Abstract
Small molecule mesenchymal-epithelial transition (MET) inhibitors, such as crizotinib, capmatinib, and tepotinib, are treatment options for metastatic non-small cell lung cancer (NSCLC) in adult patients whose tumors have a mutation that leads to MET exon 14 skipping. In clinical trials, these MET inhibitors were associated with a high incidence of peripheral edema, although this was generally mild-to-moderate in severity. There is limited information about the mechanism involved in MET inhibitor-induced peripheral edema. Perturbation of hepatocyte growth factor (HGF)/MET signaling may disrupt the permeability balance in the vascular endothelium and thus promote edema development. Another potential mechanism is through effects on renal function, although this is unlikely to be the primary mechanism. Because edema is common in cancer patients and may not necessarily be caused by the cancer treatment, or other conditions that have similar symptoms to peripheral edema, a thorough assessment is required to ascertain the underlying cause. Before starting MET-inhibitor therapy, patients should be educated about the possibility of developing peripheral edema. Patient limb volume should be measured before initiating treatment, to aid assessment if symptoms develop. Since the exact mechanism of MET inhibitor-induced edema is unknown, management is empiric, with common approaches including compression stockings, specific exercises, massage, limb elevation, and/or diuretic treatment. Although not usually required, discontinuation of MET inhibitor treatment generally resolves peripheral edema. Early diagnosis and management, as well as patient information and education, are vital to decrease the clinical burden associated with edema, and to reinforce capmatinib treatment adherence.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Peripheral edema (usually mild/moderate) is common in patients receiving small molecule mesenchymal-epithelial transition (MET) inhibitors. |
Discerning the etiology of peripheral edema is important for optimal management. |
Patient information and education are important approaches to limiting the impact of MET inhibitor-related edema. It can generally be managed using diuretics, elevation, compression stockings, exercise, and dietary changes, in addition to dose reduction or interruption in patients with persistent Grade ≥ 2 edema. |
1 Introduction
The small molecule mesenchymal-epithelial transition (MET) tyrosine kinase inhibitors capmatinib (Tabrecta®; Novartis, East Hanover, NJ, USA) and tepotinib (Tepmetco®; Merck KGaA, Darmstadt, Germany) are both approved as first-line (in the USA [1, 2]) or line-agnostic (in Japan [3, 4]) treatment of metastatic non-small cell lung cancer (NSCLC) in adult patients whose tumors have a mutation that leads to MET exon 14 (METex14) skipping. This mutation predominantly occurs in NSCLC, and is present in about 3–4% of all patients with NSCLC [5]. In Europe, tepotinib is approved in patients previously treated with immunotherapy or platinum-based chemotherapy [6], and capmatinib has received a positive opinion from the Committee for Medicinal Products for Human Use for approval in this indication [7]. Other small molecule MET inhibitors that may be used in this setting include crizotinib (Xalkori®; Pfizer, NY, USA) [8] and savolitinib (Orpathys®; HUTCHMED, China, and AstraZeneca, Cambridge, UK) [9], although the latter agent is only approved in China. Crizotinib is a type Ia inhibitor of MET, anaplastic lymphoma kinase (ALK), and c-ros proto-oncogene 1 (ROS1), while capmatinib, tepotinib, and savolitinib are type Ib MET inhibitors that target and selectively bind to MET, including the mutant variant produced by METex14 skipping [5, 10]. Capmatinib and tepotinib have demonstrated clinically meaningful efficacy and a good tolerability profile in adult patients with advanced NSCLC with this mutation in several clinical trials [11,12,13,14,15]. The National Comprehensive Cancer Network guidelines now recommend capmatinib or tepotinib as first-line therapy in patients with the METex14 mutation, with crizotinib being considered useful in certain circumstances [8]. Prior to the approval of these small molecule MET inhibitors, first-line treatment for patients with metastatic NSCLC included platinum doublet chemotherapy with or without vascular endothelial growth factor (VEGF) signaling pathway inhibitors [16,17,18]. Due to the mechanism of action (i.e., anti-angiogenesis), the inhibition of the VEGF pathway can lead to vascular disturbances including hypertension and proteinuria, which can be intensified by concurrent pathologic conditions [19]. In contrast, MET inhibitors have limited effect on renal function, although reversible increases in creatinine levels were observed in 24% of patients treated with capmatinib [12] and 27% of those treated with tepotinib [14].
