Abstract
Background
The combination of trifluridine-tipiracil and bevacizumab was compared with trifluridine-tipiracil monotherapy in a randomized, open-label, phase II trial, resulting in a statistically significant and clinically relevant improvement in progression-free survival (PFS), with tolerable toxicity in patients with refractory metastatic colorectal cancer (mCRC); however, evidence supporting the role of this combination in a real-world setting is limited.
Objective
The aim of our work was to provide further evidence on the activity and safety of this combination in a real-world series of Western mCRC patients refractory or intolerant to previous therapies.
Patient and Methods
We conducted a retrospective, observational study of patients with mCRC refractory or intolerant to standard therapies. Patients were treated with trifluridine-tipiracil and bevacizumab. Previous therapy with fluoropyrimidines, irinotecan, oxaliplatin, bevacizumab, aflibercept, regorafenib, and cetuximab or panitumumab (only RAS wild-type) was allowed, as was previous participation in clinical trials. Clinicopathological characteristics, overall response rate (ORR), disease control rate (DCR), overall survival (OS), PFS, and safety data were retrospectively collected and analyzed.
Results
We recorded 31 patients treated between 1 December 2017 and 30 June 2022. Median age was 69 years (range 38–82 years), 39% were male, 100% had an Eastern Cooperative Oncology Group (ECOG) performance status (PS) of 0–1, tumor location was left-sided in 77% of cases, 54% had synchronous presentation, 35% were RAS mutant, 3% were BRAF mutant, and 71% underwent primary tumor resection; 64% of patients had liver metastases, 55% had lung metastases, and 23% had peritoneal carcinomatosis. The median number of previous treatment lines was 2 (range 0–5), and 84% of patients received at least one previous anti-angiogenic agent. The ORR and DCR were 3% and 71%, respectively. With a median follow-up of 8 months (range 2–39), median PFS was 6 months (95% confidence interval [CI] 3.1–8.9 months) and median OS was 14 months (95% CI 10.1–17.8 months). Adverse events of any grade were reported in 58% of patients. The most common grade 3–4 toxicities were neutropenia (19%) and anemia (6%); 35% of patients required either dose delays or dose reductions due to toxicity. Granulocyte colony-stimulating factor (G-CSF) prophylaxis was administered either on first or subsequent cycles of treatment in 35% of patients. No treatment-related deaths occurred. Sixty percent of the patients who discontinued treatment eventually received one or more lines of subsequent therapy.
Conclusions
Our series provides further evidence on the activity and safety of the combination of trifluridine-tipiracil and bevacizumab in a real-world series of Western refractory mCRC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Treatment options for refractory metastatic colorectal cancer are limited. |
The combination of trifluridine-tipiracil and bevacizumab showed promising activity and safety in clinical trials. |
Our series provides further evidence on the efficacy and tolerability of this combination in real-world patients. |
1 Introduction
Colorectal cancer (CRC) is the third most common cancer in males and the second most common in females, with approximately 1.9 million new cases and 0.9 million deaths in 2020 worldwide [1]. In patients diagnosed with CRC, 20% have metastatic disease and 40% of those treated for localized disease eventually develop systemic recurrence [2].
First- and second-line systemic treatment for metastatic CRC (mCRC) usually includes a chemotherapy backbone, formed by fluoropyrimidines, oxaliplatin, and irinotecan-based regimens, paired with a biologic agent [3]. An anti-vascular endothelial growth factor (VEGF) or anti-epidermal growth factor receptor (EGFR) antibody is usually added to the chemotherapy regimen depending on tumor- and patient-related characteristics, such as RAS/BRAF mutational status and tumor sidedness [4]. Immune checkpoint inhibitors (ICIs) were recently added to therapeutic options in mismatch repair-deficient (dMMR)/microsatellite instability-high (MSI-H) mCRC [5].
Patients with mCRC experiencing disease progression despite treatment with chemotherapy and targeted agents have refractory disease [2]. In these patients, treatment is aimed at extending survival without altering quality of life. Both regorafenib and trifluridine-tipiracil have been shown to improve progression-free survival (PFS) and overall survival (OS) when compared with best supportive care in refractory disease [6, 7].
