Abstract
Integrated strategies of community health promotion (ISCHP) are based on intersectoral collaborations using the Health in All Policies approach to address determinants of health. While effects on health determinants have been shown, evidence on the effectiveness of ISCHP on health outcomes is scarce. The aim of this study is to assess the long-term effects of ISCHP on diabetes mellitus mortality (DMM) in German communities. A nonrandomized evaluation based on secondary county-level official data (1998–2016) was performed. In April 2019, 149 communities in Germany with ISCHP out of 401 were identified. Communities with < 5 measurements of DMM, starting before 1999 or after 2015, were excluded. Analyses included 65 communities with ISCHP (IG) and 124 without ISCHP (CG). ISCHP ran for a mean of 5.6 years. Fixed effects (FE) models were used to estimate effects of ISCHP and duration on DMM taking into account the time-varying average age. The FE estimator for DMM is b = − 2.48 (95% CI − 3.45 to − 1.51) for IG vs. CG and b = − 0.30 (95% CI − 0.46 to − 0.14) for ISCHP duration (0–16 years). In the first year of an ISCHP, a reduction of the annual DMM of 0.3 per 100,000 population (1%), and in the 16th year of 4.8 (14%) was achieved. This study provides preliminary evidence of the effectiveness of ISCHP in Germany. Limitations include inaccuracies to classify IG and CG and possible selection bias. Longitudinal county-level data may be an efficient data source to evaluate complex interventions, thereby contributing to further strengthen evidence-based integrated health promotion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Health in All Policies (HiAP) describes a holistic societal model in which policies are applied as interventions to promote the health of a population [1]. Interventions based on HiAP typically target at communities or settings and may address various health-related sectors [1]. The WHO mentioned the concept of HiAP in 2010 in a statement; however, numerous HiAP-like interventions have been implemented (long) before, such as the WHO Healthy Cities movement, showing that by targeting the population as a whole including the physical and social environment, even modest changes of determinants of health may have a large public health impact [2]. In line with this population-based strategy, research focused on developing, implementing, and evaluating comprehensive community prevention approaches (CCPA) based on socioecological models [3]. While meta-analyses and systematic reviews provide clear evidence on the effectiveness of CCPA on health behaviours, evidence on health consequences like morbidity or mortality remains inconsistent [4,5,6,7].
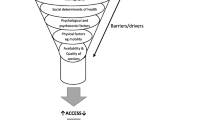
In Germany, communities have started to establish Integrated Strategies of Community Health Promotion (ISCHP), since the late 1980s with starting the German Healthy Cities Network [8]. ISCHP are CCPA based on the framework of health determinants and of Health in All Policies (HiAP) [1, 9]. Meanwhile, several initiatives at the state and federal levels support ISCHP [8]. The model in Fig. 1 shows possible causal pathways between the intervention ISCHP and the expected outcomes including important mediating and moderating parameters. Typically, ISCHP mediated by policy-induced changes in health determinants need a longer latency period to produce measurable effects on health outcomes. However, as ISCHP have so far evaluated only in a formative way despite a sufficient period of time, evidence on their effectiveness is still lacking [8, 10].
To examine retrospectively the effect of ISCHP on health, we classified the initiation of an ISCHP or not as a natural policy experiment as policies were not initiated or allocated by the researchers [13, 14]. We chose diabetes mortality as a relevant health outcome because we assumed that health outcomes related to diabetes mellitus are sensitive to ISCHP as healthy diet and promotion of physical activity are common (intermediate) targets of ISCHP [15, 16]. Further reasons include that diabetes is highly prevalent in Germany contributing to a substantial burden of disease and the data availability [17, 18]. We used fixed effects analysis, thereby taking advantage of the longitudinal data and of implicitly eliminating time-invariant (socioeconomic) confounders to enhance validity/causality. The two leading hypotheses of our study are (1) diabetes mellitus mortality (DMM) increases less/decreases more in communities, which initiated an ISCHP; (2) this effect is stronger the longer ISCHP runs.