In clinical trials, MET inhibitors, such as crizotinib, capmatinib, and tepotinib, have been associated with a high incidence of peripheral edema [5, 10]. The incidence of cancer drug-induced peripheral edema is often difficult to ascertain. There is no specific definition of peripheral edema in the latest version of the Common Terminology Criteria for Adverse Events (CTCAE), although there is a definition of edema limb [20]. Clinical trials may not all use the same terms, or they may group several CTCAE events together, for example, as ‘edema’. Furthermore, peripheral edema is common in cancer patients, and may not necessarily be drug related [21], and patients may have other conditions with symptoms similar to peripheral edema [22]. Consequently, peripheral edema may be misdiagnosed or under-recognized.
The aim of this review is to describe the incidence of peripheral edema in patients treated with small molecule MET inhibitors, the potential molecular mechanism of this toxicity, and ways in which to manage it. We also highlight the need to accurately define peripheral edema in order to initiate early management and avoid negative effects on patients’ quality of life.
2 Methods
Literature searches of PubMed and SCOPUS (from January 2000 to June 2022) were performed using various relevant search terms (‘peripheral edema’, ‘non-small cell lung cancer’, ‘MET inhibitor’, ‘capmatinib’, ‘tepotinib’, ‘crizotinib’, ‘savolitinib’, ‘supportive care’, ‘management’ and ‘adverse events’) to identify English-language clinical data on the incidence, mechanism, and management of peripheral edema associated with the use of small molecule MET inhibitors. The reference lists of identified studies were screened for additional information. The data from the literature search were used to supplement the authors’ clinical experience in using MET inhibitors and in managing associated peripheral edema.
3 Incidence of Peripheral Edema in Clinical Trials
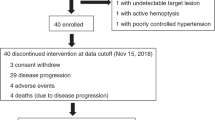
The incidence of peripheral edema associated with MET inhibitors in clinical trials is summarized in Table 1. In Phase I studies of capmatinib, peripheral edema was one of the most common adverse events (AEs). In an open-label Phase I study in patients with MET-positive solid tumors, peripheral edema was one of the most commonly reported AEs with capmatinib monotherapy (expansion dose: 400 mg twice daily [tablets] or 600 mg twice daily [capsules]), occurring in 39% of patients in the dose-expansion phase, and was suspected to be treatment related in 26% of patients [23]. Similarly, the incidence of peripheral edema of any grade was 20.5% in a Japanese open-label, Phase I dose-escalation and -expansion trial of capmatinib (n = 44; dose range 100 mg once daily to 600 mg twice daily) in patients with advanced solid tumors (not selected based on MET dysregulation status) [24]. In the Phase II GEOMETRY mono-1 study in 364 patients with MET-dysregulated advanced NSCLC, peripheral edema was the most common AE with capmatinib (400 mg tablets, twice daily), developing in 51% of patients (treatment-related in 43%), and resulted in permanent treatment discontinuation in six patients [12]. Although the majority of cases were mild or moderate in severity, 9% of patients had Grade 3 or 4 peripheral edema [12]. In a preplanned analysis of Japanese patients enrolled in GEOMETRY mono-1 (n = 45), peripheral edema was the second most frequent treatment-related AE, occurring in 31% of patients [25]. More recently, real-world data from an international early access program study of capmatinib in 81 patients with advanced METex14-mutated NSCLC found that peripheral edema was the most common treatment-related AE of any grade (48%) or Grade ≥ 3 (13%) [26].
