Abstract
Background
The prognosis of patients with advanced gastrointestinal stromal tumor (GIST) has improved greatly after the introduction of imatinib. However, primary or secondary resistance to imatinib occurs in the majority of patients. Sunitinib is the standard second line treatment in exon-9 mutated GIST.
Objective
We compared the clinical outcomes of sunitinib with imatinib dose escalation in patients with progressive advanced non-KIT exon 9 mutated GIST after failure of first line imatinib.
Patients and Methods
A retrospective study was performed, retrieving data from a real-life database (Dutch GIST Registry) including patients with GIST treated with sunitinib or imatinib dose escalation after failure on first line imatinib 400 mg daily. Primary outcome measures were progression free survival (PFS) and overall survival (OS).
Results
In total, 110 patients were included, 72 (65.5%) patients were treated with sunitinib (group A) and 38 (34.5%) received an imatinib dose escalation (group B). Important prognostic features at baseline, such as tumor size, stage at diagnosis, mitotic count and localization were equally distributed in both groups. No significant difference (p = 0.88) between median PFS in group A [8.7 months (95% CI 5.6–11.3)] and group B [5.6 months, (95% CI 2.6–8.7)] was observed. Moreover, the OS was similar between group A and group B; 63.2 months and 63.4 months, respectively.
Conclusion
This study represents a proper sample size cohort containing detailed data on mutational status of patients with advanced GIST. We illustrated that imatinib dose escalation could serve as a good alternative for sunitinib as second-line treatment in patients with a non-KIT exon 9 mutation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Imatinib 400 mg daily is firmly established first-line therapy for advanced GIST. |
Second-line treatment with imatinib dose escalation resulted in similar PFS and OS compared to sunitinib (the standard second-line therapy). |
Imatinib dose escalation is an alternative strategy as second-line treatment of advanced GIST. |
1 Introduction
Gastrointestinal stromal tumors (GISTs) are rare tumors accounting for less than 1% of gastrointestinal malignancies. Nevertheless, GISTs represent the most common type of sarcoma, with an incidence of 15 patients per million per year [1]. Primary GIST occurs most frequently in the stomach (56%) and small intestines (32%), while localization of GIST in colon (6%), rectum (1%), esophagus (< 1%) and other sites (4%) is rare [2]. Approximately 80% of GISTs are a result of oncogenic mutations in KIT receptor and 10–15% of patients exhibit mutations in platelet-derived growth factor receptor (PDGFR) genes [3, 4]. In the remaining 10%–15% of GIST (formerly labeled as wild-type GIST) NF1, NTRK and BRAF-mutations and mutations leading to succinate dehydrogenase (SDH)-deficiency, are identified [5,6,7].
Localized GIST is treated with complete surgical resection and, depending on risk assessment, adjuvant therapy is indicated [8]. For patients with locally advanced (unresectable) GIST or metastasized GIST, imatinib is the treatment of choice [9, 10]. While imatinib 400 mg daily is the standard dose, the MetaGIST study illustrated that imatinib dose of 800 mg daily is more effective in patients with a KIT exon 9 mutation and is therefore the recommend dose in this type of mutation [11].
When treatment with imatinib fails, sunitinib is the standard second-line therapy [12]. However, the European Society for Medical Oncology (ESMO) guidelines suggest that high-dose imatinib (800 mg daily) may be an option in patients with progression on first-line imatinib [8]. It is unclear whether imatinib dose escalation or sunitinib should be preferred in case of disease progression on imatinib 400 mg, as they have not been compared head-to-head in a prospective study. Prospectively collected real-life data, such as the Dutch GIST Registry, are then the next best method to evaluate this. In the current study, we compared the efficacy of sunitinib with imatinib dose escalation after failure on first-line imatinib in patients with advanced GIST.