Methods
This evaluation follows the ‘Transparent Reporting of Evaluations with Nonrandomized Designs’ (TREND) statement [19]. Ethical approval was obtained from the Ethics Committee of Hannover Medical School (reference number 10052_BO_K_2021).
Study Design, Assignment Method, and Eligibility
We used a natural policy experiment to retrospectively evaluate the long-term effects of ISCHP on DMM in German communities (counties and independent towns) [20, 21]. The assignment method is self-selection from comparison group (communities without ISCHP since 1998) by default into the intervention group by initiating an ISCHP in the years 1999 to 2015. The units of analysis are communities. Due to the holistic approach of ISCHP, with the exception of non-modifiable variables like age, gender, genetics, ethnicity, and supra-regional events and trends, all determinants of health that community can influence do no more represent potential confounders rather than mediating variables (Fig. 1). Based on McDowell et al. [22], we understand ISCHP as a population determinant to be captured by a global measure and DMM as an individual outcome that can be captured by an aggregated measure. Our analyses include county-level time series data of yearly DMM between 1998 and 2016. Eligible were all communities with a minimum of 5 years data available on the number of persons who died of diabetes mellitus, an annual sequence was not required. Excluded were all communities that initiated an ISCHP before 1999 or after 2015.
Data Sources and Data Linkage
Exposure (ISCHP as the self-selected intervention): We used databases, member registers, and grey literature [E-Supplement] to identify all German communities (independent towns, counties, towns, and rural communities) with an ISCHP (n = 214). The starting year was the year in which these communities first either participated in a program aimed at building an ISCHP or launched a project to build an ISCHP. We use the latter as a proxy measure for the year the communities initiated the ISCHP. Data collection took part in April 2019.
Outcome diabetes mellitus mortality (DMM): County-level data of the years 1998 to 2016 on population size (n = 489) and number of death of diabetes mellitus (n = 243) were downloaded from www.regionalstatistik.de in May 2019. County-level data of relevant time-varying confounders for the years from 1998 to 2016 on the mean age, proportion of foreigners, and proportion of women were downloaded from www.inkar.de in May 2019.
Data on exposure that not already referred to the county-level were manually aggregated to this level. Next, exposure data were manually merged with the data from www.inkar.de using the municipality names. As both the data from www.inkar.de and the data from www.regionalstatistik.de include the official municipality key, these data could be merged in an automated way using IBM SPSS Version 26.
Intervention and Comparison Conditions
Communities with an ISCHP
ISCHP is described as an overall strategic and coordinated approach and the collaboration of various society and policy sectors with the aim of creating health-promoting living environments and services [23]. ISCHP address a range of determinants of health and a range of target groups with special attention to increasing the health opportunities for people in socioeconomic risk situations [23]. To this end, preventive services and measures are coordinated across municipal departmental boundaries and with the involvement of actors from outside the administration and the target groups [23]. Therefore ISCHP require a form of steering that is based on collaboration and consensus-building and coordinates both horizontally between different society and policy sectors and vertically between different levels of action [23]. A central role in steering played the municipal administration [23]. The German Cooperation Network ‘Equity in Health’ published five booklets about how to develop and maintain an ISCHP. There are further guidelines to implement an ISCHP [24, 25].
Communities without an ISCHP
It can be assumed that in Germany, even in communities without ISCHP, concepts and principles are used that belong to the core features of an ISCHP. However, the prevention strategy in communities without an ISCHP is certainly less holistic, addresses only a few target groups and health outcomes, and therefore focuses only on a subset of the social determinants of health. Assumingly, in communities without an ISCHP, intersectoral networking and collaboration is less intensive in most cases.
