Abstract
Intra-arterial blood pressure measurement is the cornerstone of hemodynamic monitoring in intensive care units (ICU). Accuracy of the measurement is dependent on the dynamic response of the measuring system, defined by its natural frequency (fnatural) and damping coefficient (Zdamping). Gardner’s plot (1981) has long been the only way to determine the accuracy of the pressure measurement. Specific objectives: (i) estimation of the amplitude of error in pressure measurement through simulations based on real-world data, (ii) a novel method to correct the error. Simulated blood pressure waveforms of various heart rates were passed through simulated measurement systems with varying fnatural and Zdamping. The numerical errors in systolic and diastolic pressures and mean error in the measured pressure were used to generate heat maps for the various recording conditions, in the same plot as that by Gardner (1981). fnatural and Zdamping from 121 patient recordings are plotted on these heat maps to demonstrate the fraction of unacceptable recordings. Performance of a tunable filter to correct the error is demonstrated. In many clinical settings, the measurement of intra-arterial pressure is prone to significant error. The proposed tunable filter is shown to improve the accuracy of intra-arterial pressure recording.
Graphic Abstract




















Similar content being viewed by others
Abbreviations
- bpm:
-
Beats per minute
- ICU:
-
Intensive care unit
References
Chambers D, Huang C, Matthews G (2019) Arterial pressure waveforms. In Basic Physiology for Anaesthetists (pp. 155–157). Cambridge: Cambridge University Press. doi:https://doi.org/10.1017/9781108565011.038
Denardo SJ, Nandyala, Freeman GL, Pierce GL, Nichols WW (2010) Pulse wave analysis of the aortic pressure waveform in severe left ventricular systolic dysfunction. Circ Heart Fail, pp.149–156. DOI: https://doi.org/10.1161/CIRCHEARTFAILURE.109.862383.
Devasahayam S (2019) Signals and systems in biomedical engineering: physiological systems modeling and signal processing, 3rd Edition, Springer. DOI: https://doi.org/10.1007/978-981-13-3531-0
Hall JE (2016) Guyton and Hall textbook of medical physiology. Elsevier
RM Gardner 1981 Direct blood pressure measurement: dynamic response requirement Anesthesiology 54 227 236 https://doi.org/10.1097/00000542-198103000-00010
J Grensemann 2018 Cardiac output monitoring by pulse contour analysis, the technical basics of less-invasive techniques Frontiers in Medicine 5 64 https://doi.org/10.3389/fmed.2018.00064
B Kleinman S Powell P Kumar RM Gardner 1992 The fast flush test measures the dynamic response of the entire blood pressure monitoring system Anesthesiology 77 1215 1220 https://doi.org/10.1097/00000542-199212000-00024
B Lami D Chemla C Richard J-L Teboul 2005 Clinical review: interpretation of arterial pressure wave in shock states Crit Care 9 601 606 https://doi.org/10.1186/cc3891
Mahesh Nirmalan Paul M Dark 2014 Broader applications of arterial pressure wave form analysis Continuing Education in Anaesthesia, Critical Care & Pain 14 6 https://doi.org/10.1093/bjaceaccp/mkt078
Mathieu Jozwiak Xavier Monnet Jean-Louis Teboul 2018 Pressure waveform analysis Anesthesia and Analgesia 126 6 https://doi.org/10.1213/ANE.0000000000002527
H Oh SH Choe YJ Kim 2021 Intraarterial catheter diameter and dynamic response of arterial pressure monitoring system: a randomized controlled trial J Clin Monit Comput 2021 1 9 https://doi.org/10.1007/S10877-021-00663-7
M Reed 1990 Gardner, Direct arterial pressure monitoring Curr Anaesth Crit Care 1 4 239 246 https://doi.org/10.1016/0953-7112(90)90008
S Romagnoli SM Romano S Bevilacqua 2011 Dynamic response of liquid-filled catheter systems for measurement of blood pressure: precision of measurements and reliability of the Pressure Recording Analytical Method with different disposable systems J Crit Care 26 415 422 https://doi.org/10.1016/J.JCRC.2010.08.010
S Romagnoli Z Ricci D Quattrone L Tofani O Tujjar G Villa 2014 Salvatore M Romano and A Raffaele De Gaudio, Accuracy of invasive arterial pressure monitoring in cardiovascular patients: an observational study Crit Care 18 644 https://doi.org/10.1186/s13054-014-0644-4
WH Rook JD Turner TH Clutton-Brock 2017 Analysis of damping characteristics of arterial catheter blood pressure monitoring in a large intensive care unit South African J Crit Care 33 8 10
C Slagt I Malagon ABJ Groeneveld 2014 Systematic review of uncalibrated arterial pressure waveform analysis to determine cardiac output and stroke volume variation Br J Anaesth 112 4 626 637 https://doi.org/10.1093/bja/aet429
B Saugel K Kouz AS Meidert 2020 (2020) How to measure blood pressure using an arterial catheter: a systematic 5-step approach Crit Care 241 24 1 10 https://doi.org/10.1186/S13054-020-02859-W
JG Webster 2006 Encyclopedia of medical devices and instrumentation Wiley-Interscience Hoboken
Acknowledgements
The authors thank the medical and technical personnel at the Surgical Intensive Care Unit of Christian Medical College, Vellore, for enabling the blood pressure recordings. Ms. Hamsavardhini,V, Ms. Kamatham Shiny Simon, and Ms. Anushka Kataria (second year medical students) are thanked for the assistance in data collection.