The MET inhibitor crizotinib has also been associated with peripheral edema. In the Phase I PROFILE 1001 study of crizotinib in patients with METex14-altered NSCLC (n = 69), the most common treatment-related AE was edema (51%; reported as a clustered term according to CTCAE, version 3.0) [27]. The Phase II METROS study in patients with MET-deregulated or ROS1-rearranged NSCLC also showed a high incidence of peripheral edema with crizotinib, with 31% of patients with MET-deregulated NSCLC having treatment-related peripheral edema [28].
Peripheral edema was the one of most common treatment-related AEs in a Phase I study of tepotinib in patients with advanced solid tumors (n = 149), reported in 26% of patients receiving micronized tepotinib capsules (300–1200 mg once daily for 3 weeks) [29]. In the Phase II VISION study of tepotinib in patients with METex14 NSCLC, peripheral edema was the most common treatment-related AE, reported in 63% of patients and leading to a dose reduction or interruption in 16 and 18%, respectively [14]. In a Japanese subset analysis of the VISION study, peripheral edema was the second most common treatment-related AE, reported by 47% of patients [15]. Although common, peripheral edema was manageable and did not lead to permanent treatment discontinuation in any of these patients [15].
Early clinical trials of savolitinib have shown that this selective MET inhibitor is also associated with a high incidence of peripheral edema. Open-label, Phase I studies in patients with advanced solid tumors reported treatment-related peripheral edema in 21–23% of patients [30, 31]. In a Phase II Chinese study in patients with METex14 skipping NSCLC (n = 70), peripheral edema was the most common treatment-related AE of any grade (54%) or Grade ≥ 3 (9%) with savolitinib (400 or 600 mg once daily) [32].
4 Potential Mechanisms of Edema with MET Inhibitors
Peripheral edema is the result of a perturbation in fluid homeostasis between the vascular, lymphatic, and interstitial spaces [22]. Many drugs can cause peripheral edema via different mechanisms that can combine synergistically [33]. Potential mechanisms include precapillary arteriolar vasodilation (vasodilatory edema), sodium and/or water retention (renal edema), lymphatic insufficiency (lymphedema), and increased capillary permeability (permeability edema).
Despite the high incidence of peripheral edema in patients receiving MET inhibitors, there is limited information in the literature about the mechanism involved. Mesenchymal-epithelial transition is a proto-oncogenic gene whose gene product naturally binds to hepatocyte growth factor (HGF), controlling a wide range of signaling pathways, including proliferation, motility, migration, and invasion [5]. Thus, MET dysregulation, due to an ongoing oncogenic process, is associated with the development and progression of several types of cancer, including NSCLC [5, 34, 35]. Hepatocyte growth factor is a powerful pro-angiogenic protein that also inhibits vascular permeability and inflammation and attenuates thrombin-induced endothelial permeability [35, 36]. The perturbation of the HGF/MET signaling by the inhibition of MET could disrupt the permeability balance in the vascular endothelium [36], thus, promoting edema development. A study in healthy volunteers treated with capmatinib showed that the drug was largely distributed to the peripheral tissues [37], which could contribute to the development of peripheral edema in patients treated with MET inhibitors.
Another potential mechanism by which MET inhibitors may cause edema is through effects on renal function. The Phase I dose-escalation study and the GEOMETRY mono-1 study of capmatinib [12, 23, 24] and the Phase I study and the VISION study of tepotinib [14, 29] showed elevated serum creatinine levels during treatment, an effect that seemed to be dose dependent. However, the number of participants per dose group in the capmatinib dose-escalation study was too small to draw conclusions [24].
Serum creatinine is cleared by active tubular secretion and renal transporters, such as multidrug and toxic extrusion (MATE) and organic anion transporters, in addition to renal glomerular filtration [38]. The increase in creatinine levels observed during capmatinib or tepotinib treatment could be due to the inhibition of the MATE proteins 1 and 2-K, since both agents are thought to inhibit these renal transporters [6, 12]. However, these changes in serum creatinine do not appear to be accompanied by a clinically meaningful impairment in renal function, so this is unlikely to be the primary mechanism of edema development.