2 Methods
2.1 Patients and Study Design
A retrospective, multicenter study was conducted, which included patients with histologically proven GIST diagnosed between January 2009 and July 2020. Data were retrieved from the Dutch GIST Registry (DGR), which contains data of all GIST patients treated in five GIST specialized centers in the Netherlands since January 2009. These centers include the Netherlands Cancer Institute, Leiden University Medical Center, Erasmus MC Rotterdam, Radboudumc, and UMC Groningen. The inclusion criteria were aged ≥ 18 years and RECIST 1.1 [13] progressive GIST on first-line imatinib at a dose of 400 mg/day, and (for the imatinib dose escalation group) imatinib dose escalation for reason of disease progression. Patients with dose escalation for reasons of therapeutic drug monitoring (personalized dosing based on imatinib drug concentrations in the blood) were excluded. Other exclusion criteria were KIT exon 9 or unknown mutational status, ongoing first-line imatinib and absence of second-line treatment. Furthermore, patients treated with an agent other than imatinib as first-line therapy were excluded. The local Medical Ethics Review Committee of LUMC confirmed that the Medical Research Involving Human Subjects Act did not apply for this study (registration no. G20.003).
2.2 Variables of Interest
Demographic data and clinicopathological features including localization, tumor size, stage at diagnosis, mitotic count and mutational status were collected. The mitotic count was specified as number of mitotic figures per 50 High Power Fields (HPF) or 5 mm2, which was considered as equivalent.
2.3 Outcomes
Our main focus was on patients with a non-KIT exon 9 mutation. The primary outcomes were progression-free and overall survival (PFS and OS) of imatinib dose escalation versus sunitinib after failure of first-line imatinib. The secondary outcome was the duration of sunitinib treatment in the direct second-line cohort (group A) compared to duration of sunitinib treatment following imatinib dose escalation (group B).
2.4 Statistical Analysis
The median follow-up was calculated from date of diagnosis to date of last follow-up or death. Progression-free survival second-line therapy was determined from date of start of imatinib dose escalation or sunitinib to date of progression or death. To estimate survival, the Kaplan Meier method was performed and the groups were compared by log-rank test. The Mann–Whitney U test was used to compare time (interval) to sunitinib failure. Categorical variables were analyzed using χ2 test. The IBM SPSS Statistics 25 was used to perform the statistical analysis. A p value of < 0.05 was labeled as significant.
3 Results
3.1 Patient Characteristics
In the DGR, 463 patients with advanced GIST were treated with first-line imatinib in a palliative setting. After excluding patients with ongoing first-line imatinib, patients with no further treatment after first-line treatment and patients with a KIT exon 9 mutation or unknown mutational status, 118 patients were eligible. Of the 118 patients who started with imatinib 400 mg, 8 patients stopped imatinib due to intolerance and were therefore excluded from further analysis (Fig. 1). In the remaining 110 patients, reason to stop imatinib 400 mg was progressive disease. After failure of imatinib 400 mg, 72 (65.5%) patients were treated with sunitinib (group A) and 38 (34.5%) received imatinib 800 mg as second-line treatment (group B: imatinib dose escalation). In group A, 42 patients (58.3%) were treated with sunitinib in a continuous dosing schedule (37.5 mg daily) and 30 patients (41.7%) received an intermittent dosing schedule (4 weeks on, 2 weeks off) with a daily dose of 50 mg. Reason for failure of sunitinib (n = 59) was due to progressive disease in 46 (78.0%) patients and toxicity in 13 (22.0%) patients. Numbers of patients who started with third-line treatment, numbers of patients with ongoing treatment of second- and third-line treatment and number of patients with no further treatment after ending second- and third-line treatment are specified in Fig. 1.
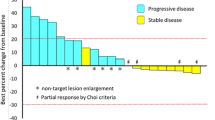
3.2 Duration of First-Line Therapy and PFS of Second-Line Treatment
The demographic and clinicopathological features are listed in Table 1. There was no significant difference between group A and group B in localized or metastasized GIST at diagnosis, localization of primary tumor, mitotic count, or mutational status. Furthermore, no significant difference was observed in the duration of first-line imatinib. The median duration of first-line imatinib was 18.6 months (01.2–94.3) in group A and 16.3 months (range 1.1–105.9) in group B. The median follow-up time for patients in group in group A was 46.5 months (range 6.4–127.7 months) and 55.3 months (range 5.3–140.3 months) in group B. During the follow-up period, progression of GIST was observed in 64 (89.9%) patients in group A and in 34 (89.5%) patients in group B. Patients who received sunitinib showed a median PFS of 8.4 months (95% CI 5.6–11.3) and treatment with imatinib dose escalation led to a median PFS of 5.6 months (95% CI 2.6–8.7). There was no significant difference in PFS between both groups (Fig. 2A).
