Abstract
Background
Targeted agents, such as antiangiogenic drugs (e.g., bevacizumab) and poly(ADP-ribose) polymerase inhibitors (e.g., rucaparib), have been shown to improve outcomes in patients with newly diagnosed or recurrent ovarian cancer. Evidence suggests that combinations of these two classes of targeted agents may result in synergistic antitumor activity.
Objective
The phase I portion of MITO 25 was designed to determine the maximum tolerated dose, pharmacokinetics, and the safety profile of rucaparib when administered in combination with bevacizumab as maintenance treatment for patients with high-grade epithelial ovarian, fallopian tube, or primary peritoneal cancer.
Methods
This was a single-arm, phase I dose-escalation study. Cohorts of three patients were recruited to receive increasing rucaparib doses of 400 mg, 500 mg, or 600 mg twice daily for 28 days. Bevacizumab 15 mg/kg was administered at day 1 every 21 days.
Results
We enrolled nine patients. Two patients in the rucaparib 600-mg group had four grade 3 treatment-emergent adverse events: increased in alanine aminotransferase and aspartate aminotransferase levels, depression, and hallucinations. These were deemed to be dose-limiting toxicities related to rucaparib. Because these dose-limiting toxicities occurred in the 600-mg group and affected more than one in three patients, the maximum tolerated dose for rucaparib was considered 500 mg twice daily when combined with bevacizumab 15 mg/kg at day 1 every 21 days. There were no new safety concerns from using the combination. No substantial difference in pharmacokinetic parameters was found between the cohorts or in the pharmacokinetic profiles of rucaparib administered alone or with bevacizumab with respect to historical controls.
Conclusions
The maximum tolerated dose of rucaparib is 500 mg twice daily when co-administered with bevacizumab. The plasma concentration–time profiles of rucaparib in combination with bevacizumab suggest no pharmacokinetic interactions between the drugs. The randomized phase II portion of MITO 25 will further investigate rucaparib maintenance treatment with or without bevacizumab in patients with newly diagnosed stage III–IV ovarian cancer who responded to carboplatin-paclitaxel chemotherapy with or without bevacizumab.
Trial Registration
ClinicalTrials.gov identifier NCT03462212; registered March 2018.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Despite recent advances in therapy, ovarian cancer mortality remains high, suggesting additional strategies are needed. |
Our analysis demonstrates the feasibility of combining rucaparib (500 mg twice daily) and bevacizumab (15 mg/kg every 21 days) as treatment for patients with newly diagnosed, advanced ovarian cancer. |
The safety profile of the combination was similar to that reported previously for rucaparib and bevacizumab as single agents. |
1 Background
Mortality in patients with ovarian cancer remains high, with only a modest increase in overall survival despite improvements in treatment. Initial response rates to chemotherapy are approximately 80% [1], but the majority of patients who achieve a complete response will relapse within 4–12 months [2, 3].
Targeted agents, such as the antiangiogenic drugs bevacizumab and cediranib, and the poly(ADP-ribose) polymerase (PARP) inhibitors olaparib, niraparib, and rucaparib, have been used to improve patient outcomes, either as single agents or in combination with chemotherapy in patients with newly diagnosed and recurrent disease in the treatment setting or as switch maintenance [4,5,6,7,8,9].
Bevacizumab is a monoclonal antibody that targets the proangiogenic vascular endothelial growth factor. Trials have demonstrated that the addition of bevacizumab to chemotherapy as first-line treatment and as treatment or maintenance for patients with recurrent ovarian cancer can improve progression-free survival (PFS) relative to chemotherapy alone [8, 9]. This may be due to additional antitumor activity on the tumor vasculature, interstitial pressure, and permeability of blood vessels, which allows enhanced delivery of chemotherapy to tumor cells [10].
PARP inhibitors block the enzymatic activity required to form poly(ADP-ribose) chains, which are crucial for the repair of single-strand breaks in DNA. They also trap PARP enzymes at sites of DNA damage, preventing repair. Olaparib, niraparib, and rucaparib all strongly inhibit the enzymatic activity of PARP1 (IC50, 1.9–0.6 nM) and PARP2 (IC50, 0.2–0.5 nM) [11], and have similar potency for DNA trapping [12, 13]. Notably, the PARP inhibitor talazoparib, which is approved for the treatment of patients with breast cancer, has stronger enzymatic inhibition (IC50, 0.5 and 0.1 nM, respectively) and more potent DNA trapping abilities.