There is some clinical evidence to suggest that the mechanism of MET inhibitor-induced peripheral edema is different from that of VEGF inhibitor-induced edema. In contrast to HGF-related inhibition of vascular permeability, VEGF promotes endothelial permeability [35, 39]. Therefore, although both MET inhibitors and VEGF inhibitors disrupt the homeostatic balance, VEGF inhibitors affect a wider range of the inhibitory and stimulatory factors controlling vascular permeability in the peripheral circulation [40].
5 Diagnosis and Management of MET Inhibitor-Induced Edema
A study of edema in advanced cancer revealed that patients with edema had a high symptom burden, including pain, limb swelling, heaviness, paresthesia, and concomitant overall impairment of well-being [41]. Although intervention is not always necessary, peripheral edema may become an issue if left unmanaged, especially for older and/or frail patients who are more susceptible to toxicities and are more likely to have other comorbidities. In addition, peripheral edema can necessitate cancer treatment dose interruption or reduction, and sometimes treatment discontinuation [12].
Before initiating MET inhibitor treatment, patients should be advised of the likelihood of edema development and assessed for any underlying conditions that might predispose them to developing edema [21]. Edema is common in patients with cancer [21], and may not necessarily be caused by their treatment. Thus, it is important to investigate the underlying cause, as their cancer treatment might exacerbate an existing comorbidity [21]. Physicians also need to distinguish between lymphedema (secondary lymphedema) and peripheral edema, both of which can be caused by cancer treatment [22, 42]. While peripheral edema caused by MET inhibitors is systemic, reversible, and often does not require treatment (as high-grade edema is rare) [21], lymphedema is local, chronic, and requires palliative care [43]; MET inhibitor treatment has not been associated with lymphedema [12, 14, 28, 32]. A careful history of the timing of the peripheral edema, and whether it changes with body position, is essential, and may provide clues to the underlying cause [44]. Lower extremity examination, tests for renal, hepatic, or thyroid function, or markers of heart failure, such as B-type natriuretic peptide, may also help to elucidate the underlying cause [44].
Since the exact mechanism by which MET inhibitors induce edema is unclear, management is empiric [21]. Multiple approaches may be used, including compression stockings, and lifestyle and dietary changes (Table 2). In clinical practice, diuretic therapy is administered as first-line treatment and patients are advised to raise their legs to reduce lower limb edema. If edema subsequently persists or interferes with the activities of daily life, dose adjustment or interruption of MET inhibitor therapy should be considered (Table 3). Patients should also be advised about appropriate skin and foot care to prevent secondary cellulitis [44].
In clinical trials of MET inhibitors, most cases of peripheral edema were mild-to-moderate in severity (refer to Table 3 for grading criteria). In a post hoc analysis of the GEOMETRY mono-1 study, 58% of the patients who developed peripheral edema during capmatinib treatment required additional therapy [45]. Of these, 81% were prescribed diuretics and 11% used compression stockings. A report on the experiences of two US-based institutions involved in this study found that peripheral edema sometimes occurred within the first 3 weeks of treatment, was generally mild, and was usually managed with one or a combination of the following: compression stockings, elevation, and diuretics [45]. One of these institutions (Massachusetts General Hospital) referred patients with peripheral edema to a lymphedema clinic, where symptoms were managed with lymphatic massage, stretching exercises, compression stockings (prescription grade), or a combination of these treatments. In some patients, these physiotherapeutic methods improved lower edema; in those patients for whom bilateral lower edema did not resolve, discontinuation of capmatinib resulted in a resolution of symptoms [45]. The authors’ clinical experience is that such measures are often only temporarily effective, and that discontinuation of MET inhibitor therapy is frequently the only approach to completely resolving drug-induced peripheral edema.