3.3 Overall Survival
In total, death occurred in 65 (59.1%) patients, with progressive GIST as cause of death in 61 patients, toxicity (small bowel perforation) as a consequence of regorafenib use in 1 patient, non-GIST-related cause of death (urosepsis) in 1 patient, and 2 patients had unspecified cause of death. Analyzing overall survival, no significant difference between group A and B was observed. Patients with imatinib dose escalation had a median OS of 63.2 months (95I CI 47.6–78.9) and a median OS of 63.4 months (95% CI 50.4–76.3) was observed in sunitinib group (Fig. 2B).
After progression on imatinib dose escalation, 27 patients proceeded to next-line treatment with sunitinib. These patients had a median time to sunitinib failure of 8.2 months (range 1.3–24.7).
4 Discussion
The discovery of KIT and PDGFRA receptor tyrosine kinase inhibitors (TKIs) allowed GIST to become a model for molecular-targeted therapy. Introduction of imatinib radically improved the prognosis of patients with inoperable and metastatic GIST, leading to a median PFS of approximately 2 years, with nearly 10% of patients having progression-free disease at 10 years after start of treatment [13].
However, in most GIST patients, resistance to imatinib (e.g., due to secondary mutations) eventually occurs. Sunitinib is the approved second-line treatment resulting in PFS of circa 6 months after failure on imatinib [12]. However, high-dose imatinib (800 mg daily) has also shown its beneficial clinical outcomes (median PFS 20–25 months) in patients with progressive disease on imatinib 400 mg [9, 10]. It is under debate, which treatment (imatinib dose escalation or sunitinib) is preferred as second-line therapy. Because high-dose (800 mg) imatinib is the standard recommended dose for KIT exon 9 mutation [8] excluding dose escalation as an option as a second-line therapy, we excluded patients with the aforementioned mutation.
In the current study, we observed that in patients with a non-KIT exon 9 mutation, treatment with imatinib dose escalation as second-line therapy led to similar clinical outcomes as sunitinib. The median PFS of imatinib dose escalation was not significantly different compared to sunitinib. Additionally, OS was equal between patients who received imatinib dose escalation and patients treated with sunitinib. A substantial difference (i.e., inferiority) in efficacy of imatinib dose escalation compared to sunitinib, might be expected due to firm position of sunitinib as second-line therapy, but our observation does not support this. As shown in Table 1, important prognostic factors, such as stage at diagnosis, tumor size, localization of GIST, and mitotic count were equally distributed in patients receiving imatinib dose escalation and patients treated with sunitinib. Furthermore, median duration of first-line imatinib was similar in both groups. Therefore an overrepresentation of patients with low-risk or indolent GIST in the group treated with imatinib dose escalation is unlikely.
Studying the role of therapeutic drug monitoring (TDM) in previous studies showed that most patients treated with a fixed dose imatinib had a serum imatinib concentration below the efficacy threshold [14], which may affect time to progression. However, post hoc analysis in our study showed that TDM was performed in 53% of patients, demonstrating generally adequate imatinib concentrations.
A number of patients in our study had primary mutations that are generally resistant to imatinib, in particular patients with PDGFRA exon 18-D842V mutation. Due to lack of alternative therapy at time of diagnosis, these patients were treated with imatinib. Nowadays, avapritinib, a novel agent, has been developed to treat patients with a D842V mutation [15]. However, for other primary imatinib-resistant mutations (e.g., SDH-deficient GIST) an effective therapy is not yet established.
For some secondary KIT mutations leading to imatinib-resistance in GIST [16, 17], sunitinib is more effective due to different and broader binding characteristics and affinities [18]. Treatment of GIST would benefit from mutational analysis at time of progression. Identification of secondary mutation resistant to imatinib and sensitive to sunitinib, makes a decision to initiate sunitinib more reasonable than imatinib dose escalation.
Beside the efficacy, the safety profile, and adverse events of imatinib dose escalation and sunitinib should be weighed before choosing the second-line treatment after failure of imatinib 400 mg. While hematological toxic adverse effects of imatinib and sunitinib are common, patients treated with sunitinib generally experience more leukopenia, neutropenia, and thrombocytopenia than patients receiving imatinib. In addition, the most common non-hematological adverse events of (high-dose) imatinib are edema, fatigue, and nausea, whereas hand-foot syndrome, diarrhea and hypertension are more frequently observed in patients receiving sunitinib [8, 9].