Statistical Analysis
Linear fixed effects (FE) models were used to estimate the effects of the time-varying independent variables ISCHP initiation and of ISCHP duration on the time-varying dependent variable DMM [26]. FE models completely ignore the between-unit variation and use only within-unit variation to estimate the effects of time-varying independent variables on a time-varying dependent variable. Consequently, FE model estimates are completely controlled for all (un)observed time-invariant variables. Relevant time-varying variables have to be observed and to be considered in the model to get unbiased estimates [14, 26]. The FE models were conducted in two ways using IBM SPSS Version 26. (A) The FE models presented in tables were modelled using the least squares dummy variable (LSDV) approach [26]. Here, the units of analysis (communities) included in the model are coded as dummy variables. Since graphical and test-statistical analysis could not exclude heteroscedasticity, the FE models were computed with robust standard errors [27]. (B) The FE models presented in the grouped scatter plots are based on FE transformation that subtracts the unit-specific mean value (the mean of all time points) for each time-varying variable and performs an ordinary least squares (OLS) regression with these demeaned data [26, 28].
Dependent Variable
The time-varying health outcome measure is the crude annual diabetes mellitus mortality rate per 100,000 residents in the communities for the years 1998 to 2016. This rate was calculated using annually reported data on population size and persons who died from diabetes mellitus. For some analyses, we performed a FE transformation on this variable.
Independent Variables
The initiation of an ISCHP was coded as a time-variant dichotomous variable. For the year 1998, this variable was set to 0 for all communities. The value 0 indicates that the community does not have an ISCHP (comparison group). Communities that did not initiate an ISCHP between 1999 and 2015 have a value of 0 in this variable for all years. For communities that initiated an ISCHP between 1999 and 2015, this variable was then given a value of 1 from the year of initiation. The second outcome, the duration of the ISCHP, was coded as a time-variant quasi-metric (ordinal) variable. This variable was also set to the value 0 for all communities for the year 1998 that means there is no ISCHP running in the community. Communities that did not initiate an ISCHP from 1999 to 2015 have a value of 0 in this variable for all years. Communities that initiated an ISCHP during this period have a value of 1 in the year of initiation, and for subsequent years this value increased by 1 each year. It should be noted that this variable thus reflects the interaction effect of ISCHP initiation (0 = no ISCHP vs. 1 = ISCHP initiated) and ISCHP duration (range: 0–17 years), because the product of these two variables is equivalent of ISCHP duration.
Time-Variant Covariates
As a measure of the changing age structure, we used a time-varying variable on the community-specific average age. As measures of changing proportions of migrants and women, we used time-varying variables on the municipality-specific proportion of migrants and proportion of women. The time trend was coded as a time-varying quasi-metric (ordinal) variable. For the year 1998, the variable has the value 0 and for the following years, the value increases by 1 each year. Due to consistently missing values in 2011 for the dependent variable, the year 2011 was not included in the analyses.
At the beginning of the analyses, outliers were identified in the DMM data. This analysis shows that data points with a DMM > 75 per 100,000 represent outliers. Of the total 3402 data points in our dataset, 244 (7%) were identified as outliers and excluded. Excluded data were equally distributed in the IG and CG. Next, the change-in-estimate-criterion was used to analyse which of the time-varying covariates should be included as confounders in the FE models [29]. While including the average age into the model changes the effect estimate for ISCHP initiation by 322%, including the proportion of immigrants changes the effect estimate by only 3% and the proportion of women by 2%. Therefore, the FE models have been adjusted for average age only. In FE models, time-constant covariates (e.g. baseline values or geographic location) are always fully controlled for. As analysis on collinearities of the independent variables (ISCHP duration, time trend, and average age) detects collinearity between time trend and average age (r = 0.649; p < 0.001), only one of the two variables is included in the FE models.
Results
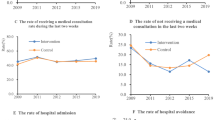
Of all 401 German communities (counties and independent towns), we identified 149 who had initiated an ISCHP and 252 who had not (Fig. 2). Exclusion of communities with fewer than five data points for the outcome and of communities who initiated an ISCHP before 1999 or after 2015 resulted in an intervention group (IG) of 65 and a control group (CG) of 124 communities. The ISCHP duration ranged from 1 to 17 years with a mean duration of 5.6 years (median: 5 years). The mean number of annual data points for the outcome measurement is 17 (range: 7–18) out of possible 18 data points. In 1998, the mean DMM was 19.1 per 100,000 in the future IGs and 25.7 per 100,000 in the CG (Table 1). In 2007, the DMM was approximately 26 in both groups and increased to 28.0 in the IGs and to 38.5 per 100,000 in the CGs by 2016.