Trifluridine-tipiracil is an orally administered drug constituting an active antitumor component (trifluridine, which competes with thymidine for DNA incorporation) and a thymidine phosphorylase inhibitor (tipiracil, which increases the bioavailability of the drug) [8]. Despite being effective across different patient subgroups and presenting a manageable safety profile [9, 10], trifluridine-tipiracil monotherapy provides limited survival benefit.
With the aim of improving its activity, several authors have tried combining trifluridine-tipiracil with the anti-VEGF antibody bevacizumab. Bevacizumab is a recombinant, humanized, monoclonal antibody that inhibits angiogenesis and predominantly acts by controlling blood vessel formation and modulating tumor-induced immunosuppression [11].
A phase I/II study (C-TASK FORCE) evaluated the combination of trifluridine-tipiracil and bevacizumab in refractory mCRC and showed promising antitumor activity with manageable toxicity [12]. These results led to the design of two different randomized phase II trials to further investigate the activity of the combination. A first trial (TASCO1) compared the combination of trifluridine-tipiracil and bevacizumab with a combination of capecitabine and bevacizumab in chemotherapy-naïve patients not amenable for intensive oxaliplatin- or irinotecan-based chemotherapy [13]. The trifluridine-tipiracil-based combination showed promising activity and tolerable toxicity, a performance consistent with results from the homologous phase III trial recently presented during a European Society of Medical Oncology (ESMO) Virtual Plenary [14]. A second trial compared the combination of trifluridine-tipiracil and bevacizumab with trifluridine-tipiracil monotherapy in refractory patients, showing a significant improvement in progression-free survival (PFS) with manageable toxicity [15]. A phase III trial in the same setting is currently ongoing to validate these findings [16].
However, evidence supporting the role of the combination of trifluridine-tipiracil and bevacizumab in a real-world setting is limited. Fujii et al. and Kotani et al. retrospectively analyzed data of patients with refractory mCRC to compare the combination of trifluridine-tipiracil and bevacizumab with trifluridine-tipiracil monotherapy [17, 18]. Both trials also suggested improved outcomes in patients receiving the combination treatment in a real-world setting. Nevertheless, both studies evaluated non-Western patients.
Therefore, the aim of our study was to describe the efficacy and safety of the combination of trifluridine-tipiracil and bevacizumab in a multicenter clinical practice setting in Western patients refractory or intolerant to/ineligible for 5-fluorouracil-based combination treatment.
2 Methods
2.1 Study Design and Patients
This study was developed using a retrospective observational design. Clinical data of patients with mCRC refractory or intolerant to previous therapies who were treated with a combination of trifluridine-tipiracil and bevacizumab at Azienda Ospedaliera Universitaria “Luigi Vanvitelli” and Azienda Sanitaria Locale “Napoli 2 Nord” were collected from medical records and were retrospectively analyzed. Informed consent requirement was waived due to the study’s observational retrospective design.
The eligibility criteria were histologically confirmed metastatic colorectal adenocarcinoma; refractoriness or intolerance to previous therapies, including fluoropyrimidines, irinotecan, oxaliplatin, and anti-VEGF and anti-EGFR antibodies (if RAS/BRAF wild-type); and concurrent treatment with trifluridine-tipiracil and bevacizumab from December 2017 to June 2022. Previous treatment with regorafenib or previous enrollment in clinical trials was allowed. Patient follow-up was performed until June 2022.
2.2 Study Procedures
The trifluridine-tipiracil and bevacizumab regimen consisted of trifluridine-tipiracil administered orally at a dose of 35 mg/m2 of body surface area, administered twice daily on days 1–5 and 8–12 in a 28-day cycle, and bevacizumab administered intravenously at a dose of 5 mg/kg of bodyweight, delivered every 2 weeks in a 28-day cycle.