Given the reasonably high incidence of peripheral edema in patients receiving MET inhibitors, the above-mentioned lymphedema clinic [45] recommends that limb volume is measured before initiating treatment, and again if edema symptoms develop. It further recommends that a volume change of 5–10% indicates the patient should be closely monitored, while a > 10% change indicates compression therapy should be initiated.
6 Conclusions
Small molecule MET inhibitors have proven efficacy and acceptable tolerability in the treatment of patients with METex14-mutant NSCLC. Despite the high incidence of peripheral edema in patients treated with MET inhibitors, most cases are mild-to-moderate in severity, and only a small percentage of patients require treatment interruption or discontinuation. Early diagnosis and management of peripheral edema, as well as patient information and education, are vital to decrease the clinical burden associated with peripheral edema and to reinforce treatment adherence. In addition, determining the etiology of the edema is important, as MET inhibitor therapy may be only one of several potential causes of edema in a patient with cancer.
References
U.S. Food and Drug Administration. TabrectaTM (capmatinib) tablets, for oral use. 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/213591s000lbl.pdf. Accessed June 2022.
U.S. Food and Drug Administration. Tepmetko® (tepotinib) tablets, for oral use. 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/214096s000lbl.pdf. Accessed June 2022.
Merck Global. Tepmetko (tepotinib) approved in Japan for advanced NSCLC with METex14 skipping alterations. 2020. https://www.merckgroup.com/en/news/tepotinib-25-03-2020.html. Accessed June 2022.
Novartis. Novartis announces MET inhibitor Tabrecta™ approved in Japan for advanced non-small cell lung cancer with METex14. 2020. https://www.novartis.com/news/media-releases/novartis-announces-met-inhibitor-tabrectatm-approved-japan-advanced-non-small-cell-lung-cancer-metex14. Accessed June 2022.
Puccini A, Marín-Ramos NI, Bergamo F, Schirripa M, Lonardi S, Lenz H-J, et al. Safety and tolerability of c-MET inhibitors in cancer. Drug Saf. 2019;42(2):211–33. https://doi.org/10.1007/s40264-018-0780-x.
European Medicines Agency. Tepmetko 225 mg film-coated tablets. 2022. https://www.ema.europa.eu/documents/product-information/tepmetko-epar-product-information_en.pdf. Accessed June 2022.
European Medicines Agency. CHMP summary of positive opinion for Tabrecta (capmatinib). 2022. https://www.ema.europa.eu/documents/smop-initial/chmp-summary-positive-opinion-tabrecta_en.pdf. Accessed June 2022.
National Comprehensive Cancer Network. NCCN clinical practise guidelines in oncology. Non-small cell lung cancer, version 3.2022. 2022. https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf. Accessed June 2022.
Markham A. Savolitinib: first approval. Drugs. 2021;81(14):1665–70. https://doi.org/10.1007/s40265-021-01584-0.
Cortot A, Le X, Smit E, Viteri S, Kato T, Sakai H, et al. Safety of MET tyrosine kinase inhibitors in patients with MET exon 14 skipping non-small cell lung cancer: a clinical review. Clin Lung Cancer. 2022;23(3):195–207. https://doi.org/10.1016/j.cllc.2022.01.003.
Schuler MH, Berardi R, Lim WT, Van Geel R, De Jonge MJ, Bauer TM, et al. Phase (Ph) I study of the safety and efficacy of the cMET inhibitor capmatinib (INC280) in patients (pts) with advanced cMET+ non-small cell lung cancer (NSCLC). J Clin Oncol. 2016;34(Suppl 15):9067.
Wolf J, Seto T, Han J-Y, Reguart N, Garon EB, Groen HJ, et al. Capmatinib in MET exon 14–mutated or MET-amplified non–small-cell lung cancer. N Engl J Med. 2020;383(10):944–57.
Le X, Sakai H, Felip E, Veillon R, Garassino MC, Raskin J, et al. Tepotinib efficacy and safety in patients with MET exon 14 skipping NSCLC: outcomes in patient subgroups from the VISION study with relevance for clinical practice. Clin Cancer Res. 2022;28(6):1117–26. https://doi.org/10.1158/1078-0432.CCR-21-2733.
