Abstract
The negative impact of extreme temperatures on health is well-established. Individual help-seeking behavior, however, may mitigate the extent of morbidity and mortality during elevated temperatures. This study examines individual help-seeking behavior during periods of elevated temperatures among a Chinese population. Help-seeking patterns and factors that influence behavior will be identified so that vulnerable subgroups may be targeted for health protection during heat crises. A retrospective time-series Poisson generalized additive model analysis, using meteorological data of Hong Kong Observatory and routine emergency help call data from The Hong Kong Senior Citizen Home Safety Association during warm seasons (June–September) 1998–2007, was conducted. A “U”-shaped association was found between daily emergency calls and daily temperature. About 49% of calls were for explicit health-related reasons including dizziness, shortness of breath, and general pain. The associate with maximum temperature was statistically significant (p = 0.034) with the threshold temperature at which the frequency of health-related calls started to increase being around 30–32°C. Mean daily relative humidity (RH) also had a significant U-shaped association with daily emergency health-related calls with call frequency beginning to increase with RH greater than 70–74% (10–25% of the RH distribution). Call frequency among females appeared to be more sensitive to high temperatures, with a threshold between 28.5°C and 30.5°C while calls among males were more sensitive to cold temperatures (threshold 31.5–33.5°C). Results indicate differences in community help-seeking behavior at elevated temperatures. Potential programs or community outreach services might be developed to protect vulnerable subgroups from the adverse impact of elevated temperatures.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The adverse effect of extreme temperatures on human health has been well documented.1–7 The Intergovernmental Panel on Climate Change predicts that global climate change through changing weather patterns will result in the increased risk of heat-related morbidity and mortality around the world.8 The sensitivity of populations to temperature extremes, however, varies widely between different demographic groups. The elderly are at greatest risk of increased morbidity and mortality during heat waves.9–14
A recent study in Hong Kong indicated that an average 1°C increase in daily mean temperature above 28.2°C was associated with an estimated cumulative 1.5% increase in mortality over the same day and subsequent week.15 Subgroup analyses showed mortality of those who were aged over 75 years, women, unmarried, or living in densely populated areas such as Kowloon and those with unknown residence appeared to be more sensitive to high temperature effects. This suggests that there are potential public health strategies which could protect populations from the adverse health impact of elevated temperatures. On the other hand, to develop appropriate heat wave prevention plans, it is important to understand the relationship between help-seeking behavior and climate-related thresholds among population subgroups. This study examines individual help-seeking behavior during elevated temperatures and heat wave episodes in a Chinese population. Results aim to characterize and identify vulnerable population subgroups that may need special support to protect their well-being.
Methods
A retrospective time-series Poisson generalized additive model analysis, using meteorological data of Hong Kong Observatory (HKO) and routine emergency help call data from The Hong Kong Senior Citizen Home Safety Association (SCHSA) during warm seasons (June–September) 1998–2007, was conducted. Daily weather variables including mean, maximum, and minimum temperatures; dew point temperatures; and mean humidity were obtained from the HKO. Pollution data were obtained from the 11 general environmental collection stations of the Hong Kong Environmental Protection Department. Daily means were calculated from hourly concentrations of nitrogen dioxide (NO2), sulfur dioxide (SO2), ozone (O3), and PM10 which is also known as respirable suspended particulates (RSP) in Hong Kong.16 Average weekly consultation rates of influenza-like illnesses reported by general outpatient clinics and practitioners were obtained from the Centre for Health Promotion to use as a proxy indicator to control for the influence of influenza epidemics on mortality.