BRCA1 and BRCA2 (BRCA1/2)-mutant cell lines and cells deficient in or depleted of homologous recombination proteins (i.e., having homologous recombination repair deficiency [HRD]) other than BRCA1/2 have sensitivity toward PARP inhibitors [14, 15]. Clinical data confirm preclinical evidence, and PARP inhibitors have been approved in “all comers” with platinum-sensitive recurrent ovarian cancer [16,17,18].
Rucaparib is an orally available, small-molecule PARP inhibitor approved for the treatment of patients with recurrent ovarian cancer either as a single agent or as maintenance treatment in those responding to platinum-based chemotherapy [6, 19]. The recommended starting dose of rucaparib is 600 mg twice daily (BID). In clinical trials, rucaparib was found to be generally well tolerated, with treatment-emergent adverse events (TEAEs) common to the PARP inhibitor class (e.g., fatigue, gastrointestinal events, hematologic events) that could be managed with supportive care or dose modifications [6, 20]. Notably, some TEAEs are more common with certain PARP inhibitors than others, such as a higher incidence of thrombocytopenia and hypertension with niraparib vs olaparib or rucaparib, and a higher incidence of increased alanine/aspartate aminotransferase levels with rucaparib vs olaparib or niraparib [21, 22].
The combination of an antiangiogenic agent and a PARP inhibitor is being studied in a number of clinical trials given the reported synergistic effect of the drugs. Inhibiting angiogenesis leads to hypoxia, which has been shown to induce HRD through the downregulation of homologous recombination repair genes, which may result in increased sensitivity of tumor cells to PARP inhibitors [23,24,25]. The combination of a PARP inhibitor (olaparib capsules 200 mg BID) and an angiogenesis inhibitor (cediranib 30 mg BID) improved PFS by approximately 8 months compared with PARP inhibition alone (olaparib capsules 400 mg BID; hazard ratio = 0.42) in a phase II study of women with platinum-sensitive, relapsed, high-grade ovarian cancer [26]. The combination of niraparib (300 mg daily) and bevacizumab (15 mg/kg day 1 every 21 days [d1 q21d]) significantly improved PFS compared with niraparib 300 mg daily alone (adjusted hazard ratio = 0.35) in patients with recurrent, platinum-sensitive ovarian cancer [27]. Maintenance treatment with olaparib tablets (300 mg BID) combined with bevacizumab (15 mg/kg q21d) improved PFS compared with bevacizumab maintenance alone (hazard ratio = 0.59) in patients with advanced ovarian cancer who had responded to first-line platinum-taxane chemotherapy plus bevacizumab [28]. Across studies, adverse events (AEs) with the combinations were consistent with the known safety profiles of the single agents, although some AEs were more frequent in the combination arms vs the single-agent arms.
Here, we present data from the phase I portion of the MITO 25 study evaluating maintenance treatment with rucaparib with or without bevacizumab in patients with newly diagnosed high-grade epithelial ovarian, fallopian tube, or primary peritoneal cancer. As no data exist for rucaparib when administered concomitantly with bevacizumab, this pharmacokinetic (PK) and dose-escalation portion was designed to determine the maximum tolerated dose (MTD) of rucaparib in this combination, provide early indications of the safety of the combination, and establish the PK profile of rucaparib when administered with bevacizumab. The efficacy of rucaparib maintenance treatment with or without bevacizumab will be further evaluated in the randomized phase II portion of MITO 25.
2 Methods
This is a single-arm, phase I dose-escalation study performed in a single institution. The trial was approved by the Fondazione IRCCS National Cancer Institute of Milan Ethical Committee and registered with ClinicalTrials.gov (NCT03462212).
2.1 Patients and Study Design
Patients provided written informed consent before participating in the study. Patients with newly diagnosed, histologically confirmed, high-grade serous, endometrioid, and clear-cell International Federation of Gynecology and Obstetrics staging system (FIGO) stage IIIB to IV epithelial ovarian cancer, primary peritoneal cancer, or fallopian tube cancer were enrolled. Patients had to have an Eastern Cooperative Oncology Group Performance Status of 0 or 1, and adequate renal, hepatic, and bone marrow function. Patients who received prior anticancer treatment were excluded.