The following characteristics were recorded for each patient: sex; age at primary diagnosis; age at diagnosis of metastatic disease (if metachronous); age at first administration of study treatment; Eastern Cooperative Oncology Group (ECOG) performance status (PS); previous surgery for primary or metastatic disease; previous locoregional treatment for metastatic disease; stage at diagnosis; primary tumor site; sites of metastatic disease; KRAS/NRAS/BRAF mutational status; MSI (when known); previous treatment administered, both in the (neo)adjuvant or metastatic setting with respective best response, PFS, and OS; and subsequent therapies following study treatment.
2.3 Outcomes
Endpoints investigated included PFS, defined as the time from study treatment start to disease progression or death due to any cause; OS, defined as the time from study treatment start to death from any cause; overall response rate (ORR), defined as the percentage of patients with a complete or partial response to study treatment; and disease control rate (DCR), defined as the percentage of patients with a complete or partial response or stable disease lasting more than 8 weeks from study treatment initiation. Tumor response was evaluated by investigators using the Response Evaluation Criteria in Solid Tumors (RECIST) version 1.1. Adverse events (AEs) were recorded using the Common Terminology Criteria for Adverse Events (CTCAE) version 5.
2.4 Statistical Analysis
Patient characteristics were reported as the median with range of values for continuous variables, and frequencies and percentages for categorical variables. Follow-up time was defined as the time from study treatment start until the last follow-up date for censored cases. Survival curves were generated using Kaplan–Meier estimates. Univariate analyses were performed to assess the impact of treatment on PFS in different patient subgroups. PFS differences were evaluated using the log-rank test, with a two-sided significance level of p = 0.05. Hazard ratios (HR) and corresponding 95% confidence intervals (CIs) were determined using a Cox proportional hazard model. Statistical analyses were performed using IBM SPSS statistics version 22.0 (IBM Corporation, Armonk, NY, USA).
3 Results
3.1 Patients
We recorded 31 patients treated between 1 December 2017 and 30 June 2022. Median age was 69 years (range 38–82 years), 39% were male, 100% had an ECOG PS of 0–1, tumor location was left-sided in 77% of cases, 54% had synchronous presentation, 35% were RAS mutant, and 3% were BRAF mutant. A proportion of patients (55%) had a history of over 18 months of metastatic disease prior to investigational treatment initiation. MSI status was known in 18/31 patients, with 3 of 18 patients displaying an MSI-H profile. Seventy-one percent of patients underwent primary tumor resection, while 29% received either surgery or other locoregional treatments for metastatic disease; 96% of patients had three or fewer sites of metastatic disease, 64% had liver metastases, 55% had lung metastases, and 23% had peritoneal carcinomatosis. The median number of previous treatment lines for metastatic disease was 2 (range 0–5), with 74% of patients receiving experimental treatment as third- or earlier-line treatment. Eighty-four percent of patients received at least one previous anti-angiogenic agent. Patient demographics and baseline characteristics are summarized in Table 1.
3.2 Efficacy
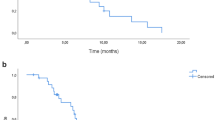
The ORR and DCR were 3% and 71%, respectively (Table 2). With a median follow-up of 8 months (range 2–39), median PFS was 6 months (95% CI 3.1–8.9 months) (Fig. 1a) and median OS was 14 months (95% CI 10.1–17.8 months) (Fig. 1b).
In univariate analysis, longer median PFS was associated with age ≥ 65 years (8 vs. 5 months; HR 0.61, p = 0.29) and male sex (8 vs. 5 months; HR 0.49, p = 0.17). Shorter median PFS was instead associated with RAS mutant status (5 vs. 8 months; HR 1.1, p = 0.85), presence of liver metastases (5 vs. 9 months; HR 1.64, p = 0.33), right primary tumor (5 vs. 6 months; HR 1.82, p = 0.34) and more than three lines of previous treatment (3 vs. 8 months; HR 1.33, p = 0.56); however, none of the highlighted differences were statistically significant.