Emergency call data were obtained from SCHSA of Hong Kong. SCHSA, a non-profit charitable organization, provides the “Personal Emergency Link” (“PE Link”) Service to elderly citizens living alone and people in need. Although mostly for older population, the PE Link Service is open to applicants of all ages, home districts, and living environments with a residential telephone line. The 24-hour emergency hotline offers support to the emergency needs of callers and provides the necessary support services through referrals. In the event of an emergency, operators might (1) call the police or ambulance center for medical assistance; (2) call the emergency contact person to report the latest status of the user, including hospitalization details; or (3) fax the medical history to the Accident & Emergency Department as to facilitate rescue and medical care. If there is no response from the caller within 2 minutes of pressing the button, the center will treat the case as in an emergency and send for the Fire Service to undertake rescues accordingly. Within the study period, 48,261 members were enrolled in SCHSA. Over two-thirds of callers became SCHSA members with the assistance of organizations such as Social Services, the Housing Department, or SCHSA charity, while the remaining paid on their own.
Poisson generalized additive models were used to model the association between the number of daily calls and daily temperature. Emergency calls (based on daily first-time call) were used as a proxy measurement for help-seeking behavior. Effect modification of the temperature–call frequency association was assessed by subgroup analysis by several demographic variables.
Area of residence was grouped into three variables and used as a proxy indicator to examine the impact of living area characteristics: (1) Kowloon—old district, densely populated, and low-income; (2) Hong Kong—newer district, less densely populated, and middle-to-high-income; and (3) New Territories—newest district, with urban planning, younger population, migrants, and young families. Binary variables were created from socioeconomic status (whether or not recipient of Comprehensive Social Security Assistance (CSSA) scheme), dependency status (living alone versus not living alone), and access to a social network (member of SCHSA versus member of another organization). Specifically, with regard to socioeconomic status, Hong Kong government’s CSSA scheme provides supplemental income to people who living below the poverty line in Hong Kong, and thus, CSSA status represents poverty or low socioeconomic status. Access to social support was defined in this study as access to a community network or services (e.g., whether SCHSA membership was obtained through government referral, through a charitable organization, etc.). Statistical analyses were stratified into demographic subgroups including age, gender, area of residence, reason for calling, socioeconomic status, dependency status, and access to social network.
Models were developed with smooth terms with 4° of freedom each for weather variables including temperature, precipitation(rainfall), and relative humidity (RH). Daily maximum, mean, and minimum temperature variables were tried in the models separately to determine which of the three was most strongly associated with daily health-related calls. Daily variation in temperature = maximum temperature − minimum temperature, change in temperature from the previous day’s daily mean RH, rainfall, and lag terms for temperature up to 7 days were also considered. The models also controlled for seasonality and long-term trends using a smooth function of time, SO2 levels, and duration of heat waves and indicator variables for day of week and public holidays. A “heat wave duration” variable was created based on the number of consecutive days in which the daily mean, maximum, and minimum temperature exceeded the threshold: (a) mean temperature > 28.2°C, (b) minimum temperature > 25.5°C, and (c) maximum temperature > 31.5°C. The smooth terms allowed for the modeling of non-linear associations between temperature and number of calls as well as for non-linear associations, characteristic of seasonality and sometimes present in long-term time trends. Temperature thresholds above which and below which call frequency began to increase were estimated graphically through visual inspection of plots of the adjusted associations between call frequency and maximum temperature from the generalized additive models.
Results
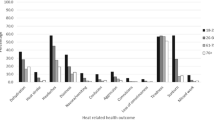
Daily mean temperature over the study days had a mean of 28.4°C, a median of 28.6°C, a range from 22.2°C to 31.8°C and an inter-quartile range (IQR) from 27.3°C to 29.5°C. Only 5 days in the series had a mean temperature below 24°C while 6 days had a mean temperature above 31°C. The mean, median, range, and IQR for maximum daily temperature were 30.6°C, 30.8°C, 23.5–35.4°C, and 29.4–32.1°C, respectively. During the warm seasons between 1998 and 2007, 19,865 SCHSA members made emergency calls to the PE Link, 10,916 of which were for explicitly health-related reasons. Table 1 shows the demographic profile of callers. About 49% of calls were for explicit health-related reasons including dizziness, shortness of breath, and general pain. The remaining gave either “other” or “no reason” for calling. Health-related callers were mostly over 75 years of age (68%), and living in Kowloon and New Territories (Hong Kong = 15%, Kowloon = 44%, New Territories = 40%). About 44% of callers were on the Hong Kong government’s CSSA scheme and 50% were living alone. Of note, while there were new members and potential drop-outs (due to death and termination of usage, etc.) of the hotline call scheme, the overall member enrollment was relatively constant during the study period.