Cohorts of three patients at a time were recruited using the Fibonacci triplets design to assess the effects of increasing doses of rucaparib (400 mg, 500 mg, and 600 mg BID) as a continuous oral administration in combination with bevacizumab at the fixed intravenous dose of 15 mg/kg administered on d1 q21d.
Three patients were recruited into the first cohort (rucaparib 400 mg BID). If no serious side effect (SSE) representing a dose-limiting toxicity (DLT; see criteria below) was reported in the first three patients, the second cohort was treated at the next dose level. If one SSE was reported in the first cohort, three more patients were to be enrolled at the same dose. If no SSEs were reported in these three patients, the second cohort was to be opened and treated as above. If one or more SSEs was reported in the further three enrolled patients, the MTD was identified as the previous rucaparib concentration.
2.2 Objectives
The primary objective was to identify the MTD of the rucaparib-bevacizumab combination in patients with stage IIIB to IV ovarian cancer. Secondary objectives were to evaluate the hematologic and nonhematologic toxicity of the rucaparib-bevacizumab combination and evaluate the PK of rucaparib when co-administered with bevacizumab in patients receiving this combination.
2.3 Dosing Schedule and Dose Escalation
All patients were treated with carboplatin area under the concentration–time curve (AUC) 5 in combination with paclitaxel 175 mg/m2 d1 q21d and bevacizumab 15 mg/kg d1 q21d for six cycles. In the case of interval debulking surgery, bevacizumab was held for ≥ 28 days before and after the surgery; held doses of bevacizumab could be replaced to complete the maximum number of cycles. At chemotherapy completion, non-progressing patients continued to receive intravenous bevacizumab q21d as maintenance for a maximum of 22 total cycles, including the cycles in combination with chemotherapy. Combination with oral rucaparib as maintenance was started within 9 weeks of chemotherapy completion. The first dose of oral rucaparib was given 7 days prior to bevacizumab administration to allow the opportunity to observe any acute drug reactions and to collect rucaparib PK data prior to bevacizumab administration. Oral rucaparib (400 mg, 500 mg, or 600 mg BID depending on cohort) was administered in 28-day cycles. Similar to prior studies [6, 20], patients received rucaparib until disease progression or unacceptable toxicity.
DLTs were assessed in patients receiving the rucaparib-bevacizumab combination. DLTs were defined as follows:
-
More than ten missed doses in the preceding 28 days due to study drug-related toxicity;
-
A delay of more than 14 days in initiating cycle 2 due to study drug-related toxicity;
-
Discontinuation of the patient due to study drug-related toxicity before completing cycle 1;
-
A nonhematologic event, including grade ≥ 3 nausea, vomiting, or diarrhea lasting more than 3 days despite optimal supportive medications; or any other grade ≥ 3 nonhematologic toxicity with the exception of transient (< 7 days), grade 3 transaminase elevation;
-
A hematologic event, including grade 4 neutropenia (absolute neutrophil count < 500/mm3) lasting ≥ 7 days; febrile neutropenia (absolute neutrophil count < 500/mm3 with a fever ≥ 38.5°C); or grade ≥ 3 thrombocytopenia (platelet count < 50,000/mm3) persisting for ≥ 5 days or grade ≥ 3 thrombocytopenia associated with bleeding.
The MTD was defined as the dose level below which no more than one out of three patients or a total of two out of six patients had DLTs. A DLT was defined as the occurrence of one of the above events during the first two cycles of drug administration, which was considered at least possibly related to the study drugs. To further safeguard the well-being of the patients, two patients in each cohort were enrolled in parallel and observed for two cycles of treatment; if no DLT occurred, a third patient was enrolled.
After the MTD was determined, the patients continued treatment until disease progression, unacceptable toxicity, or refusal of further treatment. AEs were graded according to the National Cancer Institute Common Terminology Criteria for Adverse Events, Version 4.03.