The communities of the IG are more often located in West Germany and include more often independent towns compared to the CG (Table 1). The mean population size of the IG is larger compared to the CG. The mean proportion of women, the mean birth rate, and the mean age are equally distributed in both groups. The mean proportion of migrants, of the highest school qualification, the mean unemployment rate, the mean tax power, and the age-standardized mortality are slightly higher in the IG compared to the CG.
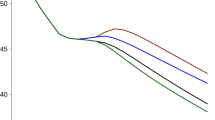
Figure 3 shows that communities having initiated ISCHP experienced a nearly stable DMM (increase of 0.0007 per 100,000 and year), while communities of the CG developed an increase in DMM of 0.54 per 100,000 and year. The DMM in communities with more than 10 years of ISCHP duration tended to decrease (Fig. 3).
Starting/duration of ISCHP and trend in annual diabetes mortality over time. Legend: Grouped scatter plot of the demeaned DMM (each data point represents the deviation of the mean DMM of one IG or CG from its own mean DMM over time) during 1998–2016. OLS regression analysis using these demeaned DMM qualifies as a FE regression. Groups are IG (n = 65; observations = 334) and CG (n = 124; observations = 2824), respectively, groups are IG with ISCHP of 1–10 years (n = 60; observations 308), IG with ISCHP of more than 10 years duration (n = 5; observations 308), and CG without ISCHP (n = 124; observations 2,824)
In communities with ISCHP, FE model analysis found a mean annual decline in DMM of 2.5 per 100,000 persons compared to the CG (Table 2). A higher average age was associated with an increased DMM. The duration of ISCHP was negatively associated with the DMM (Table 2). Each year with ISCHP, the DMM reduces on average by 0.3 per 100,000 persons, decreasing to an annually DMM by 4.8 per 100,000 persons after 16 years of ISCHP. Analyses included ISCHP with a mean duration of 4.4 years ranging from 1 to 16. A higher average age was associated with a higher DMM.
Discussion
We retrospectively analysed the effect of ISCHP started between 1999 and 2015 on diabetes mortality using a natural experiment based on aggregated longitudinal secondary data on county-level. From all 401 German communities, we included 65 as IG und 125 as CG. The FE models showed that ISCHP are associated with an average absolute reduction of DMM of 2.5 per 100,000 persons each year they run. A longer duration was associated with higher effects. To our knowledge, this is the first summative evaluation of ISCHP in Germany.
Applying advanced methods based on the latest research knowledge to provide evidence on the effects of complex health promotion programs is one of the major strengths of our study. There is a broad consensus that natural experiments and quasi-experimental study designs are appropriate for evaluating the effectiveness of CCPA [13, 14, 20, 30]. This is especially true when the focus is on population-level effects. The FE analysis we used is one out of six statistical analysis methods recommended to validly analyse data of non-randomized studies [14]. A major advantage of FE analyses is that they lead to conservative parameter estimates being close to the true value [14]. Other studies have also shown that time series analysis of small-area-level data is appropriate to demonstrate long-term effects of complex public health interventions [31,32,33].
Compared to randomized studies, natural experiments or quasi-experimental studies are prone to baseline imbalances. In this study, we cannot exclude a selection bias as the communities had chosen whether to start ISCHP or not and the reason for their decision remained unknown. Motivation to implement ISCHP could either include concerns on community health as well as to further promote health in already health-conscious, well-being communities. Comparing the available socio-demographic indicators in 1998 between IG and CG, no consistent result emerges to the question whether one study group might be more privileged than the other one. However, time constant confounders are automatically adjusted for in FE models.