There are no randomized prospective trials comparing imatinib dose escalation to sunitinib as second-line treatment. Previously published studies are either single-center based with small sample size [19] or lack data on important factors such as mutational status [20]. The most important limitation of the current study is the retrospective design making randomized treatment allocation impossible, which may have led to selection bias. Moreover, data on quality-of-life parameters and (patient)-reported side effects were not included. When available, these parameters can contribute to shared decision-making in choosing imatinib dose escalation or sunitinib as treatment after failure of first-line imatinib. Furthermore, prognostic factors (e.g., sites of metastases, tumor burden) for metastatic GIST, which are different than for primary GIST, were not consistently available and therefore not included in this study. The strength of our study is detailed data on mutational status, tumor size, mitotic count, and localization of primary tumor. Furthermore, the Dutch GIST Registry represents a unique real-life database including clinicopathological data on patients treated in Dutch sarcoma specialized centers, allowing to study GIST patients more specifically.
In conclusion, this study demonstrates that in patient with advanced GIST harboring a non-KIT exon 9 mutation, imatinib dose escalation could serve as a proper alternative second-line strategy for sunitinib, after failure on imatinib 400 mg.
References
Verschoor AJ, Bovee J, Overbeek LIH, Hogendoorn PCW, Gelderblom H. The incidence, mutational status, risk classification and referral pattern of gastro-intestinal stromal tumours in the Netherlands: a nationwide pathology registry (PALGA) study. Virchows Arch. 2018;472(2):221–9.
Soreide K, Sandvik OM, Soreide JA, Giljaca V, Jureckova A, Bulusu VR. Global epidemiology of gastrointestinal stromal tumours (GIST): a systematic review of population-based cohort studies. Cancer Epidemiol. 2016;40:39–46.
Hirota S, Isozaki K, Moriyama Y, Hashimoto K, Nishida T, Ishiguro S, et al. Gain-of-function mutations of c-kit in human gastrointestinal stromal tumors. Science. 1998;279(5350):577–80.
Heinrich MC, Corless CL, Duensing A, McGreevey L, Chen CJ, Joseph N, et al. PDGFRA activating mutations in gastrointestinal stromal tumors. Science. 2003;299(5607):708–10.
Agaimy A, Terracciano LM, Dirnhofer S, Tornillo L, Foerster A, Hartmann A, et al. V600E BRAF mutations are alternative early molecular events in a subset of KIT/PDGFRA wild-type gastrointestinal stromal tumours. J Clin Pathol. 2009;62(7):613–6.
Miettinen M, Wang ZF, Sarlomo-Rikala M, Osuch C, Rutkowski P, Lasota J. Succinate dehydrogenase-deficient GISTs: a clinicopathologic, immunohistochemical, and molecular genetic study of 66 gastric GISTs with predilection to young age. Am J Surg Pathol. 2011;35(11):1712–21.
Miettinen M, Fetsch JE, Sobin LH, Lasota J. Gastrointestinal stromal tumors in patients with neurofibromatosis 1—a clinicopothologic and molecular genetic study of 45 cases. Am J Surg Pathol. 2006;30(1):90–6.
Casali PG, Abecassis N, Bauer S, Biagini R, Bielack S, Bonvalot S, et al. Soft tissue and visceral sarcomas: ESMO-EURACAN clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2018;29:51–67.
Verweij J, Casali PG, Zalcberg J, LeCesne A, Reichardt P, Blay JY, et al. Progression-free survival in gastrointestinal stromal tumours with high-dose imatinib: randomised trial. Lancet. 2004;364(9440):1127–34.
Blanke CD, Rankin C, Demetri GD, Ryan CW, von Mehren M, Benjamin RS, et al. Phase III randomized, intergroup trial assessing imatinib mesylate at two dose levels in patients with unresectable or metastatic gastrointestinal stromal tumors expressing the kit receptor tyrosine kinase: S0033. J Clin Oncol. 2008;26(4):626–32.
Gastrointestinal Stromal Tumor Meta-Analysis G. Comparison of two doses of imatinib for the treatment of unresectable or metastatic gastrointestinal stromal tumors: a meta-analysis of 1,640 patients. J Clin Oncol. 2010;28(7):1247–53.
Demetri GD, van Oosterom AT, Garrett CR, Blackstein ME, Shah MH, Verweij J, et al. Efficacy and safety of sunitinib in patients with advanced gastrointestinal stromal tumour after failure of imatinib: a randomised controlled trial. Lancet. 2006;368(9544):1329–38.