2.4 Pharmacokinetic Sampling and Analysis
Blood samples for the rucaparib PK analysis were drawn from each patient during cycle 1 on day −7 (acute administration), day 1 (bevacizumab infusion), and day 21 and at 1, 2, 3, 4, 6, 8, and 24 hours post-dose. Plasma concentrations were determined using a validated high-performance liquid chromatography method combined with mass spectrometry, which was performed with a minor modification from the method used by Sparidans et al. [29].
Pharmacokinetic parameters were calculated from the concentration–time data using a noncompartmental analysis. Rucaparib parameters obtained on days 1 and 21 were compared with those obtained on day −7 to compare the steady-state condition of rucaparib after bevacizumab infusion with that of rucaparib prior to bevacizumab coadministration. The rucaparib PK parameters were also compared to what was reported in the investigator brochure of the drug referring to historical controls.
The following parameters were obtained for rucaparib: maximum plasma concentration (Cmax) at steady state, minimal plasma concentration at steady state, and AUC at steady state. Cmax, time to Cmax (Tmax), and AUC from 0 to 8 hours were determined at the first administration on day − 7.
2.5 Statistical Analysis
Descriptive statistics were calculated for the PK parameters: mean, standard deviation, coefficient of variation, median, and geometric mean using SAS, Version 9.3.
3 Results
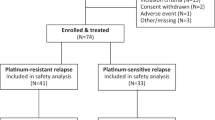
We enrolled nine patients, three in each dose cohort, from April 2018 to March 2019. Patient baseline demographics and disease characteristics for each dose subgroup are reported in Table 1.
3.1 Safety
The AEs experienced by patients in each dose group are summarized in Table 2. Patients in all groups had arthralgia and nausea, whereas hypertension, dysgeusia, and diarrhea became more common in the higher dosage groups. The majority of AEs were grade 1 or 2, and were thought to be related to rucaparib or bevacizumab.
Two patients in the 600-mg group had four grade 3 TEAEs: one patient had grade 3 increased alanine aminotransferase and aspartate aminotransferase levels lasting 10 days and another patient had grade 3 depression and hallucinations.
3.2 Maximum Tolerated Dose
No DLTs occurred in the rucaparib 400- or 500-mg dose groups. The alanine aminotransferase elevation and the depression and hallucination events were considered DLTs related to rucaparib. Alanine aminotransferase elevations have been reported in trials of patients receiving rucaparib for recurrent disease, and depression has been reported with other PARP inhibitors. Although hallucinations were never reported, given the complete resolution of the symptoms after rucaparib discontinuation, we concluded that were rucaparib related. Because both of these SSEs occurred in the 600-mg group and affected two out of three patients, the MTD for rucaparib in combination with bevacizumab 15 mg/kg d1 q21d was identified to be 500 mg BID (i.e., the dose level below the group in which the DLTs occurred).
3.3 Pharmacokinetics
Table 3 summarizes the mean PK data over time for rucaparib at the three dose levels, administered alone and in combination with bevacizumab. Despite the clear limitations represented by the small sample size, the narrow dose range, and the high PK variability, plasma exposure of rucaparib was approximately dose proportional. The values of Tmax ranged from 1.7 to 5 hours, suggesting a relatively fast absorption. The range of trough concentrations (i.e., the lowest concentration before the next dose was administered) was 1.5–1.6, 1.8–2.0, and 1.6–2.1 μg/mL at doses of 400, 500, and 600 mg BID, respectively. Rucaparib reached steady-state levels on days 1 and 21, with the Cmax and AUC being two to three times higher than those determined on day −7.
Figure 1 shows the mean concentration–time profiles of patients treated with the three doses, and Fig. 2 compares the concentration–time profiles for the three groups at the three timepoints. No substantial difference in PK parameters was found between the three-dose cohorts or in the PK profiles of rucaparib when administered prior to or concomitantly with bevacizumab with respect to historical controls as reported in the rucaparib prescribing information.
4 Discussion
This phase I dose-escalation study evaluated the use of rucaparib and bevacizumab as maintenance treatment in patients with newly diagnosed, FIGO stage IIIB–IV ovarian, primary peritoneal, or fallopian tube cancer who had responded to carboplatin/paclitaxel chemotherapy plus bevacizumab. The MTD of rucaparib was 500 mg BID when co-administered with bevacizumab 15 mg/kg d1 q21d. There were no new safety concerns arising from the use of the combination of rucaparib and bevacizumab in these patients. The plasma–concentration time profiles of rucaparib administered with bevacizumab were similar to those of rucaparib as a single agent reported historically. The randomized phase II portion of MITO 25 will expand evaluation of maintenance treatment with rucaparib in combination with bevacizumab in patients with chemotherapy-naïve, advanced ovarian cancer.