3.3 Safety
AEs are summarized in Table 3. Overall, AEs of any grade were reported in 58% of patients. The most common grade 3–4 toxicities were neutropenia (19%) and anemia (6%).
Granulocyte colony-stimulating factor (G-CSF) prophylaxis was administered either on first or subsequent cycles of treatment in 35% of patients. Dose delays or dose reductions due to toxicity were required in 35% of patients; 6/31 patients received G-CSF as primary prophylaxis, and 5/31 patients received G-CSF as secondary prophylaxis. Sixty percent of the patients who discontinued treatment eventually received one or more lines of subsequent therapy. Eight of 12 patients received regorafenib as a further line of treatment. No treatment-related deaths occurred.
4 Discussion
Treatment options currently available for refractory mCRC include regorafenib and trifluridine-tipiracil as single-agent therapies. Regulatory approval for both drugs was based on phase III randomized controlled clinical trials. Regorafenib monotherapy in a predominantly Western population provided an ORR of 1% and median PFS and OS of 1.9 months and 6.4 months, respectively [7]. Comparable activity and lower incidence of AEs were also reported using a dose-escalation strategy [19]. On the other hand, single-agent trifluridine-tipiracil yielded a similar benefit in a clinical trial setting, with an ORR of 1.6% and a median PFS and OS of 2.0 and 7.1 months, respectively [6]. Trifluridine-tipiracil monotherapy also achieves similar activity in a real-world setting [20]. Rechallenge with anti-angiogenic agents has been shown to improve PFS and OS in the treatment of mCRC patients who relapse after a first-line therapy containing bevacizumab [21].
The combination of trifluridine-tipiracil and bevacizumab was initially tested in refractory mCRC in the C-TASK FORCE trial [12]. In this phase I/II study, the combination treatment was evaluated in Japanese refractory mCRC patients and yielded a 4% ORR, as evaluated by the investigators, a median PFS of 5.6 months, and a median OS of 11.4 months. The trial also suggested the presence of a modest increase in the risk of neutropenia. A different phase II trial was conducted in Denmark by Pfeiffer et al. comparing the combination therapy with single-agent trifluridine-tipiracil [15]. The authors reported a DCR of 67%, median PFS of 5.6 months, and a median OS of 11.4 months. They also found that bevacizumab did not increase the risk of serious AEs despite the fact that patients receiving combination therapy received treatment for a longer period of time. Both trials consistently showed a benefit, both in median PFS and OS of approximatively 3 months compared with trifluridine-tipiracil monotherapy.
Our study evaluated the activity and safety of a combination of trifluridine-tipiracil in a cohort of real-world Western patients with refractory mCRC. The combination of trifluridine-tipiracil and bevacizumab in our cohort resulted in an ORR of 3% and DCR of 71%. The reported median PFS and OS were 6 and 14 months, respectively, although, interestingly, the generalized application of results recorded is limited by the small sample size and retrospective nature of the analysis. Activity of the combination was comparable with that reported by Pfeiffer et al. [15] in a clinical trial setting, reflecting similar baseline characteristics in the two cohorts (median age, 67 vs. 64 years; left primary, 77% vs. 76%; liver metastases, 64% vs. 61%). However, survival estimates were longer in our analysis, possibly due to a lower proportion of RAS-mutant patients (35% vs. 59%) and a higher fraction of patients receiving trifluridine-tipiracil and bevacizumab in a third- or earlier-line setting (74% vs. 46%). One more possible explanation might lie in the high proportion of patients with good prognosis characteristics (GPC) in our cohort, as defined in the recent work by Tabernero et al. in patients treated with trifluridine-tipiracil monotherapy [22]. In fact, in our series, the majority of patients had three or fewer sites of metastatic disease (30/31) and had a history of advanced CRC of over 18 months (17/31).
