Abstract
Purpose
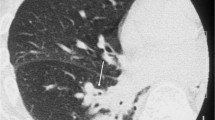
The authors sought to assess the role of highresolution computed tomography (HRCT) in the detection and follow-up of nontuberculous mycobacteria (NTM) pulmonary infection in immunocompetent patients and to identify the most common radiological patterns for diagnosis.
Materials and methods
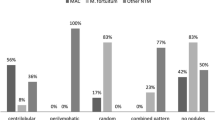
Plain chest radiographs and HRCT scans of 42 consecutive patients with NTM pulmonary infection (M/F 26/16; mean age 57, range 41–83) were retrospectively reviewed. Ten of these patients were followed up for 18 months after diagnosis. Small nodules (<10 mm), nodules 10- to 30-mm in diameter, lobar/segmental consolidation, cavitations, bronchiectasis and tree-in-bud pattern were analysed.
Results
Small nodules were more frequent than nodules 10- to 30-mm in diameter, and segmental consolidation was more frequent than lobar. Cavitations, tree-in-bud and bronchiectasis were more frequently located in the upper lobes. Four of the followed-up patients had cavitation of preexisting nodules, and five had progression of bronchiectasis.
Conclusions
HRCT allows accurate detection and followup of the most frequent presentation patterns: diffuse small nodules, bronchiectasis, upper lobe segmental consolidation and cavitations. The appearance of new bronchiectasis and progression of old disease are due to pulmonary infection.
Riassunto
Obiettivo
Valutare il ruolo dell’HRCT nell’infezione polmonare da micobatteri atipici non tubercolari (NTMB) all’esordio ed in corso di follow-up ed identificare i reperti radiologici più rappresentativi di diagnosi.
Materiali e metodi
Abbiamo valutato gli esami Rx/TC a strato sottile (HRCT spessore 1 mm/interslice 10 mm) relativi a 42 casi consecutivi di infezione polmonare da NTMB, insorta in pazienti immunocompetenti (M/F, 26/16; età media 57 anni; range 41–83); abbiamo eseguito il follow-up in 10 casi entro 18 mesi dalla diagnosi. Abbiamo ricercato la presenza di micro e macronoduli, consolidazioni parenchimali, cavitazioni, bronchiectasie, tree-in-bud.
Risultati
La micronodulia (<10 mm) è più frequente della macronodulia, la consolidazione segmentaria della lobare; le cavitazioni, il tree-in-bud, le bronchiectasie sono più frequenti nei lobi superiori. Nel follow-up in 4 casi si è avuta cavitazione dei noduli, in 5 progressione delle bronchiectasie.
Conclusioni
L’HRCT consente la corretta identificazione ed il monitoraggio a distanza del pattern che più frequentemente si riscontra nella localizzazione polmonare dell’infezione: micronodulia diffusa, bronchiectasie, consolidazione segmentaria lobare superiore, cavità. La comparsa di nuove bronchiectasie e la progressione delle preesistenti è connessa all’infezione.