The phase I portion of MITO 25 utilized a standard Fibonacci triplets design to evaluate the combination. Two patients in the rucaparib 600-mg group had DLTs, including a grade 3 transaminases elevation lasting more than 7 days and a grade 3 neurological event. Per protocol, the next lower dose (500 mg BID) was declared the MTD when taken in combination with the bevacizumab dose of 15 mg/kg d1 q21d. A grade 3 alanine aminotransferase/aspartate aminotransferase increase is a known side effect of rucaparib and can be managed according to the summary of product characteristics [19].
Depression has been reported with other PARP inhibitors but not with rucaparib, nor were hallucinations. Nevertheless, the two symptoms were considered treatment related as the patient had no prior history of depression or hallucinations and rucaparib was the only new treatment added to the long-lasting therapy of the patient. Furthermore, these symptoms completely disappeared after rucaparib discontinuation.
The overall safety profile was similar to that reported in previous studies of single-agent rucaparib and single-agent bevacizumab [6, 8, 9, 20, 30, 31]. The most frequent bevacizumab-related AE was hypertension as reported in the registration trial [8]. In the phase III ARIEL3 study, patients were treated with rucaparib 600 mg BID as a single agent [6]. The most common TEAEs were nausea, asthenia or fatigue, dysgeusia, anemia or decrease hemoglobin, constipation, and vomiting. Grade 3 or higher TEAEs were reported in 56% of patients taking rucaparib, the most common of which were anemia (19%), and increased alanine aminotransferase or aspartate aminotransferase levels (11%). In ARIEL3, a dose reduction due to a TEAE occurred in 55% of patients in the rucaparib group; therefore, it is not surprising that a lower dosage would be recommended when rucaparib is taken in combination with another agent [6]. A similar safety profile was also reported for patients in the phase II ARIEL2 study [31]. TEAEs observed in our phase I portion of MITO 25 were also generally similar to those reported in other studies evaluating PARP inhibitors in combination with bevacizumab [27, 28]. Across those studies, the most common any-grade TEAEs in the combination arms were nausea, fatigue, hypertension, and anemia. The combination arms generally had higher incidence of grade 3 or greater TEAEs, with the most common being hypertension and anemia.
At the three dose levels investigated, rucaparib exhibited dose-related plasma concentration–time profiles in line with those observed after repeated administration of the agent given on its own, with the accumulation of the drug two to three times that of the concentration obtained after acute administration (day −7). In the patients studied, there were no substantial differences in the PK profiles of rucaparib when it was administered alone or concomitantly with bevacizumab. In addition, the PK parameters were consistent with those reported in earlier studies on the PK of rucaparib administered as a single agent [30, 32].
The combination of bevacizumab 15 mg/kg d1 q21d plus rucaparib 500 mg BID will be used in the multicenter phase II portion of MITO 25 in patients with newly diagnosed, high-grade epithelial ovarian, fallopian tube, or primary peritoneal cancer. Patients with HRD-negative tumors will be randomized (1:1:1) to one of three arms: carboplatin-paclitaxel chemotherapy plus bevacizumab followed by bevacizumab-only maintenance treatment (Arm A), carboplatin-paclitaxel chemotherapy followed by rucaparib-only maintenance treatment (Arm B), or carboplatin-paclitaxel chemotherapy plus bevacizumab followed by bevacizumab plus rucaparib maintenance treatment (Arm C). Patients with HRD-positive tumors will be randomized (1:1) to either Arm B or Arm C. The primary endpoint of phase II is PFS, and secondary endpoints include overall survival, response rate, time to subsequent therapy, safety and tolerability, and quality of life. The investigators will enroll 290 patients; recruiting will begin in the third quarter of 2020 and the trial is expected to run for approximately 5 years.
References
Bookman MA. Developmental chemotherapy and management of recurrent ovarian cancer. J Clin Oncol. 2003;21:149s–67s. https://doi.org/10.1200/jco.2003.02.553.
