with a PHBC (34.8%) compared to the group without a PHBC (18.4%, P = .013). These data indicate that unnecessary biopsies may be partly avoided when calcification evaluation is based on their morphology, distribution and increase over time without accounting for a PHBC.
Assessment of breast calcifications can be challenging. Previous studies have reported a PPV of less than 30% for calcification classification [16, 20,21,22]. Moreover, a fair to moderate agreement among multiple readers is described in case of calcification assessment based on morphology and distribution [23,24,25]. To improve the accuracy of calcification evaluation, in our study all images were analyzed in consensus by two radiologists specialized in breast imaging and specifications for calcification assessment according to BI-RADS were provided. Considering all lesions with a risk of malignancy > 2%, we found a PPV of 36.7% proving that a strict use of BI-RADS classification can be used to improve accuracy in calcification assessment [26].
From BI-RADS category 2–5, a progressive PPV was found in both groups of patients. A PPV of 9.1% for lesions categorized BI-RADS 3 was higher than that commonly reported, and it can be explained by the low number of cases included in this category with only one case of malignancy, i.e., low-grade DCIS (13). BI-RADS category 4 encompasses a wide range of malignancy, and use of subcategories is suggested in order to provide a more detailed risk stratification assessment, a more accurate radiologic–pathologic correlation and ultimately support patient treatment decisions. Nevertheless, BI-RADS 4 subcategories remain scarcely applied, particularly in calcification assessment despite the proven advantages in terms of risk assessment [14, 16, 27]. In our study, we found a progressive risk of malignancy from category 4a to c, although with a slightly higher percentage for category 4a (16.2%) and a slightly lower percentage for category 4c (47.3%) compared to the corresponding expected ranges (2–10% and 51–95%). The PPV of morphology and distribution categories were similar in patients with or without PHBC (P = 0.144 and P = 0.068, respectively).
In patients with and without a PHBC, DCIS was similarly the most frequent diagnosis of malignancy (21.7% and 25.0%, respectively). The percentage of cases with ADH was higher in patients without a PHBC than in patients with a PHBC (26.3% and 8.7%, respectively). Although antihormonal therapy (e.g., tamoxifen and aromatase inhibitor) seems to reduce the incidence of clinically detected benign breast disease and could in part explain this finding, we found that a similar percentage of other benign lesions was present in the two groups of patients [28].
In patients with a PHBC of more than 10 years about 47% of the biopsied calcifications were malignant compared to 12.5% in case of breast cancer in 1–10 years before the biopsy. A malignancy was diagnosed in the contralateral breast in 41.7% patients and in the ipsilateral breast in 58.3% patients. Previous works reported that tumor recurrences at the original tumor site are in observed at a rate up to 2.5% per year between 2 and 6 years after treatment and are in general due to local treatment failure [29, 30]. Local imaging findings in the first two years after treatment usually represent benign lesions and cancer diagnosed after 10 years are usually new malignancies in a different site or in the contralateral breast [31]. A number of factors including breast cancer subtype, breast cancer treatment and stage are known to be associated with local recurrence. In our study, these factors did not differ between women with malignant and benign calcifications, but this could be also due to the limited number of cases included for each category [32].
Our study has some limitations. First, a single projection or magnification was provided for the calcification evaluation and no previous examinations were available for comparison. Although the growth rate could be not directly assessed, information regarding calcification increase over time was provided to increase the accuracy in the calcification assessment [33]. Second, in case of ipsilateral calcifications in patients with a PHBC, the presence of postoperative changes could have biased the evaluation. Nevertheless, fourteen patients without a PHBC and previous breast surgical excision have also been included. Third, the study was performed in an oncology referral center with a high proportion of patients in follow-up after breast cancer treatment and our results could may not be generalizable to other diagnostic settings. Fourth, family history was not considered owing to partly unavailable information. Finally, a limited number of cases were included and we are aware that a matched-population-based study would have strengthened the significance of our findings.
In conclusion, our study demonstrates that the PPV of calcifications is similar in women with or without PHBC when BI-RADS classification is applied. Calcification assessment should be based only on their morphology, distribution and increase over time. In case of suspicious calcifications in patients with a PHBC longer than 10 years we observed a higher risk of malignancy.