Females, people under 75 years old, those living alone, and Hong Kong Island and New Territories residents had lower thresholds at which high-temperature effects on calls began to be seen (Table 1 and Figures 1, 2, 3, 4, 5, 6, and 7). Heat wave durations and daily rainfall were not significantly associated with health-related calls and were dropped from the models. Maximum temperature was a stronger predictor of daily health-related calls than mean or minimum temperature (both of which were non-significant were examined independently) so maximum temperature was chosen for all subsequent modeling. Lagged effects of maximum temperature, diurnal temperature variation, and changes in temperature from the previous day were also not significant and were dropped from the models.
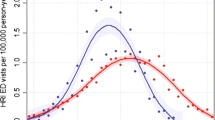
All health-related calls (p values: maximum air temperature p = 0.034, mean relative humidity p = 0.011, SO2 p = 0.046. During the warm seasons between 1998 and 2007, 19,865 SCHSA members made emergency calls to the PE Link, of which 10,916 were for explicitly health-related reasons). Associations between weather and SO2 and daily numbers of health-related calls. Y-axis represents the centered standardized residuals when controlling for other variables in the model. Solid line represents the smoothed mean residuals across values of the X-axis variables which describes the basic shape of the association. Dashed lines represent 95% Bayesian credible intervals.
Figures 1, 2, 3, 4, 5, 6, and 7 illustrate the association between daily calls for health-related reasons and mean temperature by subgroups. Results indicate that daily calls had a “U”-shaped association with daily maximum temperature (p = 0.034) and a ∩-shaped relationship with mean RH (p = 0.011; Figure 1). For maximum daily temperature, the threshold at which frequency of calls began to increase was about 30–32°C. For mean RH, the frequency of calls peaked between 74% and 78% and decreased for RH% above and below these values (Figure 1). Since 77% was at the 25th percentile of the RH distribution, an inverse association between RH and call frequency existed over most of the range of RH observed in the data. There was also a U-shaped association between mean daily temperature and frequency of calls with a temperature threshold at which calls increased of 27–29°C. Subgroup analyses of the association between maximum temperature and the frequency of health-related calls indicated that females (Figure 3), those 75 years of age or older, and Hong Kong Island residents (Figure 4) appeared more sensitive to high maximum temperatures, while males and Kowloon residents appeared more sensitive to lower maximum temperatures, i.e., “cool effects.” Figure 8 shows the overall association between daily maximum temperature and daily health-related calls, not adjusting for seasonality or other confounders.
Discussion
Results indicate that during the warm seasons in Hong Kong, the volume of help-seeking calls at higher temperatures varies among demographic subgroups. Overall, the threshold temperature for making calls has a U-shaped distribution. Our findings are comparable to a recent temperature-related mortality study in Hong Kong which found that during the warm seasons, 28.2°C was the critical threshold temperature for elevated mortality (May–October, 1998–2006).15
Age and Gender Effect
While the effect of extreme temperature was particularly noticeable among older age groups and females,13 , 17 few studies have examined the temperature threshold differences between demographic subgroups. A study that compared the differences in six major cities in South Korea found that threshold temperatures for mortality varied between 27.0°C and 29.7°C.18 The elderly were found to be especially vulnerable with lower threshold temperatures for mortality ranging from 24.5°C to 28.5°C.