Harries M, Gore M. Part I: chemotherapy for epithelial ovarian cancer-treatment at first diagnosis. Lancet Oncol. 2002;3:529–36. https://doi.org/10.1016/s1470-2045(02)00846-x.
Cannistra SA. Cancer of the ovary. N Engl J Med. 2004;351:2519–29. https://doi.org/10.1056/NEJMra041842.
Ledermann J, Harter P, Gourley C, Friedlander M, Vergote I, Rustin G, et al. Olaparib maintenance therapy in platinum-sensitive relapsed ovarian cancer. N Engl J Med. 2012;366:1382–92. https://doi.org/10.1056/NEJMoa1105535.
Mirza MR, Monk BJ, Herrstedt J, Oza AM, Mahner S, Redondo A, et al. Niraparib maintenance therapy in platinum-sensitive, recurrent ovarian cancer. N Engl J Med. 2016;375:2154–64. https://doi.org/10.1056/NEJMoa1611310.
Coleman RL, Oza AM, Lorusso D, Aghajanian C, Oaknin A, Dean A, et al. Rucaparib maintenance treatment for recurrent ovarian carcinoma after response to platinum therapy (ARIEL3): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet. 2017;390:1949–61. https://doi.org/10.1016/s0140-6736(17)32440-6.
Pujade-Lauraine E, Ledermann JA, Selle F, Gebski V, Penson RT, Oza AM, et al. Olaparib tablets as maintenance therapy in patients with platinum-sensitive, relapsed ovarian cancer and a BRCA1/2 mutation (SOLO2/ENGOT-Ov21): a double-blind, randomised, placebo-controlled, phase 3 trial. Lancet Oncol. 2017;18:1274–84. https://doi.org/10.1016/s1470-2045(17)30469-2.
Coleman RL, Brady MF, Herzog TJ, Sabbatini P, Armstrong DK, Walker JL, et al. Bevacizumab and paclitaxel-carboplatin chemotherapy and secondary cytoreduction in recurrent, platinum-sensitive ovarian cancer (NRG Oncology/Gynecologic Oncology Group study GOG-0213): a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2017;18:779–91. https://doi.org/10.1016/S1470-2045(17)30279-6.
Aghajanian C, Goff B, Nycum LR, Wang YV, Husain A, Blank SV. Final overall survival and safety analysis of OCEANS, a phase 3 trial of chemotherapy with or without bevacizumab in patients with platinum-sensitive recurrent ovarian cancer. Gynecol Oncol. 2015;139:10–6. https://doi.org/10.1016/j.ygyno.2015.08.004.
Jain RK. Normalizing tumor vasculature with anti-angiogenic therapy: a new paradigm for combination therapy. Nat Med. 2001;7:987–9. https://doi.org/10.1038/nm0901-987.
Robillard L, Nguyen M, Harding TC, Simmons AD. In vitro and in vivo assessment of the mechanism of action of the PARP inhibitor rucaparib. Cancer Res. 2017;77:abstract 2475.
Murai J, Huang SY, Das BB, Renaud A, Zhang Y, Doroshow JH, et al. Trapping of PARP1 and PARP2 by clinical PARP inhibitors. Cancer Res. 2012;72:5588–99. https://doi.org/10.1158/0008-5472.CAN-12-2753.
Murai J, Huang SY, Renaud A, Zhang Y, Ji J, Takeda S, et al. Stereospecific PARP trapping by BMN 673 and comparison with olaparib and rucaparib. Mol Cancer Ther. 2014;13:433–43. https://doi.org/10.1158/1535-7163.MCT-13-0803.
Bryant HE, Schultz N, Thomas HD, Parker KM, Flower D, Lopez E, et al. Specific killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) polymerase. Nature. 2005;434:913–7. https://doi.org/10.1038/nature03443.
McCabe N, Turner NC, Lord CJ, Kluzek K, Białkowska A, Swift S, et al. Deficiency in the repair of DNA damage by homologous recombination and sensitivity to poly(ADP-ribose) polymerase inhibition. Cancer Res. 2006;66:8109–15. https://doi.org/10.1158/0008-5472.can-06-0140.