Our results are in line with two other long-term community-based prevention programs. The Stockholm Diabetes Prevention Program cumulatively reduced DMM by 436 per 10,000 in men and 53 in women over 10 years [34]. Another study found a long-term effect for the Mexican diabetes prevention program PREVENIMSS with a reduction in DMM of 3.6 per 100,000 per year [35]. While these effects are higher than our results, this can at least be explained by the fact that ISCHG did not focus on DM prevention but could include a wide range of prevention targets and target groups, e.g. children.
Important limitations of our study may result from measurement inaccuracies of the exposure including the starting year, level of implementation, and intensity of the ISCHP-based programs. The year when a community joined a program to establish an ISCHP may only be a crude indicator for the year the community actually started the ISCHP-based interventions, which is more of a process. Interventions may have been started either years before joining the program or may not be completed until years after joining the program. The German Cooperation Network 'Equity in Health' distinguishes three levels of implementing an ISCHP [36]: sporadic informal integration, ongoing partially formalised integration, or ongoing fully formalized integration; we could not account for this characteristic (which is also changing over time) due to lacking data. Besides, our data do not include distinctions in the priorities of the various ISCHP that affect the intensity, the target groups, or the composition of the measures. For example, ISCHP focussing on programs such as No Child Left Behind (KeKiz) have certainly no or only a marginal direct effect on DMM. However, participating in an ISCHP program may reflect a fundamental, ‘beneficial to health’ attitude of a community leading to better overall health outcomes. However, these inaccuracies would underestimate the effect of ISCHP. Future evaluations should include more precise characteristics on each ISCHP associated program.
We cannot exclude a contamination of the CG. Even those communities that do not belong to a program for building an ISCHP may apply concepts and principles belonging to the core elements of an ISCHP. However, the prevention strategy in communities without an ISCHP is certainly less holistic and addresses only a subset of the social determinants of health or only a few target groups and health outcomes. Furthermore, in communities without an ISCHP, intersectoral networking and collaboration is supposed to be less intensive. In spite of these possible overlaps of IG and CG, we found positive effects in favour of the IG suggesting even higher effects of ISCHP on DMM.
Performing FE analyses, we found a notable reduction in DMM—a highly prevalent and relevant health outcome. We cannot exclude a selection bias. However, further inaccuracies to classify IG and CG tend to underestimate the ISCHP effect. In sum, our retrospective study provides at least preliminary evidence on the effectiveness of ISCHP in Germany. Further efforts should address thorough development and implementation of high-quality evaluation methods to further strengthen evidence-based integrated health promotion. Longitudinal county-level data may be an efficient data source to evaluate complex interventions.
References
Kickbusch I, Buckett K, Eds. Implementing Health In All Policies: Adelaide 2010. Department Of Health, Government Of South Australia; 2010.
Rose G. Sick Individuals And Sick Populations. Int J Epidemiol. 2001;30(3):427–32; Discussion 433–4. https://doi.org/10.1093/Ije/30.3.427
Nissinen A, Berrios X, Puska P. Community-based noncommunicable disease interventions: lessons from developed countries for developing ones. Bull World Health Organ. 2001;79(10):963–970. Published November 1, 2001.
Anderson Lm, Adeney Kl, Shinn C, Safranek S, Buckner-Brown J, Krause Lk. Community coalition-driven interventions to reduce health disparities among racial and ethnic minority populations. Cochrane Database Syst Rev. 2015;(6):Cd009905. https://doi.org/10.1002/14651858.Cd009905.Pub2
Bagnall A-M, Radley D, Jones R, et al. Whole systems approaches to obesity and other complex public health challenges: a systematic review. BMC Public Health. 2019;19(1):8. https://doi.org/10.1186/S12889-018-6274-Z
Nickel S, Von Dem KO. Do multiple community-based interventions on health promotion tackle health inequalities? Int J Equity Health. 2020;19(1):157. https://doi.org/10.1186/S12939-020-01271-8
O'mara-Eves A, Brunton G, Oliver S, Kavanagh J, Jamal F, Thomas J. The effectiveness of community engagement in public health interventions for disadvantaged groups: a meta-analysis. Bmc Public Health. 2015;15:129. https://doi.org/10.1186/S12889-015-1352-Y
Böhm K, Gehne D. Vernetzte Kommunale Gesundheitsförderung Für Kinder Und Jugendliche : Überblick Über Den Status Quo In Deutschland. Bundesgesundheitsbl. 2018;61(10):1208–14. https://doi.org/10.1007/S00103-018-2803-2
Dahlgren G, Whitehead M. Policies and strategies to promote social equity in health: background document to who – strategy paper for Europe. Arbetsrapport/Institutet För Framtidsstudier. 2007;(14).