Funding
The study was funded by Department of Biotechnology (DBT), Government of India.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the Institutional Review Board of Christian Medical College Vellore, India (IRB Min. No: 10859 dated 27/09/2017 and 12173 dated 06/08/2019).
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The article was deposited as preprint: Suresh Devasahayam, Naveen Gangadharan, C Surekha, Bowya Baskaran, Farhan Adam Mukadam, Sathya Subramani. “Intra-Arterial Blood Pressure Measurement: Sources of Error and Solutions,” https://www.medrxiv.org/content/10.1101/2020.08.29.20184275v2
Appendix
Appendix
1.1 Blood pressure waveform
The arterial pressure waveform can be simulated compactly by Fourier synthesis, with at least 20 sinusoids with magnitude, \({M}_{k}\), and phase, \({\phi }_{k}\): \(P(t)={P}_{d}+({P}_{s}-{P}_{d})\sum_{k=0}^{20}{M}_{k}\mathrm{cos}(2\pi k{f}_{o}t-{\phi }_{k})\). fo = (heart rate in beats/min)/60, Ps= systolic pressure, and Pd = diastolic pressure.
k | 0 | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | 19 | 20 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
\({M}_{k}\) | 0.4486 | 0.365 | 0.1825 | 0.1194 | 0.0567 | 0.0294 | 0.0448 | 0.0277 | 0.0117 | 0.0208 | 0.0172 | 0.0064 | 0.0112 | 0.0124 | 0.0044 | 0.0066 | 0.0074 | 0.0054 | 0.0023 | 0.0045 | 0.0030 |
\({\phi }_{k}\) | 0.0 | 3.169 | 5.034 | 0.709 | 2.8 | 3.843 | 5.445 | 1.378 | 2.712 | 4.061 | 6.142 | 1.6 | 2.7 | 4.831 | 0.453 | 1.307 | 3.522 | 5.61 | 5.73 | 1.197 | 4.0 |
1.2 Calculation of catheter system characteristics from physical properties
The effective resistance, R, capacitance, C, and inductance (inertance), L, of the system and the natural frequency, fn, and damping coefficient, ζ, are calculated using the equations given below. The total capacitance depends on the compliance of the diaphragm, the compliance of the catheter, and the isothermal compression of the air bubbles trapped in the fluid.
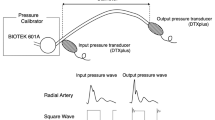
1.3 Calculation of catheter system characteristics from fast-flush test
Measuring the time, tn, and amplitude swing, yn, (deviation from the mean arterial pressure) of the nth maximum, the natural frequency and damping coefficient can be calculated as follows:
1.4 Definition of waveform errors
-
(a)
Mean error: \({e}_{mean}=\frac{1}{T}\underset{0}{\overset{T}{\int }}[{P}_{m}(t)-{P}_{i}(t-\tau )]dt\), T = cardiac cycle duration,\(\tau\)= time shift to compensate for phase lag of the measurement system (i.e., shift at which the mean error is minimum)
-
(b)
Systolic error, \({e}_{s}=max[{P}_{m}(t)]-max[{P}_{i}(t)]\)
-
(c)
Diastolic error, \({e}_{d}=min[{P}_{m}(t)]-min[{P}_{i}(t)]\)
(subscript “m” is for the measured waveform and subscript “i” for the true waveform).
Rights and permissions
About this article
Cite this article
Devasahayam, S., Gangadharan, N., Surekha, C. et al. Intra-arterial blood pressure measurement: sources of error and solutions. Med Biol Eng Comput 60, 1123–1138 (2022). https://doi.org/10.1007/s11517-022-02509-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-022-02509-z