Despite lacking statistical significance due to limited sample size, subgroup analysis results were hypothesis-generating and consistent with those previously reported by both Kuboki et al. and Pfeiffer et al. [12, 15], suggesting lower efficacy of the combination in RAS-mutant tumors. A trend in lower efficacy was also observed in the presence of liver metastasis, similar to what was reported by Van Cutsem et al. [13], albeit in a different treatment setting. Furthermore, our analysis suggests greater efficacy being associated with left-sided tumors and earlier implementation of this treatment option. The higher efficacy in patients with RAS wild-type and left-sided tumors also yields the question of whether bevacizumab or an anti-EGFR drug is the best combination option in these subjects. Trifluridine-tipiracil was combined with the anti-EGFR drug panitumumab in patients with wild-type RAS mCRC who were refractory/intolerant to standard therapies other than anti-EGFR therapy, yielding a median PFS and OS of 5.8 months and 14.1 months, respectively [23]. We will hopefully be able to provide a better answer to this question based on upcoming results from the phase II FIRE-8 trial [24], which aims to compare bevacizumab and panitumumab as a combination partner for trifluridine-tipiracil as first-line treatment in patients with RAS wild-type tumors, and from the phase II VELO trial [25], which is investigating a combination of trifluridine-tipiracil and panitumumab versus trifluridine-tipiracil alone as third-line therapy in patients with RAS wild-type tumors who experienced clinical response to EGFR targeting earlier lines of treatment.
The combination of trifluridine-tipiracil and bevacizumab had a manageable safety profile in the real-world setting. AEs of any grade were reported in 58% of patients, with 35% of patients experiencing grade 3 or 4 toxicities. The most frequent higher-grade AEs recorded were neutropenia (19%) and anemia (6%). Compared with the results reported by Kuboki et al. and Pfeiffer et al. [12, 15], a lower incidence of severe neutropenia (19% vs. 67–72%) might be explained by a significant proportion of patients receiving prophylactic G-CSF administration in our cohort (35%).
In line with data previously reported by Kuboki et al. [12], a high percentage of patients received one or more lines of subsequent treatment (60% vs. 80%).
5 Conclusions
In the current study, the combination of trifluridine-tipiracil and bevacizumab showed promising clinical activity in a cohort of real-world patients with refractory mCRC. Additionally, similar to trifluridine-tipiracil alone, toxicities observed with the combination were manageable and in line with the safety report of currently published clinical trials. G-CSF administration might be routinely used to prevent severe neutropenia.
The combination of trifluridine-tipiracil and bevacizumab therefore appears to be a well-tolerated and effective treatment option in pretreated mCRC patients, especially those with RAS wild-type, left-sided tumors. Absence of liver metastases and earlier implementation of this combination in the continuum of care also appear to predict stronger benefit.
Although the application of results reported is limited by the small sample size and retrospective nature of the analysis performed, based on our experience and currently available clinical trial results, we endorse the use of this combination as a treatment option where available.
References
Siegel RL, Miller KD, Fuchs HE, Jemal A. Cancer statistics, 2022. CA Cancer J Clin. 2022;72:7–33.
Biller LH, Schrag D. Diagnosis and treatment of metastatic colorectal cancer: a review. JAMA. 2021;325(7):669–85.
Dekker E, Tanis PJ, Vleugels JLA, Kasi PM, Wallace MB. Colorectal cancer. Lancet. 2019;394(10207):1467–80.
Ciardiello F, Ciardiello D, Martini G, Napolitano S, Tabernero J, Cervantes A. Clinical management of metastatic colorectal cancer in the era of precision medicine. CA Cancer J Clin. 2022;72(4):372–401.
Arrichiello G, Poliero L, Borrelli C, Paragliola F, Nacca V, Napolitano S, et al. Immunotherapy in colorectal cancer: is the long-awaited revolution finally happening? Cancer Treat Res Commun. 2021;28: 100442.
Mayer RJ, Van Cutsem E, Falcone A, Yoshino T, Garcia-Carbonero R, Mizunuma N, et al. Randomized trial of TAS-102 for refractory metastatic colorectal cancer. N Engl J Med. 2015;372:1909–19.