Ehlen S, Dreiskämper D, Utesch T, Rehaag R. Integrierte Gesamtansätze Kommunaler Gesundheitsförderung Für Kinder. Präv Gesundheitsf. 2018;13(3):254–60. https://doi.org/10.1007/S11553-018-0640-7
Mielck A, Kilian H, Lehmann F, Richter-Kornweitz A, Kaba-Schönstein L. German Cooperation-Network ’Equity In Health’-Health Promotion In Settings. Health Promot Int. 2018;33(2):318–24. https://doi.org/10.1093/Heapro/Daw069
Plümer Kd, Kennedy L, Trojan A. Evaluating the implementation of the who healthy cities programme across Germany (1999–2002). Health Promot Int. 2010;25(3):342–354. https://doi.org/10.1093/Heapro/Daq028
Craig P, Katikireddi Sv, Leyland A, Popham F. Natural experiments: an overview of methods, approaches, and contributions to public health intervention research. Annu Rev Public Health. 2017;38:39–56. https://doi.org/10.1146/Annurev-Publhealth-031816-044327
Hu Y, Van Lenthe Fj, Hoffmann R, Van Hedel K, Mackenbach Jp. Assessing the impact of natural policy experiments on socioeconomic inequalities in health: how to apply commonly used quantitative analytical methods? Bmc Med Res Methodol. 2017;17(1):68. https://doi.org/10.1186/S12874-017-0317-5
Peimani M, Nasli-Esfahani E, Shakibazadeh E. Ottawa Charter Framework as a guide for type 2 diabetes prevention and control in Iran. J Diabetes Metab Disord. 2019;18(1):255–61. https://doi.org/10.1007/S40200-018-0381-3
Andersson Cm, Bjärås G, Tillgren P, Östenson C-G. A longitudinal assessment of inter-sectoral participation in a community-based diabetes prevention programme. Soc Sci Med. 2005;61(11):2407–2422. https://doi.org/10.1016/J.Socscimed.2005.04.032
Plass D, Vos T, Hornberg C, Scheidt-Nave C, Zeeb H, Krämer A. Trends in disease burden in germany: results, implications and limitations of the global burden of disease study. Dtsch Arztebl Int. 2014;111(38):629–38. https://doi.org/10.3238/Arztebl.2014.0629.
Heidemann C, Scheidt-Nave C. Prevalence, incidence and mortality of diabetes mellitus in adults in germany – a review in the framework of the diabetes surveillance. Robert Koch-Institut, Epidemiologie Und Gesundheitsberichterstattung. 2017;2.
Des Jarlais Dc, Lyles C, Crepaz N. Improving the reporting quality of nonrandomized evaluations of behavioral and public health interventions: the trend statement. Am J Public Health. 2004;94(3):361–366. https://doi.org/10.2105/Ajph.94.3.361
Craig P, Cooper C, Gunnell D, et al. Using natural experiments to evaluate population health interventions: new medical research council guidance. J Epidemiol Community Health. 2012;66(12):1182–6. https://doi.org/10.1136/Jech-2011-200375
Shadish Wr, Cook Td, Campbell Dt. Experimental and quasi-experimental designs for generalized causal inference. Wadsworth Cengage Learning; 2002.