Abbreviations
- BI-RADS:
-
Breast Imaging-Reporting and Data System
- PHBC:
-
Personal History of Breast Cancer
- PPV:
-
Positive predictive value
References
Anderson SJ, Wapnir I, Dignam JJ et al (2009) Prognosis after ipsilateral breast tumor recurrence and locoregional recurrences in patients treated by breast-conserving therapy in five National Surgical Adjuvant Breast and Bowel Project protocols of node-negative breast cancer. J Clin Oncol 27:2466–2473. https://doi.org/10.1200/JCO.2008.19.8424
Komoike Y, Akiyama F, Iino Y et al (2006) Ipsilateral breast tumor recurrence (IBTR) after breast-conserving treatment for early breast cancer: risk factors and impact on distant metastases. Cancer 106:35–41. https://doi.org/10.1002/cncr.21551
Wernli KJ, Ichikawa L, Kerlikowske K et al (2019) Surveillance breast MRI and mammography: comparison in women with a personal history of breast cancer. Radiology 292:311–318. https://doi.org/10.1148/radiol.2019182475
Monticciolo DL, Newell MS, Moy L et al (2018) Breast cancer screening in women at higher-than-average risk: recommendations from the ACR. J Am Coll Radiol 15:408–414. https://doi.org/10.1016/j.jacr.2017.11.034
Cardoso F, Kyriakides S, Ohno S et al (2019) Early breast cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol 30:1194–1220. https://doi.org/10.1093/annonc/mdz173
Lu WL, Jansen L, Post WJ, Bonnema J, Van de Velde JC, De Bock GH (2009) Impact on survival of early detection of isolated breast recurrences after the primary treatment for breast cancer: a meta-analysis. Breast Cancer Res Treat 114:403–412. https://doi.org/10.1007/s10549-008-0023-4
Paszat L, Sutradhar R, Grunfeld E et al (2009) Outcomes of surveillance mammography after treatment of primary breast cancer: a population-based case series. Breast Canceres Treat 114:169–178. https://doi.org/10.1007/s10549-008-9986-4
Buist DSM, Abraham L, Lee CI et al (2018) Breast biopsy intensity and findings following breast cancer screening in women with and without a personal history of breast cancer. JAMA Intern Med 178:458–468. https://doi.org/10.1001/jamainternmed.2017.854
Fisher B, Anderson S, Bryant J et al (2002) Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med 347:1233–1241. https://doi.org/10.1056/NEJMoa022152
Veronesi U, Cascinelli N, Mariani L et al (2002) Twenty-year follow-up of a randomized study comparing breast-conserving surgery with radical mastectomy for early breast cancer. N Engl J Med 347:1227–1232. https://doi.org/10.1056/NEJMoa020989
Chansakul T, Lai KC, Slanetz PJ (2012) The postconservation breast: part 1, expected imaging findings. Am J Roentgenol 198:321–330. https://doi.org/10.2214/AJR.10.7298
Bluekens AM, Holland R, Karssemeijer N, Broeders MJ, den Heeten GJ (2012) Comparison of digital screening mammography and screen-film mammography in the early detection of clinically relevant cancers: a multicenter study. Radiology 265:707–714. https://doi.org/10.1148/radiol.12111461
Sickles E DOC, Bassett LW, et al. (2013) BI-RADS: Mammography, 5th edn. In: Breast imaging reporting and data system: ACR BI-RADS–breast imaging atlas. American College of Radiology, Reston
Bent CK, Bassett LW, D’Orsi CJ, Sayre JW (2010) The positive predictive value of BI-RADS microcalcification descriptors and final assessment categories. AJR Am J Roentgenol 194:1378–1383. https://doi.org/10.2214/AJR.09.3423
Berg WA, Arnoldus CL, Teferra E, Bhargavan M (2001) Biopsy of amorphous breast calcifications: pathologic outcome and yield at stereotactic biopsy. Radiology 221:495–503. https://doi.org/10.1148/radiol.2212010164
Burnside ES, Ochsner JE, Fowler KJ et al (2007) Use of microcalcification descriptors in BI-RADS 4th edition to stratify risk of malignancy. Radiology 242:388–395. https://doi.org/10.1148/radiol.2422052130
Buist DS, Abraham LA, Barlow WE et al (2010) Diagnosis of second breast cancer events after initial diagnosis of early stage breast cancer. Breast Cancer Res Treat 124:863–873. https://doi.org/10.1007/s10549-010-1106-6
Houssami N, Abraham LA, Miglioretti DL et al (2011) Accuracy and outcomes of screening mammography in women with a personal history of early-stage breast cancer. JAMA 305:790–799. https://doi.org/10.1001/jama.2011.188
Lu W, Schaapveld M, Jansen L et al (2009) The value of surveillance mammography of the contralateral breast in patients with a history of breast cancer. Eur J Cancer 45:3000–3007. https://doi.org/10.1016/j.ejca.2009.08.007