Geography and the Issue with “Cool Temperature Effects”
Our findings show that help-seeking behavior was more sensitive to elevated temperatures for women, those over 75 years of age, and people living in a wealthier part of Hong Kong (e.g., Hong Kong Island). Of note, while call volume was the highest overall in Kowloon, the most densely populated area of Hong Kong, the threshold temperature was also the highest compared to other areas. Thus, Kowloon residents were less likely to show an increase in help-seeking behavior until temperatures were higher and also were more sensitive to “cool temperature” effects. Although this may be explained by physiological adaptation, it may also be influenced by lack of knowledge (e.g., lower awareness of the potential adverse health implications and consequent failure to seek help during high temperatures) and behavioral practices (delay or refuse to seek care). Future study would need to explore the underlying drivers and motivations of health and help-seeking behavior in extreme temperature by different population subgroups.
Temperature Variability
A study in Shanghai revealed that temperature variability may play an important role in heat-related health impact.19 In Shanghai, mortality was strongly associated with the diurnal temperature range (DTR), or within-day variation in temperature.19 The study population included 6.3 million residents between 2001 and 2004 in suburban and urban areas of Shanghai. The DTR was found to be positively associated with mortality, particularly among those aged over 45 years. In the USA, higher risk of death was observed during summertime for cities with greater temperature variances.20 In Valencia, Spain, mortality increased in proportion to the range of temperatures varying between winters and summers.21
Our results indicate that help-seeking behavior related to health-related reasons are sensitive to temperature. Morbidity studies also show that hospital admissions rise with increased ambient temperature.12 , 22 Policy makers may wish to consider plans incorporating temperature sensitivity and help-seeking behavior to reduce hospital admissions during extreme temperatures.
Although this study is one of few studies that have examined help-seeking behavior during extreme temperatures, there are methodological limitations due to the study’s retrospective nature. In addition, only first-time calls made by members were used. Results may be biased toward the SCHSA population who are generally older and female, and the lack of information regarding the air conditioner ownership within our study population might also lead to potential biasness findings toward expressed help need during extreme temperature. Another potential limitation to this study is that the most vulnerable subgroups may have been excluded as the PE Link emergency bell requires a telephone land line.
Conclusion
While the threshold for mortality was found to be consistent among population subgroups,15 results indicate differences in community help-seeking behavior in times of crisis during elevated temperature. There is currently a limited understanding of the effectiveness of population response to public warning of heat, especially in the high-risk populations in urban Chinese communities. Policy makers and community outreach services should consider targeting more vulnerable subgroups to protect them from adverse human health impact from elevated temperature.
What This Paper Adds
What is already known on this subject:
-
There are intra-city differences in the association between temperature and mortality in urban areas.
-
It is uncertain if the temperature thresholds of individual help-seeking behavior correlate to the temperature–mortality pattern.
-
Limited studies were found to examine predictors of individual help-seeking behavior during elevated temperature.
What this study adds:
-
Daily emergency calls exhibited a “U”-shaped association with temperature.
-
Study results indicate differences in individual help-seeking behavior at elevated temperatures.
-
Potential programs or community outreach services might be developed to target vulnerable subgroups to protect them from the adverse impact of elevated temperatures.
References
Pirard P, Vandentorren S, Pascal M, et al. Summary of the mortality impact assessment of the 2003 heat wave in France. Euro Surveill. 2005; 10(7): 15.
Davis RE, Knappenberger PC, Michaels PJ, et al. Changing heat-related mortality in the United States. Environ Health Perspect. 2003; 111(14): 1712–1718.
Hajat S, Kovats RS, Atkinson RW, Haines A. Impact of hot temperatures on death in London: a time series approach. J Epidemiol Community Health. 2002; 56(5): 367–372.
Braga AL, Zanobetti A, Schwartz J. The time course of weather-related deaths. Epidemiology. 2001; 12(6): 662–667.
Grize L, Huss A, Thommen O, et al. Heat wave 2003 and mortality in Switzerland. Swiss Med Wkly. 2005; 135(13–14): 200–205.