Paik PK, Felip E, Veillon R, Sakai H, Cortot AB, Garassino MC, et al. Tepotinib in non-small-cell lung cancer with MET exon 14 skipping mutations. N Engl J Med. 2020;383(10):931–43. https://doi.org/10.1056/NEJMoa2004407.
Sakai H, Morise M, Kato T, Matsumoto S, Sakamoto T, Kumagai T, et al. Tepotinib in patients with NSCLC harbouring MET exon 14 skipping: Japanese subset analysis from the Phase II VISION study. Jpn J Clin Oncol. 2021;51(8):1261–8. https://doi.org/10.1093/jjco/hyab072.
U.S. Food and Drug Administration. Tarceva (erlotinib) tablets, for oral use. 2016. https://www.accessdata.fda.gov/drugsatfda_docs/label/2016/021743s025lbl.pdf. Accessed 5 July 2021.
U.S. Food and Drug Administration. Iressa (gefitinib) tablets for oral use. 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/206995s004lbl.pdf. Accessed 5 July 2021.
U.S. Food and Drug Administration. Avastin® (bevacizumab) injection, for intravenous use. 2020. https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/125085s337lbl.pdf. Accessed 5 July 2021.
Gurevich F, Perazella MA. Renal effects of anti-angiogenesis therapy: update for the internist. Am J Med. 2009;122(4):322–8. https://doi.org/10.1016/j.amjmed.2008.11.025.
National Cancer Institute. Common Terminology Criteria for Adverse Events (CTCAE). 2017. National Cancer Institute, https://ctep.cancer.gov/protocolDevelopment/electronic_applications/ctc.htm#ctc_50. Accessed 18 Jan 2021.
Yang Y, Liu YH, Sun X, Yu MW, Yang L, Cheng PY, et al. Risk of peripheral edema in cancer patients treated with MEK inhibitors: a systematic review and meta-analysis of clinical trials. Curr Med Res Opin. 2017;33(9):1663–75. https://doi.org/10.1080/03007995.2017.1349657.
Cho S, Atwood JE. Peripheral edema. Am J Med. 2002;113(7):580–6. https://doi.org/10.1016/S0002-9343(02)01322-0.
Bang YJ, Su WC, Schuler M, Nam DH, Lim WT, Bauer TM, et al. Phase 1 study of capmatinib in MET-positive solid tumor patients: dose escalation and expansion of selected cohorts. Cancer Sci. 2020;111(2):536–47. https://doi.org/10.1111/cas.14254.
Esaki T, Hirai F, Makiyama A, Seto T, Bando H, Naito Y, et al. Phase I dose-escalation study of capmatinib (INC280) in Japanese patients with advanced solid tumors. Cancer Sci. 2019;110(4):1340–51. https://doi.org/10.1111/cas.13956.
Seto T, Ohashi K, Sugawara S, Nishio M, Takeda M, Aoe K, et al. Capmatinib in Japanese patients with MET exon 14 skipping-mutated or MET-amplified advanced NSCLC: GEOMETRY mono-1 study. Cancer Sci. 2021;112(4):1556–66. https://doi.org/10.1111/cas.14826.
Illini O, Fabikan H, Swalduz A, Vikström A, Krenbek D, Schumacher M, et al. Real-world experience with capmatinib in MET exon 14-mutated non-small cell lung cancer (RECAP): a retrospective analysis from an early access program. Ther Adv Med Oncol. 2022;14:17588359221103206. https://doi.org/10.1177/17588359221103206.
Drilon A, Clark JW, Weiss J, Ou SI, Camidge DR, Solomon BJ, et al. Antitumor activity of crizotinib in lung cancers harboring a MET exon 14 alteration. Nat Med. 2020;26(1):47–51. https://doi.org/10.1038/s41591-019-0716-8.