Grothey A, Van Cutsem E, Sobrero A, Siena S, Falcone A, Ychou M, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): An international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381:303–12.
Peeters M, Cervantes A, Moreno Vera S, Taieb J. Trifluridine/tipiracil: an emerging strategy for the management of gastrointestinal cancers. Future Oncol. 2018;14(16):1629–45.
Van Cutsem E, Mayer RJ, Laurent S, Winkler R, Grávalos C, Benavides M, et al. The subgroups of the phase III RECOURSE trial of trifluridine/tipiracil (TAS-102) versus placebo with best supportive care in patients with metastatic colorectal cancer. Eur J Cancer. 2018;90:63–72.
Van Cutsem E, Falcone A, Garcia-Carbonero R, Komatsu Y, Pastorino A, Peeters M, et al. Proxies of quality of life in metastatic colorectal cancer: analyses in the RECOURSE trial. ESMO Open. 2017;2(5): e000261.
Garcia J, Hurwitz HI, Sandler AB, Miles D, Coleman RL, Deurloo R, et al. Bevacizumab (Avastin®) in cancer treatment: a review of 15 years of clinical experience and future outlook. Cancer Treat Rev. 2020;86:102017.
Kuboki Y, Nishina T, Shinozaki E, Yamazaki K, Shitara K, Okamoto W, et al. TAS-102 plus bevacizumab for patients with metastatic colorectal cancer refractory to standard therapies (C-TASK FORCE): an investigator-initiated, open-label, single-arm, multicentre, phase 1/2 study. Lancet Oncol. 2017;18:1172–81.
Van Cutsem E, Danielewicz I, Saunders MP, Pfeiffer P, Argilés G, Borg C, et al. Trifluridine/tipiracil plus bevacizumab in patients with untreated metastatic colorectal cancer ineligible for intensive therapy: the randomized TASCO1 study. Ann Oncol. 2020;31:1160–8.
André T, Falcone A, Shparyk Y, Moiseenko FV, Polo Marques E, Csosziet T, et al. VP11-2021: trifluridine/tipiracil plus bevacizumab vs capecitabine plus bevacizumab as first line treatment for patients with metastatic colorectal cancer ineligible for intensive therapy: the phase III randomized SOLSTICE study. Ann Oncol. 2022;33(2):229–30.
Pfeiffer P, Yilmaz M, Möller S, Zitnjak D, Krogh M, Petersen LN, et al. TAS-102 with or without bevacizumab in patients with chemorefractory metastatic colorectal cancer: an investigator-initiated, open-label, randomised, phase 2 trial. Lancet Oncol. 2020;21:412–20.
Tabernero J, Taieb J, Prager GW, Ciardiello F, Fakih M, Leger C, et al. Trifluridine/tipiracil plus bevacizumab for third-line management of metastatic colorectal cancer: SUNLIGHT study design. Futur Oncol. 2021;17:1977–85.
Kotani D, Kuboki Y, Horasawa S, Kaneko A, Nakamura Y, Kawazoe A, et al. Retrospective cohort study of trifluridine/tipiracil (TAS-102) plus bevacizumab versus trifluridine/tipiracil monotherapy for metastatic colorectal cancer. BMC Cancer. 2019;19(1):1253.
Fujii H, Matsuhashi N, Kitahora M, Takahashi T, Hirose C, Iihara H, et al. Bevacizumab in combination with TAS-102 improves clinical outcomes in patients with refractory metastatic colorectal cancer: a retrospective study. Oncologist. 2020;25:e469–76.
Bekaii-Saab TS, Ou FS, Ahn DH, Boland PM, Ciombor KK, Heying EN, et al. Regorafenib dose-optimisation in patients with refractory metastatic colorectal cancer (ReDOS): a randomised, multicentre, open-label, phase 2 study. Lancet Oncol. 2019;20:1070–82.
Cremolini C, Rossini D, Martinelli E, Pietrantonio F, Lonardi S, Noventa S, et al. Trifluridine/Tipiracil (TAS-102) in refractory metastatic colorectal cancer: a multicenter register in the frame of the Italian compassionate use program. Oncologist. 2018;23:1178–87.