Casali PG, Zalcberg J, Le Cesne A, Reichardt P, Blay JY, Lindner LH, et al. Ten-year progression-free and overall survival in patients with unresectable or metastatic GI stromal tumors: long-term analysis of the European organisation for research and treatment of cancer, Italian sarcoma group, and Australasian gastrointestinal trials group intergroup phase III randomized trial on imatinib at two dose levels. J Clin Oncol. 2017;35(15):1713–20.
NS IJ, Groenland SL, Koenen AM, Kerst M, van der Graaf WTA, Rosing H, et al. Therapeutic drug monitoring of imatinib in patients with gastrointestinal stromal tumours—results from daily clinical practice. Eur J Cancer. 2020;136:140–8.
Heinrich MC, Jones RL, von Mehren M, Schöffski P, Serrano C, Kang YK, et al. Avapritinib in advanced PDGFRA D842V-mutant gastrointestinal stromal tumour (NAVIGATOR): a multicentre, open-label, phase 1 trial. Lancet Oncol. 2020;21(7):935–46.
Antonescu CR, Besmer P, Guo T, Arkun K, Hom G, Koryotowski B, et al. Acquired resistance to imatinib in gastrointestinal stromal tumor occurs through secondary gene mutation. Clin Cancer Res. 2005;11(11):4182–90.
Liegl B, Kepten I, Le C, Zhu M, Demetri GD, Heinrich MC, et al. Heterogeneity of kinase inhibitor resistance mechanisms in GIST. J Pathol. 2008;216(1):64–74.
Gramza AW, Corless CL, Heinrich MC. Resistance to tyrosine kinase inhibitors in gastrointestinal stromal tumors. Clin Cancer Res. 2009;15(24):7510–8.
Yang WL, Li K, Yu JR, Shou CH, Zhang Q, Hong YY, et al. Clinical outcomes of imatinib dose escalation versus sunitinib in first-line imatinib-failure gastrointestinal stromal tumour. Scand J Gastroenterol. 2018;53(10–11):1328–34.
Hsu JT, Le PH, Kuo CF, Chiou MJ, Kuo CJ, Chen TH, et al. Imatinib dose escalation versus sunitinib as a second-line treatment against advanced gastrointestinal stromal tumors: a nationwide population-based cohort study. Oncotarget. 2017;8(41):71128–37.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No external funding was used in the analysis and preparation of this manuscript. An unrestricted research grant for the Dutch GIST Registry to NKI is received from Novartis (3017/13), Pfizer (WI189378), Bayer (2014-MED-12005), and Deciphera (4EE9EEC-7F19-484D-86A4-646CFE0950A5). These funding sources did not have any involvement in conducting this research.
Conflict of interest
Mahmoud Mohammadi, Thekla M. Jansen-Werkhoven , Nikki S. IJzerman, Dide den Hollander, Roos F. Bleckman, Astrid W. Oosten, Ingrid M.E. Desar, An K.L. Reyners, Neeltje Steeghs and Hans Gelderblom declare that they have no conflicts of interest that might be relevant to the contents of this manuscript.
Ethics approval
The local Medical Ethics Review Committee of LUMC confirmed that the Medical Research Involving Human Subjects Act did not apply for this study (registration no. G20.003).
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
Code availability
Not applicable.
Author contributions
MM: Conceptualization, Formal analysis, Writing—Original Draft, Writing—Review & Editing TMJ-W: Software, Investigation NSI: Investigation, Writing—Review & Editing DH: Investigation, Writing—Review & Editing RFB: Investigation, Writing—Review & Editing AWO: Writing—Review & Editing, IMED: Writing—Review & Editing, AKLR: Writing—Review & Editing, NS: Methodology, Writing—Review & Editing HG: Conceptualization, Methodology, Supervision.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Mohammadi, M., Jansen-Werkhoven, T.M., Ijzerman, N.S. et al. Dutch Gastrointestinal Stromal Tumor (GIST) Registry Data Comparing Sunitinib with Imatinib Dose Escalation in Second-Line Advanced Non-KIT Exon 9 Mutated GIST Patients. Targ Oncol 17, 627–634 (2022). https://doi.org/10.1007/s11523-022-00926-6
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-022-00926-6