Landi L, Chiari R, Tiseo M, D’Inca F, Dazzi C, Chella A, et al. Crizotinib in MET-deregulated or ROS1-rearranged pretreated non-small cell lung cancer (METROS): a phase II, prospective, multicenter, two-arms trial. Clin Cancer Res. 2019;25(24):7312–9. https://doi.org/10.1158/1078-0432.CCR-19-0994.
Falchook GS, Kurzrock R, Amin HM, Xiong W, Fu S, Piha-Paul SA, et al. First-in-man phase I trial of the selective MET inhibitor tepotinib in patients with advanced solid tumors. Clin Cancer Res. 2020;26(6):1237–46.
Gan HK, Millward M, Hua Y, Qi C, Sai Y, Su W, et al. First-in-human phase I study of the selective MET inhibitor, savolitinib, in patients with advanced solid tumors: safety, pharmacokinetics, and antitumor activity. Clin Cancer Res. 2019;25(16):4924–32. https://doi.org/10.1158/1078-0432.CCR-18-1189.
Wang Y, Liu T, Chen G, Gong J, Bai Y, Zhang T, et al. Phase Ia/Ib study of the selective MET inhibitor, savolitinib, in patients with advanced solid tumors: safety, efficacy, and biomarkers. Oncologist. 2022;27(5):342-e83. https://doi.org/10.1093/oncolo/oyab066.
Lu S, Fang J, Li X, Cao L, Zhou J, Guo Q, et al. Once-daily savolitinib in Chinese patients with pulmonary sarcomatoid carcinomas and other non-small-cell lung cancers harbouring MET exon 14 skipping alterations: a multicentre, single-arm, open-label, phase 2 study. Lancet Respir Med. 2021;9(10):1154–64. https://doi.org/10.1016/s2213-2600(21)00084-9.
Largeau B, Cracowski JL, Lengellé C, Sautenet B, Jonville-Béra AP. Drug-induced peripheral oedema: an aetiology-based review. Br J Clin Pharmacol. 2021;87(8):3043–55. https://doi.org/10.1111/bcp.14752.
Dhillon S. Capmatinib: first approval. Drugs. 2020;80(11):1125–31. https://doi.org/10.1007/s40265-020-01347-3.
Gallo S, Sala V, Gatti S, Crepaldi T. HGF/MET axis in heart function and cardioprotection. Biomedicines. 2014;2(4):247–62. https://doi.org/10.3390/biomedicines2040247.
Hack SP, Bruey JM, Koeppen H. HGF/MET-directed therapeutics in gastroesophageal cancer: a review of clinical and biomarker development. Oncotarget. 2014;5(10):2866–80. https://doi.org/10.18632/oncotarget.2003.
Glaenzel U, Jin Y, Hansen R, Schroer K, Rahmanzadeh G, Pfaar U, et al. Absorption, distribution, metabolism, and excretion of capmatinib (INC280) in healthy male volunteers and in vitro aldehyde oxidase phenotyping of the major metabolite. Drug Metab Dispos. 2020;48(10):873–85. https://doi.org/10.1124/dmd.119.090324.
Lepist EI, Zhang X, Hao J, Huang J, Kosaka A, Birkus G, et al. Contribution of the organic anion transporter OAT2 to the renal active tubular secretion of creatinine and mechanism for serum creatinine elevations caused by cobicistat. Kidney Int. 2014;86(2):350–7. https://doi.org/10.1038/ki.2014.66.
Gallo S, Sala V, Gatti S, Crepaldi T. Cellular and molecular mechanisms of HGF/MET in the cardiovascular system. Clin Sci (Lond). 2015;129(12):1173–93. https://doi.org/10.1042/cs20150502.
Kamba T, McDonald DM. Mechanisms of adverse effects of anti-VEGF therapy for cancer. Br J Cancer. 2007;96(12):1788–95. https://doi.org/10.1038/sj.bjc.6603813.