Kettritz U, Rotter K, Schreer I et al (2004) Stereotactic vacuum-assisted breast biopsy in 2874 patients: a multicenter study. Cancer 100:245–251. https://doi.org/10.1002/cncr.11887
Liberman L, Abramson AF, Squires FB, Glassman JR, Morris EA, Dershaw DD (1998) The breast imaging reporting and data system: positive predictive value of mammographic features and final assessment categories. AJR Am J Roentgenol 171:35–40. https://doi.org/10.2214/ajr.171.1.9648759
Rominger M, Wisgickl C, Timmesfeld N (2012) Breast microcalcifications as type descriptors to stratify risk of malignancy: a systematic review and meta-analysis of 10665 cases with special focus on round/punctate microcalcifications. Rofo 184:1144–1152. https://doi.org/10.1055/s-0032-1313102
Berg WA, Campassi C, Langenberg P, Sexton MJ (2000) Breast imaging reporting and data system: inter- and intraobserver variability in feature analysis and final assessment. AJR Am J Roentgenol 174:1769–1777. https://doi.org/10.2214/ajr.174.6.1741769
Lazarus E, Mainiero MB, Schepps B, Koelliker SL, Livingston LS (2006) BI-RADS lexicon for US and mammography: interobserver variability and positive predictive value. Radiology 239:385–391. https://doi.org/10.1148/radiol.2392042127
Lee AY, Wisner DJ, Aminololama-Shakeri S et al (2017) Inter-reader variability in the use of BI-RADS descriptors for suspicious findings on diagnostic mammography: a multi-institution study of 10 academic radiologists. Acad Radiol 24:60–66. https://doi.org/10.1016/j.acra.2016.09.010
Timmers JM, van Doorne-Nagtegaal HJ, Verbeek AL, den Heeten GJ, Broeders MJ (2012) A dedicated BI-RADS training programme: effect on the inter-observer variation among screening radiologists. Eur J Radiol 81:2184–2188. https://doi.org/10.1016/j.ejrad.2011.07.011
Elezaby M, Li G, Bhargavan-Chatfield M, Burnside ES, DeMartini WB (2018) ACR BI-RADS assessment category 4 subdivisions in diagnostic mammography: utilization and outcomes in the national mammography database. Radiology 287:416–422. https://doi.org/10.1148/radiol.2017170770
Tan-Chiu E, Wang J, Costantino JP et al (2003) Effects of tamoxifen on benign breast disease in women at high risk for breast cancer. J Natl Cancer Inst 95:302–307. https://doi.org/10.1093/jnci/95.4.302
Kreike B, Hart AA, van de Velde T et al (2008) Continuing risk of ipsilateral breast relapse after breast-conserving therapy at long-term follow-up. Int J Radiat Oncol Biol Phys 71:1014–1021. https://doi.org/10.1016/j.ijrobp.2007.11.029
Bucchi L, Belli P, Benelli E et al (2016) (2016) Recommendations for breast imaging follow-up of women with a previous history of breast cancer: position paper from the Italian Group for Mammography Screening (GISMa) and the Italian College of Breast Radiologist (ICBR) by SIRM. Radiol Med 121:891–896. https://doi.org/10.1007/s11547-016-0676-8
Chansakul T, Lai KC, Slanetz PJ (2012) The postconservation breast: part 2, Imaging findings of tumor recurrence and other long-term sequelae. AJR Am J Roentgenol 198:331–343. https://doi.org/10.2214/AJR.11.6881
Lam DL, Houssami N, Lee JM (2017) Imaging surveillance after primary breast cancer treatment. AJR Am J Roentgenol 208:676–686. https://doi.org/10.2214/AJR.16.16300
Grimm LJ, Miller MM, Thomas SM et al (2019) Growth dynamics of mammographic calcifications: differentiating ductal carcinoma in situ from benign breast disease. Radiology 292:77–83. https://doi.org/10.1148/radiol.2019182599
Funding
Open access funding provided by University of Zurich. This work was supported by a grant of “Promedica-Stiftung” to M. Marcon. The funding source was not involved in study design, in collection, analysis and interpretation of data in manuscript writing or in the decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation and data collection were performed by VB, MU and MLG. Image analysis was performed by NB and MM. Data analysis was performed by VB and MM. The first draft of the manuscript was written by VB and MM, and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethical approval
The institutional review board approved this retrospective study (CRO-2019-83). The requirement for written informed consent was waived.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bertani, V., Berger, N., Eberhard, M. et al. Mammographic calcifications undergoing percutaneous biopsy: outcome in women with and without a personal history of breast cancer. Radiol med 128, 149–159 (2023). https://doi.org/10.1007/s11547-022-01583-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-022-01583-5