Abstract
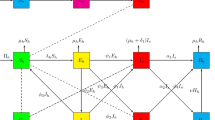
The developing world has been facing a significant health issue due to cholera as an endemic communicable disease. Lusaka was Zambia’s worst affected province, with 5414 reported cases of cholera during the outbreak from late October 2017 to May 12, 2018. To explore the epidemiological characteristics associated with the outbreak, we fitted weekly reported cholera cases with a compartmental disease model that incorporates two transmission routes, namely environment-to-human and human-to-human. Estimates of the basic reproduction number show that both transmission modes contributed almost equally during the first wave. In contrast, the environment-to-human transmission appears to be mostly dominating factor for the second wave. Our study finds that a massive abundance of environmental vibrio’s with a huge reduction in water sanitation efficacy triggered the secondary wave. To estimate the expected time to extinction (ETE) of cholera, we formulate the stochastic version of our model and find that cholera can last up to 6.5–7 years in Lusaka if any further outbreak occurs at a later time. Results indicate that a considerable amount of attention is to be paid to sanitation and vaccination programs in order to reduce the severity of the disease and to eradicate cholera from the community in Lusaka.






Similar content being viewed by others
Data Availability
The data are obtained form the Zambian Ministry of Health database and from “Zambia Cholera Outbreak Situation Report” available at https://www.afro.who.int/countries/zambia/situation-reports/cholera).
References
Al-Abri SS, Beeching NJ, Nye FJ (2005) Traveller’s diarrhoea. Lancet Infect Dis 5(6):349–360
Ali M, Lopez AL, You YA, Kim YE, Sah B, Maskery B, Clemens J (2012) The global burden of cholera. Bull World Health Organ 90(3):209–218
Ali M, Nelson AR, Lopez AL, Sack DA (2015) Updated global burden of cholera in endemic countries. PLoS Negl Trop Dis 9(6):0003832
Andersson H, Britton T (2000) Stochastic epidemics in dynamic populations: quasi-stationarity and extinction. J Math Biol 41(6):559–580
Andrews JR, Basu S (2011) Transmission dynamics and control of cholera in Haiti: an epidemic model. The Lancet 377(9773):1248–1255
Britton T (2010) Stochastic epidemic models: a survey. Math Biosci 225:24–35
Chowell G (2017) Fitting dynamic models to epidemic outbreaks with quantified uncertainty: a primer for parameter uncertainty, identifiability, and forecasts. Infect Dis Model 2(3):379–398
Chowell G, Luo R (2021) Ensemble bootstrap methodology for forecasting dynamic growth processes using differential equations: application to epidemic outbreaks. BMC Med Res Methodol 21(1):1–18
Chowell G, Ammon C, Hengartner N, Hyman J (2006) Transmission dynamics of the great influenza pandemic of 1918 in Geneva, Switzerland: assessing the effects of hypothetical interventions. J Theor Biol 241(2):193–204
Chowell G, Tariq A, Hyman JM (2019) A novel sub-epidemic modeling framework for short-term forecasting epidemic waves. BMC Med 17(1):1–18
Chowell G, Luo R, Sun K, Roosa K, Tariq A, Viboud C (2020) Real-time forecasting of epidemic trajectories using computational dynamic ensembles. Epidemics 30:100379
Clemens J, Harris J, Khan MR, Kay B, Yunus M, Svennerholm A-M, Sack D, Chakraborty J, Stanton B, Khan M et al (1986) Field trial of oral cholera vaccines in Bangladesh. The Lancet 328(8499):124–127
Codeço CT (2001) Endemic and epidemic dynamics of cholera: the role of the aquatic reservoir. BMC Infect Dis 1(1):1–14
Emch M, Feldacker C, Islam MS, Ali M (2008) Seasonality of cholera from 1974 to 2005: a review of global patterns. Int J Health Geogr 7(1):1–13
Gardiner CW et al (1985) Handbook of Stochastic Methods. Springer, Berlin
Hartley DM, Morris JG Jr, Smith DL (2006) Hyperinfectivity: a critical element in the ability of v. cholerae to cause epidemics? PLoS Med 3(1):7
Kabwe P, Moonde L, Gama A, Hadunka F, Sinyange N, Kateule E, Inambao A, Mwamba M, Zulu G, Kumar R (2017) Descriptive characterization of the cholera outbreak in Lusaka district, 2016. The Health Press
Kapata N, Sinyange N, Mazaba ML, Musonda K, Hamoonga R, Kapina M, Zyambo K, Malambo W, Yard E, Riggs M et al (2018) A multisectoral emergency response approach to a cholera outbreak in Zambia: October 2017-february 2018. J Infect Dis 218((suppl-3):181–183
King AA, Ionides EL, Pascual M, Bouma MJ (2008) Inapparent infections and cholera dynamics. Nature 454(7206):877–880
Legros D (2018) Global cholera epidemiology: opportunities to reduce the burden of cholera by 2030. J Infect Dis 218(suppl–3):137–140
Levine M, Black R, Clements M, Cisneros L, Nalin D, Young C (1981) Duration of infection-derived immunity to cholera. J Infect Dis 143(6):818–820