Xiong Y-X, Ren L, Wang Z-Q, Huang X-W, Zhou Y-J. The role of angiogenesis inhibitors re-challenge in colorectal cancer previously treated with bevacizumab: a meta-analysis of randomized controlled trials. Eur Rev Med Pharmacol Sci. 2017;21:1489–94.
Tabernero J, Argiles G, Sobrero AF, Borg C, Ohtsu A, Mayer RJ, et al. Effect of trifluridine/tipiracil in patients treated in RECOURSE by prognostic factors at baseline: An exploratory analysis. ESMO Open. 2020;5(4):e000752.
Kato T, Kagawa Y, Kuboki Y, Gamoh M, Komatsu Y, Yasui H, et al. Safety and efficacy of panitumumab in combination with trifluridine/tipiracil for pre-treated patients with unresectable, metastatic colorectal cancer with wild-type RAS: The phase 1/2 APOLLON study. Int J Clin Oncol. 2021;26:1238–47.
Sommerhäuser G, Kurreck A, Stintzing S, Heinemann V, von Weikersthal LF, Dechow T, et al. Study protocol of the FIRE-8 (AIO-KRK/YMO-0519) trial: a prospective, randomized, open-label, multicenter phase II trial investigating the efficacy of trifluridine/tipiracil plus panitumumab versus trifluridine/tipiracil plus bevacizumab as first-line treatment in patients with metastatic colorectal cancer. BMC Cancer. 2022;22:820.
Martinelli E, Ciardiello D, Martini G, Troiani T, Cardone C, Vitiello PP, et al. Implementing anti-epidermal growth factor receptor (EGFR) therapy in metastatic colorectal cancer: challenges and future perspectives. Ann Oncol. 2020;31:30–40.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open access funding provided by Università degli Studi della Campania Luigi Vanvitelli within the CRUI-CARE Agreement. This research did not receive any specific grants from funding agencies in the public, commercial, or not-for-profit sectors.
Conflicts of interest
Erika Martinelli has served as an adviser and speaker for AstraZeneca, Amgen, Bayer, Merck-Serono, Roche, Sanofi, Servier, and Pierre Fabre. Davide Ciardiello has served as an adviser and speaker for Roche, Amgen, Merck-Serono, Pfizer, Sanofi, Bayer, Servier, BMS, Cellgene, and Lilly, and has received institutional research grants from Bayer, Roche, Merck-Serono, Amgen, AstraZeneca, and Takeda. Teresa Troiani has served as an adviser and speaker for Roche, Merck-Serono, Sanofi, Servier, Novartis, and Bayer. Gianluca Arrichiello, Alessandra Perrone, Stefania Napolitano, Giulia Martini, Vincenzo De Falco, Pasquale Incoronato, Maria Maddalena Laterza, Gaetano Facchini, Vincenzo Famiglietti, Valeria Nacca, Fernando Paragliola, Rossella Napolitano, Gabriella Suarato, Antonella Nicastro, and Fortunato Ciardiello report they have no conflicts of interest that might be relevant to the contents of this manuscript.
Ethics approval, consent to participate, and consent for publication
Patient informed consent for participation requirement was waived due to the observational retrospective design of this study. Patient consent for publication was collected as per local policy.
Availability of data and material, and code availability
All data generated or analyzed during this study are included in this published article.
Authors’ contributions
GA, AP, EM, and TT contributed to the conception and design of this study. GA, EM, and TT wrote the first draft of the manuscript. GA, EM, and TT revised the manuscript. All authors contributed to manuscript revision, and read and approved the submitted version.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Arrichiello, G., Perrone, A., Napolitano, S. et al. Real-World Activity and Safety of Trifluridine-Tipiracil Plus Bevacizumab Therapy in Patients with Refractory Metastatic Colorectal Cancer. Targ Oncol 17, 635–642 (2022). https://doi.org/10.1007/s11523-022-00916-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-022-00916-8