Similar content being viewed by others
References/Bibliografia
Jeong YJ, Lee KS, Koh WJ et al (2004) Nontuberculous mycobacterial pulmonary infection in immunocompetent patients: comparision of thin-section CT and histopathologic findings. Radiology, 231: 880–886
Koh WJ, Lee KS, Kwon OJ et al (2005) Bilateral bronchiectasis and bronchiolitis at thin-section CT: diagnostic implication in nontuberculous mycobacterial pulmonary infection. Radiology 235: 282–288
Corbett EL, Blumberg L, Churchyard GJ et al (1999) Nontuberculous mycobacteria defining disease in a prospective cohort of south african miners. Am J Respir Crit Care Med 160: 15–21
Henry MT, Inamdar L, O’Riordain D et al (2004) Nontuberculous mycobacteria in non-HIV patients: epidemiology, treatment and response. Eur Respir J 23: 741–746
Davies PDO (1994) Infection with nontuberculous mycobacteria. Br J Hosp Med 52: 375–377
Runyon EH (1959) Anonymous mycobacteria in pulmonary disease. Med Clin North Am 43: 273–290
Wolinsky E (1992) Mycobacterial diseases other than tuberculosis. Clin Infect Dis 15: 1–12
Erasmus JJ, McAdams HP, Farrell MA, Patz EF Jr (1999) Pulmonary nontuberculous mycobacterial infection: radiologic manifestations. Radiographics 19: 1487–1505
Field SK, Fischer D, Cowie RL (2004) Mycobacterim avium complex pulmonary disease in patients without HIV infection. Chest 126: 566–581
Primm TP, Lucero CA, Falkinham JO 3rd (2004) Health impacts of environmental mycobacteria. Clin Microbiol Rev 17: 98–106
American Thoracic Society (1997) Diagnosis and treatment of disease caused by nontuberculous mycobacteria. Am J Resp Crit Care Med 156: S21–S25
Lynch DA, Simone PM, Fox MA et al (1995) CT features of pulmonary mycobacterium avium complex infection. J Comput Assist Tomogr 19: 353–360
Katoch VM (2004) Infections due to non-tuberculous mycobacteria. Indian J Med Res 120: 290–304
Fujita J, Ohtsuki I, Suemitsu I et al (1999) Pathological and radiological changes in resected lung specimens in Mycobacterium avium intracellulare complex disease. Eur Respir J 13: 535–540
Prince DS, Peterson DD, Steiner RM et al (1989) Infection with Mycobacterium avium complex in patients without predisposing conditions. N Engl J Med 321: 863–868
Kubo K, Yamazaki Y, Hachiya T et al (1998) Mycobacterium aviumintracellulare pulmonary infection in patients without known predisposing lung disease. Lung 176: 381–391
Miller WT Jr (1994) Spectrum of pulmonary nontuberculous mycobacterial infection. Radiology 191: 343–350
Wittram C, Weisbrod GL (2002) Mycobacterium avium complex lung disease in immunocompetent patients: radiography-CT correlation. Br J Radiol 75: 340–344
Griffith DE, Aksamit T, Brown-Elliott BA et al (2007) An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med Vol 175: 367–416
Tuddenham WJ (1984) Glossary of terms for thoracic radiology: recommendations of the Nomenclature Committee of the Fleischner Society. AJR Am J Roentgenol 143: 509–517
Austin JMH, Muller NL, Freidman PJ et al (1996) Glossary of terms for CT of the lungs: recommendations of the Nomenclature Committee of the Fleischner Society. Radiology 200: 327–331
Hartman TE, Swensen SJ, Williams DE (1993) Mycobacterium avium intracellulare complex: evaluation with CT. Radiology 187: 23–26
Reich JM, Johnson RE (1992) Mycobacterium avium complex pulmonary disease presenting as an isolated lingular or middle lobe pattern. The Lady Windermere syndrome. Chest 101: 1605–1609
Moore EH (1993) Atypical mycobacterial infection in the lung: CT appearance. Radiology 187: 777–782
Aronchick JM, Miller WT, Epstein DM, Gefter WB (1986) Association of achalasia and pulmonary Mycobacterium fortuitum infection. Radiology 160: 85-86
Primack SL, Logan PM, Hartman TE et al (1995) Pulmonary tuberculosis and Mycobacterium avium-intracellulare: a comparison of CT findings. Radiology 194: 413–417
Wickremasinghe M, Ozerovitch LJ, Davies G et al (2005) Non-tuberculous mycobacteria in patients with bronchiectasis. Thorax 60: 1045–1051
Woodring JH, Vandiviere HM (1990) Pulmonary disease caused by nontuberculous mycobacteria. J Thorac Imaging 5: 64–76
Nelson KG, Griffith DE, Brown BA et al (1998) Results of operation in Mycobacterium avium intracellulare lung disease. Ann Thorac Surg 66: 325–330
Pomerantz M, Madsen L, Goble M et al (1991) Surgical management of resistant Mycobacterial tuberculosis and other Mycobacterial pulmonary infections. Ann Thorac Surg 52: 1108–1112
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ferrara, I., Cappabianca, S., Brunese, L. et al. HRCT in detection of pulmonary infections from nontuberculous mycobacteria: personal experience. Radiol med 114, 376–389 (2009). https://doi.org/10.1007/s11547-009-0375-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-009-0375-9