Lorusso D, Tripodi E, Maltese G, Lepori S, Sabatucci I, Bogani G, et al. Spotlight on olaparib in the treatment of BRCA-mutated ovarian cancer: design, development and place in therapy. Drug Des Devel Ther. 2018;12:1501–9. https://doi.org/10.2147/DDDT.S124447.
Sabatucci I, Lorusso D. The role of niraparib in the treatment of ovarian cancer: actuality and perspectives [in Italian]. Recenti Prog Med. 2017;108:265–8. https://doi.org/10.1701/2715.27713.
Sabatucci I, Maltese G, Lepori S, Tripodi E, Bogani G, Lorusso D. Rucaparib: a new treatment option for ovarian cancer. Expert Opin Pharmacother. 2018;19:765–71. https://doi.org/10.1080/14656566.2018.1464557.
Rubraca (rucaparib) tablets [summary of product characteristics]. Swords, Ireland: Clovis Oncology Ireland Ltd.; 2019.
Kristeleit RS, Oaknin A, Ray-Coquard I, Leary A, Balmana J, Drew Y, et al. Antitumor activity of the poly(ADP-ribose) polymerase inhibitor rucaparib as monotherapy in patients with platinum-sensitive, relapsed, BRCA-mutated, high-grade ovarian cancer, and an update on safety. Int J Gynecol Cancer. 2019;29:1396–404. https://doi.org/10.1136/ijgc-2019-000623.
Ray-Coquard I, Mirza MR, Pignata S, Walther A, Romero I, du Bois A. Therapeutic options following second-line platinum-based chemotherapy in patients with recurrent ovarian cancer: comparison of active surveillance and maintenance treatment. Cancer Treat Rev. 2020;90:102107. https://doi.org/10.1016/j.ctrv.2020.102107.
LaFargue CJ, Dal Molin GZ, Sood AK, Coleman RL. Exploring and comparing adverse events between PARP inhibitors. Lancet Oncol. 2019;20:e15-28. https://doi.org/10.1016/S1470-2045(18)30786-1.
Bindra RS, Gibson SL, Meng A, Westermark U, Jasin M, Pierce AJ, et al. Hypoxia-induced down-regulation of BRCA1 expression by E2Fs. Cancer Res. 2005;65:11597–604. https://doi.org/10.1158/0008-5472.CAN-05-2119.
Bindra RS, Schaffer PJ, Meng A, Woo J, Maseide K, Roth ME, et al. Down-regulation of Rad51 and decreased homologous recombination in hypoxic cancer cells. Mol Cell Biol. 2004;24:8504–18. https://doi.org/10.1128/MCB.24.19.8504-8518.2004.
Mirza MR, Pignata S, Ledermann JA. Latest clinical evidence and further development of PARP inhibitors in ovarian cancer. Ann Oncol. 2018;29:1366–76. https://doi.org/10.1093/annonc/mdy174.
Liu JF, Barry WT, Birrer M, Lee J-M, Buckanovich RJ, Fleming GF, et al. Combination cediranib and olaparib versus olaparib alone for women with recurrent platinum-sensitive ovarian cancer: a randomised phase 2 study. Lancet Oncol. 2014;15:1207–14. https://doi.org/10.1016/S1470-2045(14)70391-2.
Mirza MR, Bergmann TK, Mau-Sorensen M, Christensen RD, Avall-Lundqvist E, Birrer MJ, et al. A phase I study of the PARP inhibitor niraparib in combination with bevacizumab in platinum-sensitive epithelial ovarian cancer: NSGO AVANOVA1/ENGOT-OV24. Cancer Chemother Pharmacol. 2019;84:791–8. https://doi.org/10.1007/s00280-019-03917-z.
Ray-Coquard I, Pautier P, Pignata S, Pérol D, González-Martín A, Berger R, et al. Olaparib plus bevacizumab as first-line maintenance in ovarian cancer. N Engl J Med. 2019;381:2416–28. https://doi.org/10.1056/NEJMoa1911361.
Sparidans RW, Durmus S, Schinkel AH, Schellens JH, Beijnen JH. Liquid chromatography-tandem mass spectrometric assay for the PARP inhibitor rucaparib in plasma. J Pharm Biomed Anal. 2014;88:626–9. https://doi.org/10.1016/j.jpba.2013.10.016.