Mcdowell I, Spasoff Ra, Kristjansson B. On the classification of population health measurements. Am J Public Health. 2004;94(3):388–393. https://doi.org/10.2105/Ajph.94.3.388
Böhme C, Reimann B. Integrierte Strategien Kommunaler Gesundheitsförderung. Rahmenbedingungen, Steuerung Und Kooperation. Ergebnisse Einer Akteursbefragung. 2018.
Landesgesundheitsamt Baden-Württemberg. Handbuch Zur Kommunalen Gesundheitsförderung: Städte Und Gemeinden Gesundheitsförderlich, Lebenswert Und Generationenfreundlich Gestalten; 2015.
Richter-Kornweitz A, Utermark K. Werkbuch Präventionskette. Herausforderungen Und Chancen Beim Aufbau Von Präventionsketten In Kommunen. Bundeszentrale Für Gesundheitliche Aufklärung; 2013.
Allison Pd. Fixed Effects Models For Count Data.
Hayes Af, Cai L. Using heteroskedasticity-consistent standard error estimators in ols regression: an introduction and software implementation. Behavior Research Methods. 2007;39(4):709–722. https://doi.org/10.3758/Bf03192961
Brüderl J. Kausalanalyse Mit Paneldaten. In: Wolf C, Best H, editors. Handbuch Der Sozialwissenschaftlichen Datenanalyse. Vs Verlag Für Sozialwissenschaften; 2010. p. 963–94.
Rothman Kj, Greenland S, Lash Tl. Modern Epidemiology. 3rd Edition. Lippincott Williams & Wilkens.
Ackermann Rt, Kenrik Duru O, Albu Jb, et al. Evaluating diabetes health policies using natural experiments: the natural experiments for translation in diabetes study. Am J Prev Med. 2015;48(6):747–754. https://doi.org/10.1016/J.Amepre.2014.12.010
Barr B, Bambra C, Whitehead M. The impact of Nhs resource allocation policy on health inequalities in England 2001–11: longitudinal ecological study. BMJ. 2014;348:G3231. https://doi.org/10.1136/Bmj.G3231
Nery Js, Rodrigues Lc, Rasella D, Et Al. Effect Of Brazil's conditional cash transfer programme on tuberculosis incidence. Int J Tuberc Lung Dis. 2017;21(7):790–796. https://doi.org/10.5588/Ijtld.16.0599
Souza Ra De, Nery Js, Rasella D, Et Al. Family health and conditional cash transfer in Brazil and its effect on tuberculosis mortality. Int J Tuberc Lung Dis. 2018;22(11):1300–1306. https://doi.org/10.5588/Ijtld.17.0907
Johansson P, Ostenson C-G, Hilding Am, Andersson C, Rehnberg C, Tillgren P. A cost-effectiveness analysis of a community-based diabetes prevention program In Sweden. Int J Technol Assess Health Care. 2009;25(3):350–358. https://doi.org/10.1017/S0266462309990079
Os M-G, Is M-R. Mortalidad Por Diabetes Tipo 2 Y La Implementación Del Programa Prevenimss: un Estudio De Series De Tiempo En México, 1998–2015. Cad Saude Publica. 2018;34(5):E00103117. https://doi.org/10.1590/0102-311x00103117.
German Cooperation Network ‘Equity In Health’. Criteria For Good Practice In Health Promotion Addressing Social Determinants; 2017. Accessed September 6, 2021. https://www.Gesundheitliche-Chancengleichheit.De/Pdf.Php?Id=Cf95285a65198a1f4d638f5434ea0c19.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics Approval
This study does not require ethical approval as it is based solely on open data. No human participants or animals are involved in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Röding, D., Walter, U. & Dreier, M. Long-Term Effects of Integrated Strategies of Community Health Promotion on Diabetes Mellitus Mortality: a Natural Policy Experiment Based on Aggregated Longitudinal Secondary Data. J Urban Health 98, 791–800 (2021). https://doi.org/10.1007/s11524-021-00590-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-021-00590-7