Longini IM Jr, Nizam A, Ali M, Yunus M, Shenvi N, Clemens JD (2007) Controlling endemic cholera with oral vaccines. PLoS Med 4(11):336
Lucas ME, Deen JL, Von Seidlein L, Wang X-Y, Ampuero J, Puri M, Ali M, Ansaruzzaman M, Amos J, Macuamule A et al (2005) Effectiveness of mass oral cholera vaccination in Beira, Mozambique. N Engl J Med 352(8):757–767
Luque Fernández MÁ, Bauernfeind A, Jiménez JD, Gil CL, Omeiri NE, Guibert DH (2009) Influence of temperature and rainfall on the evolution of cholera epidemics in Lusaka, Zambia, 2003–2006: analysis of a time series. Trans R Soc Trop Med Hyg 103(2):137–143
Marino S, Hogue IB, Ray CJ, Kirschner DE (2008) A methodology for performing global uncertainty and sensitivity analysis in systems biology. J Theor Biol 254(1):178–196
Martcheva M (2015) An introduction to mathematical epidemiology, vol 61. Springer, New York
McKay MD, Beckman RJ, Conover WJ (2000) A comparison of three methods for selecting values of input variables in the analysis of output from a computer code. Technometrics 42(1):55–61
Miller Neilan RL, Schaefer E, Gaff H, Fister KR, Lenhart S (2010) Modeling optimal intervention strategies for cholera. Bull Math Biol 72(8):2004–2018
Mukandavire Z, Liao S, Wang J, Gaff H, Smith DL, Morris JG Jr (2011) Estimating the reproductive numbers for the 2008–2009 cholera outbreaks in Zimbabwe. Proc Natl Acad Sci 108(21):8767–8772
Mukandavire Z, Tripathi A, Chiyaka C, Musuka G, Nyabadza F, Mwambi H (2011) Modelling and analysis of the intrinsic dynamics of cholera. Differ Equ Dynam Syst 19(3):253–265
Mwaba J, Debes AK, Shea P, Mukonka V, Chewe O, Chisenga C, Simuyandi M, Kwenda G, Sack D, Chilengi R et al (2020) Identification of cholera hotspots in Zambia: a spatiotemporal analysis of cholera data from 2008 to 2017. PLoS Negl Trop Dis 14(4):0008227
Mwaba J, Debes AK, Murt KN, Shea P, Simuyandi M, Laban N, Kazimbaya K, Chisenga C, Li S, Almeida M et al (2021) Three transmission events of vibrio cholerae o1 into Lusaka, Zambia. BMC Infect Dis 21(1):1–7
Naficy A, Rao MR, Paquet C, Antona D, Sorkin A, Clemens JD (1998) Treatment and vaccination strategies to control cholera in sub-saharan refugee settings: a cost-effectiveness analysis. JAMA 279(7):521–525
Nasell I (1999) On the time to extinction in recurrent epidemics. J. R. Statist. Soc. B 61:309–330
Nelson EJ, Harris JB, Glenn Morris J, Calderwood SB, Camilli A (2009) Cholera transmission: the host, pathogen and bacteriophage dynamic. Nat Rev Microbiol 7(10):693–702
Posny D, Wang J, Mukandavire Z, Modnak C (2015) Analyzing transmission dynamics of cholera with public health interventions. Math Biosci 264:38–53
Righetto L, Casagrandi R, Bertuzzo E, Mari L, Gatto M, Rodriguez-Iturbe I, Rinaldo A (2012) The role of aquatic reservoir fluctuations in long-term cholera patterns. Epidemics 4(1):33–42
Roosa K, Chowell G (2019) Assessing parameter identifiability in compartmental dynamic models using a computational approach: application to infectious disease transmission models. Theor Biol Med Model 16(1):1–15
Saltelli A, Tarantola S, Campolongo F, Ratto M et al (2004) Sensitivity analysis in practice: a guide to assessing scientific models. England, Chichester
Sanches RP, Ferreira CP, Kraenkel RA (2011) The role of immunity and seasonality in cholera epidemics. Bull Math Biol 73(12):2916–2931
Sardar T, Mukhopadhyay S, Bhowmick AR, Chattopadhyay J (2013) An optimal cost effectiveness study on Zimbabwe cholera seasonal data from 2008–2011. PLoS ONE 8(12):81231
Sasaki S, Suzuki H, Igarashi K, Tambatamba B, Mulenga P (2008) Spatial analysis of risk factor of cholera outbreak for 2003–2004 in a peri-urban area of Lusaka, Zambia. Am J Trop Med Hyg 79(3):414–421
Sasaki S, Suzuki H, Fujino Y, Kimura Y, Cheelo M (2009) Impact of drainage networks on cholera outbreaks in Lusaka, Zambia. Am J Public Health 99(11):1982–1987
Sinyange N, Brunkard JM, Kapata N, Mazaba ML, Musonda KG, Hamoonga R, Kapina M, Kapaya F, Mutale L, Kateule E et al (2018) Cholera epidemic-Lusaka, Zambia, October 2017-may 2018. Morb Mortal Wkly Rep 67(19):556
Sur D, Lopez AL, Kanungo S, Paisley A, Manna B, Ali M, Niyogi SK, Park JK, Sarkar B, Puri MK et al (2009) Efficacy and safety of a modified killed-whole-cell oral cholera vaccine in India: an interim analysis of a cluster-randomised, double-blind, placebo-controlled trial. The Lancet 374(9702):1694–1702
Tappero JW, Tauxe RV (2011) Lessons learned during public health response to cholera epidemic in Haiti and the dominican republic. Emerg Infect Dis 17(11):2087
Thiem VD, Deen JL, Von Seidlein L, Anh DD, Park J-K, Ali M, Danovaro-Holliday MC, Son ND, Hoa NT, Holmgren J et al (2006) Long-term effectiveness against cholera of oral killed whole-cell vaccine produced in Vietnam. Vaccine 24(20):4297–4303
World Health Organization (2017) Ending cholera a global roadmap to 2030, p 32