Kristeleit R, Shapiro GI, Burris HA, Oza AM, LoRusso P, Patel MR, et al. A phase I-II study of the oral PARP inhibitor rucaparib in patients with germline BRCA1/2-mutated ovarian carcinoma or other solid tumors. Clin Cancer Res. 2017;23:4095–106. https://doi.org/10.1158/1078-0432.CCR-16-2796.
Swisher EM, Lin KK, Oza AM, Scott CL, Giordano H, Sun J, et al. Rucaparib in relapsed, platinum-sensitive high-grade ovarian carcinoma (ARIEL2 Part 1): an international, multicentre, open-label, phase 2 trial. Lancet Oncol. 2017;18:75–87. https://doi.org/10.1016/S1470-2045(16)30559-9.
Shapiro GI, Kristeleit R, Burris HA, LoRusso P, Patel MR, Drew Y, et al. Pharmacokinetic study of rucaparib in patients with advanced solid tumors. Clin Pharmacol Drug Dev. 2019;8:107–18. https://doi.org/10.1002/cpdd.575.
Acknowledgments
Editorial support funded by Clovis Oncology was provided by Nathan Yardley and Frederique H. Evans of Ashfield Healthcare Communications (Middletown, CT, USA).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
Open access funding provided by Università Cattolica del Sacro Cuore within the CRUI-CARE Agreement. Clovis Oncology supported the trial with financial support for PK evaluation and editorial support, and by providing rucaparib free of charge.
Conflict of Interest
Domenica Lorusso has served in a consulting or advisory role for Clovis Oncology, Amgen, AstraZeneca, ImmunoGen, Genmab, Merck, PharmaMar, Roche, Takeda, and Tesaro; received support for travel or accommodation from AstraZeneca, PharmaMar, Roche, and Tesaro; has served as a principal investigator of trials for Clovis Oncology, AstraZeneca, Immunogen, Genmab, Merck, PharmaMar, Roche, and Tesaro; and her institution has received research grants from Clovis Oncology, Merck, PharmaMar, Roche, and Tesaro. Maurizio D’Incalci has served in a consulting or advisory role for Tesaro and PharmaMar. Filippo de Braud has served in a consulting or advisory role for Regione Toscana and Servier; received support for travel or accommodation from Amgen, BMS, Celgene, and Roche; received fees for review activities such as data monitoring boards from BMS, Daiichi Sankyo, EMD Serono, Incyte, Ignyta, Nerviano Medical Science (NMS), OCTIMET Oncology, Pfizer, Pharma Research Associates; Pierre Fabre, Roche, Sanofi, and Teofarma; and reports other support (e.g., writing assistance, administrative support) from AccuMed, Bayer, Biotechspert, BMS, Celgene, Dephaforum, Healthcare Research & Pharmacoepidemiology, Ignyta, Loxo Oncology, Merck, MSD, Pfizer, prIME Oncology, Roche, Sanofi, and Servier. Giuseppa Maltese, Ilaria Sabatucci, Sara Cresta, Cristina Matteo, Tommaso Ceruti, , Massimo Zucchetti, Francesco Raspagliesi, Cristina Sonetto, Valentina Sinno, Dominique Ronzulli, and Serena Giolitto have no conflicts of interest that are directly relevant to the content of this article.
Ethics Approval
The trial was approved by the Fondazione IRCCS National Cancer Institute of Milan Ethical Committee.
Consent to Participate
Patients provided written informed consent before participating in the study.
Consent for Publication
Not applicable.
Availability of Data and Material
Further data are available from the corresponding author upon request.
Code Availability
Not applicable.
Authors’ Contributions
DL designed the study. GM, IS, SC, FR, CS, VS, DR, and SG collected the data. DL, CM, TC, MD, MZ, and FdB analyzed the data. All authors contributed to the interpretation of the data and critically revised the manuscript for important intellectual content. All authors provided final approval of the manuscript and agreed to be accountable for the accuracy and integrity of this work.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lorusso, D., Maltese, G., Sabatucci, I. et al. Phase I Study of Rucaparib in Combination with Bevacizumab in Ovarian Cancer Patients: Maximum Tolerated Dose and Pharmacokinetic Profile. Targ Oncol 16, 59–68 (2021). https://doi.org/10.1007/s11523-020-00780-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11523-020-00780-4