Michelozzi P, de Donato F, Bisanti L, et al. The impact of the summer 2003 heat waves on mortality in four Italian cities. Euro Surveill. 2005; 10(7): 161–165.
Curriero FC, Heiner KS, Samet JM, et al. Temperature and mortality in 11 cities of the eastern United States. Am J Epidemiol. 2002; 155(1): 80–87.
Intergovernmental Panel on Climate Change. IPCC fourth assessment report: climate change 2007. http://www.ipcc.ch/ipccreports/ar4-wg2.htm. Published 2007. Accessed June 22, 2008.
Fouillet A, Rey G, Laurent F, et al. Excess mortality related to the August 2003 heat wave in France. Int Arch Occup Environ Health. 2006; 80(1): 16–24.
Huynen MM, Martens P, Schram D, et al. The impact of heat waves and cold spells on mortality rates in the Dutch population. Environ Health Perspect. 2001; 109(5): 463–470.
Hutter HP, Moshammer H, Wallner P, et al. Heatwaves in Vienna: effects on mortality. Wien Klin Wochenschr. 2007; 119(7–8): 223–227.
Kovats RS, Hajat S, Wilkinson P. Contrasting patterns of mortality and hospital admissions during hot weather and heat waves in Greater London, UK. Occup Environ Med. 2004; 61(11): 893–898.
Johnson H, Kovats RS, McGregor G, et al. The impact of the 2003 heat wave on mortality and hospital admissions in England. Health Stat Q. 2005; 25: 6–11.
Abrahamson V, Wolf J, Lorenzoni I, et al. Perceptions of heatwave risks to health: interview-based study of older people in London and Norwich, UK. J Public Health Med. 2009; 31: 119–126.
Chan EYY, Goggins WB, Kim JJ, Griffiths S. A study of intracity variation of temperature related mortality and socioeconomic status among Chinese population in Hong Kong. J Epidemiol Community Health. 2010. doi:10.1136/jech.2008.085167.
Environmental Protection Department, The Government of the Hong Kong Special Administrative Region. Definition for respirable suspended particles (RSP). www.epd.gov.hk/epd/english/environmentinhk/air/data/emission_inve_rsp.html. Accessed May 1, 2009.
Nitschke M, Tucker GR, Bi P. Morbidity and mortality during heatwaves in metropolitan Adelaide. Med J Aust. 2007; 187: 11–12.
Kim H, Ha JS, Park J. High temperature, heat index, and mortality in 6 major cities in South Korea. Arch Environ Occup Health. 2006; 61(6): 265.
Tan J, Zheng Y, Song G, et al. Heat wave impacts on mortality in Shanghai, 1998 and 2003. Int J Biometeorol. 2007; 51(3): 193–200.
Braga AL, Zanobetti A, Schwartz J. The effect of weather on respiratory and cardiovascular deaths in 12 U.S. cities. Environ Health Perspect. 2002; 110(9): 859–863.
Ballester F, Corella D, Pérez-Hoyos S, Sáez M, Hervás A. Mortality as a function of temperature. A study in Valencia, Spain, 1991–1993. Int J Epidemiol. 1997; 26(3): 551–561.
Tai CC, Lee CC, Shih CL, Chen SC. Effects of ambient temperature on volume, specialty composition and triage levels of emergency department visits. Emerg Med J. 2007; 24(9): 641–644.
Acknowledgments
This study is supported by the Chinese University of Hong Kong School of Public Health Research Grant. The study sponsor was not involved in the study design or the collection, analysis or interpretation of data, writing of the article, or decision to submit it for publication.
Ethics Approval
Ethics approval was not required for the study.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Chan, E.Y.Y., Goggins, W.B., Kim, J.J. et al. Help-Seeking Behavior during Elevated Temperature in Chinese Population. J Urban Health 88, 637–650 (2011). https://doi.org/10.1007/s11524-011-9599-9
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11524-011-9599-9