World Health Organization (2022) Cholera situation report. https://www.who.int/health-topics/cholera#tab=tab_1. Accessed 5 May 2022
Yang C, Wang J (2019) A cholera transmission model incorporating the impact of medical resources. Math Biosci Eng 16(5):5226–5246
Zuckerman JN, Rombo L, Fisch A (2007) The true burden and risk of cholera: implications for prevention and control. Lancet Infect Dis 7(8):521–530
Acknowledgements
The authors are grateful to the anonymous referees for their careful reading, valuable comments, and helpful suggestions, which helped us to improve the quality of this work. B. M. is supported by Senior Research Fellowship from University Grants Commission (UGC), India.
Author information
Authors and Affiliations
Contributions
B.M. took part in methodology, formal analysis, software, writing—original draft, writing—review & editing. B. S. involved in conceptualization, methodology, software, supervision, writing—review & editing. I. G. involved in conceptualization, methodology, supervision, writing —review & editing. J. C. took part in supervision, conceptualization, writing—review & editing.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendix A: Results with Normal Error Structure
Appendix A: Results with Normal Error Structure
Fitting the model (1) to the weekly reported cholera cases in Lusaka, Zambia, for the \(1\textrm{st}\) wave. The empirical distributions of each estimated parameter are illustrated by the histograms using 1000 bootstrap replicates with normal error structure. The location of the true values of the parameters is marked as vertical dotted yellow lines. Here reported discrete data points are represented by blue circles, while the best fit of the model to the data is depicted by the solid red line in the bottom-left panel. The dashed red lines demonstrate 95% confidence bands around the best-fit line. Also, 1000 epidemic curves considering normal error structure (with mean the best-fit solution and deviation 20% of the mean) exhibited by the sky-blue lines (Color figure online)
Fitting the model (1) to the weekly reported cholera cases in Lusaka, Zambia, for the \(2\textrm{nd}\) wave. The empirical distributions of each estimated parameter are illustrated by the histograms using 1000 bootstrap replicates with normal error structure. The location of the true values of the parameters is marked as vertical dotted yellow lines. Here reported discrete data points are represented by blue circles, while the best fit of the model to the data is depicted by the solid red line in the bottom-left panel. The dashed red lines demonstrate 95% confidence bands around the best-fit line. Also, 1000 epidemic curves considering normal error structure (with mean the best-fit line and deviation 20% of the mean) exhibited by the cyan lines. We observe that during the second wave, the rate of environment-to-human transmission increases drastically (about 52%) due to the high abundance of environmental vibrio’s. Also, water sanitation efficiency (\(\rho \)) decreases significantly (about 44%) during this period (Color figure online)
We consider bootstrap realizations assuming normal error structures in the data and estimate parameters for both waves to assure that results revealed by our study are robust in the context of chosen error structure. For the normal error structure, we consider 1000 bootstrap replicates from the best-fitted curve with the best-fit solution as the mean and a deviation of 20% of the mean. The empirical distribution and 95% confidence interval for each of the estimated parameters associated with both waves are depicted in Figs. 7 and 8, respectively. In addition, estimated \(\mathcal {R}_0\) with its partial partitions (\(\mathcal {R}_e\), \(\mathcal {R}_h\)) is provided in Table 2. It can be seen that during the second wave, \(\rho \) decreased by about 44%, and transmission from the environment was mostly responsible (estimated \(\mathcal {R}_e\) was 90% of \(\mathcal {R}_0\)). Although the mean values of the estimated parameters are almost the same with both error structures, the uncertainty ranges of the estimated parameters with a normal error structure are wider than those obtained using the Poisson error structure in the data. The estimated ETE of cholera in Lusaka with normal error structure is found to be about 7 years which assures the robustness of the results in the context of chosen error structure in the data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Maity, B., Saha, B., Ghosh, I. et al. Model-Based Estimation of Expected Time to Cholera Extinction in Lusaka, Zambia. Bull Math Biol 85, 55 (2023). https://doi.org/10.1007/s11538-023-01149-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11538-023-01149-0