Gradalski T. Edema of advanced cancer: prevalence, etiology, and conservative management—a single hospice cross-sectional study. J Pain Symptom Manag. 2019;57(2):311–8. https://doi.org/10.1016/j.jpainsymman.2018.11.005.
Shallwani SM, Hodgson P, Towers A. Comparisons between cancer-related and noncancer-related lymphedema: an overview of new patients referred to a specialized hospital-based center in Canada. Lymphat Res Biol. 2017;15(1):64–9. https://doi.org/10.1089/lrb.2016.0023.
Cormier JN, Askew RL, Mungovan KS, Xing Y, Ross MI, Armer JM. Lymphedema beyond breast cancer. Cancer. 2010;116(22):5138–49. https://doi.org/10.1002/cncr.25458.
Trayes KP, Studdiford JS, Pickle S, Tully AS. Edema: diagnosis and management. Am Fam Physician. 2013;88(2):102–10.
Goodwin K, Ledezma B, Heist RS, Garon EB. Management of selected adverse events with capmatinib: institutional experiences from the GEOMETRY mono-1 trial [abstract MO01.04 plus poster presentation]. J Thorac Oncol. 2021;16:S16–7. https://doi.org/10.1016/j.jtho.2020.10.052.
Reed M, Rosales ALS, Chioda MD, Parker L, Devgan G, Kettle J. Consensus recommendations for management and counseling of adverse events associated with lorlatinib: a guide for healthcare practitioners. Adv Ther. 2020;37(6):3019–30. https://doi.org/10.1007/s12325-020-01365-3.
Acknowledgements
We would like to thank Alma Orts-Sebastian, PhD, and Toni Dando who, under the guidance of the authors, wrote the outline and first draft, respectively. This medical writing assistance was provided by inScience Communications, Springer Healthcare, and was funded by Novartis, Japan.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Assistance with the preparation of this manuscript was funded by Novartis, Japan.
Conflict of interest
Makoto Nishio has received Grants and personal fees from AstraZeneca, Bristol Myers Squibb, Chugai Pharmaceutical, Daiichi Sankyo, Eli Lilly, MSD, Novartis, Ono Pharmaceutical, Pfizer, Takeda Pharmaceutical Company Limited, and Taiho Pharmaceutical; and personal fees from AbbVie, Boehringer-Ingelheim, Merck Biopharma, and TEIJIN PHARMA LIMITED, outside the submitted work. Terufumi Kato has received Grants and personal fees from Abbvie, Amgen, AstraZeneca, Bristol Myers Squibb, Chugai, Eli Lilly, Merck Biopharma, MSD, Novartis, Ono, Pfizer, and Taiho; Grants from Regeneron; and personal fees from Boehringer Ingelheim, Daiichi-Sankyo, Nippon Kayaku, and Takeda. Ryo Toyozawa has received honoraria for lectures from Bristol-Myers Squibb, Chugai Pharmaceutical, Eli Lilly Japan, Kyowa Hakko Kirin, MSD, Nippon Boehringer Ingelheim, Nippon Kayaku, Novartis Pharma, and Taiho Pharmaceutical; and his institution has received Grants from Abbvie, Amgen, Daiichi Sankyo, Eli Lilly Japan, Novartis Pharma, Pfizer Japan, and Takeda Pharmaceutical. Toyoaki Hida has received Grants and personal fees from Novartis, Merck, AstraZeneca and Pfizer.
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Availability of data and material
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Code availability
Not applicable.
Author contributions
All authors contributed to the focus and scope, as well as concept of this review. All authors reviewed the text for intellectual content, read and approved drafts, and take responsibility for the content of the review.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Nishio, M., Kato, T., Toyozawa, R. et al. Management of Peripheral Edema in Patients with MET Exon 14-Mutated Non-small Cell Lung Cancer Treated with Small Molecule MET Inhibitors. Targ Oncol 17, 597–604 (2022). https://doi.org/10.1007/s11523-022-00912-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-022-00912-y