Abstract
Individuals with physical disabilities (PD) face many quality of life challenges. In this study, a randomized controlled trial was conducted to investigate the impact of mindfulness-based intervention (MBI) on the psychological morbidity (indexed by depression and anxiety), emotional well-being (indexed by mindfulness and self-compassion), and health-related quality of life (QOL) among individuals with PD in China. A total of 512 participants with PD were randomly allocated to either the MBI group or the control group. Participants in the experimental group received an eight-week MBI in four sequential stages with different mindfulness meditation exercises. Results showed that participants who underwent MBI exhibited significantly fewer symptoms of depression and anxiety, elevated levels of mindfulness and self-compassion, and enhanced health-related QOL compared to those who did not receive the treatment after intervention. The study yielded promising results for using MBI in promoting the well-being of individuals with PD in China. Suggestions for future research are also highlighted.
Similar content being viewed by others
Introduction
Based on official Chinese government official statistics, individuals with disabilities in China surpassed 85 million. There were over 24 million of people with physical disabilities (PD), representing the dominant category within the different types of disability (Second National Sample Survey Office for Persons with Disabilities, 2008). This category includes individuals experiencing muscular dystrophy, amputations, stroke, multiple sclerosis, cerebral palsy, spinal cord injuries, and/or infectious diseases. Notably, these conditions transcend mere physical mobility limitations because they result in psychological distress and broader health risks. The impact of PD on individuals extends beyond the realm of impaired physical functioning to encompass multifaceted impairment in the areas of psychological morbidity, emotional well-being, and health-related quality of life (QOL). Thus, it is necessary to design effective and innovative interventions based on the specific rehabilitation needs of individuals with ID (Huang et al., 2017; Lebrasseur et al., 2021). It is worth noting that COVID-19 pandemic has had a profound effect on the holistic well-being and QOL of the general populations (Shek, 2021; Shek et al., 2023). Against the backdrop of the COVID-19 pandemic, individuals with PD in China, who have endured prolonged city lockdown measures, are likely to encounter increasingly formidable impediments to their health and well-being, owing to constrained avenues for medical intervention and routine caregiving (Wang et al., 2022; Zhang & Chen, 2021). Increased loneliness, heightened stress levels, elevated perception of risk, diminished resilience, and compromised social coping mechanisms are among the observed risks to mental health and QOL within this group (Na & Yang, 2022). Therefore, there is an urgent need to explore methods and strategies for improving the QOL of individuals with PD, both in academia and in practice.
Over the past few years, clinical practitioners have attempted to promote the QOL and well-being of individuals with physical functioning impairment by undertaking a variety of measures, such as implementing different psychological intervention strategies (Anderson & Ozakinci, 2018; Hardison & Roll, 2016; Hickey et al., 2019; McCracken et al., 2007). Among these interventions, Mindfulness-Based Intervention (MBI) is considered as a potentially effective approach for helping individuals with PD.The theoretical basis of mindfulness originates from the philosophy of ancient Buddhist and is deeply influenced by its centuries-old practice of meditation, which emphasizes the regulation of attention and non-reactive awareness. The idea of mindfulness was embraced by Western psychology through the transformative work of Jon Kabat-Zinn. He refined mindfulness methods so that the “secular” mindfulness practices could be used extensively by the public (Kabat-Zinn, 2003; Tirch et al., 2015).
Kabat-Zinn’s outstanding contribution lies in his introduction of mindfulness into mainstream practice, laying the foundation for the development of this field (Reibel & McCrown, 2019). In the current context, MBI has developed into a structured psychotherapy system that integrates mindfulness meditation, yoga, and cognitive behavioral techniques (Apolinário-Hagen et al., 2020; Pascoe et al., 2017; Shelov et al., 2009; Wielgosz et al., 2019). The core goal of MBI is to cultivate individual self-awareness, regulate emotions, and establish adaptive coping mechanisms, thereby stimulating the individual's inner potential for change. The essence of mindfulness lies in non-judgmental awareness of the present moment, which encompasses the observation and acceptance of emotions, experiences, thoughts and body sensations. These skills are developed progressively through formal meditative practices such as mindfulness and breath awareness, as well as informal daily practices such as open monitoring of daily activities (Mace, 2007; Plaza et al., 2013; Wahbeh & Oken, 2016).
Bishop et al. (2004) suggested that the core dimensions of MBI should consist of self-regulated attention and unique experience orientation. Self-regulation requires careful observation and recognition of thoughts, feelings, and perceptions, while an experiential orientation emphasizes curiosity, openness, and a nonjudgmental attitude. The goal of MBI is to reshape one’s internal experience, promote his/her objective observation, and, over time, deepen his/her insight into habitual thought patterns. Accroding to Shapiro et al. (2006), mindfulness comprises three main components which are attention, intention and attitude. Based on this, Hölzel et al. (2011) developed a more comprehensive theoretical framework for analyzing the interaction mechanism of MBI. This theoretical framework explains in detail how mindfulness works while identifying the important roles of body awareness, attention regulation, emotion regulation (including exposure, reappraisal, extinction, and reconsolidation), and fundamental changes in the mindful self-perspective. It also seeks to demonstrate the potential benefits of MBI in having a transformative impact on an individual's cognitive and affective processes.
The effectiveness of MBI in improving the health and well-being of a variety of populations (including individuals suffering from stress, anxiety, cancer, and chronic diseases) has been confirmed by several studies (Grossman et al., 2004; Hofmann et al., 2010; Ledesma & Kumano, 2009; Merkes, 2010; Zhang et al., 2016a, 2016b). In the context of people with PD, MBI offers promising ways to help improve mental well-being. These practices encourage accepting physical limitations and building resilience, which can help reduce the negative psychological effects often linked with PD (Battalio et al., 2020). Additionally, through techniques like body scan meditations and mindful movement, individuals with PD can become more aware of their body sensations and feel more in control of their physical experiences (Goodrich et al., 2015). Moreover, fostering mindfulness might contribute to improved pain management, reduced stress reactivity, and enhanced emotional regulation, which are especially relevant for individuals dealing with PD (Liu et al., 2022; Reiner, et al., 2013). Despite that MBI may result in positive outcomes for patients with PD, research in this area remains woefully inadequate. In the process of seeking relevant evidence, we found that some studies have proven the significant effectiveness of MBI in reducing psychological morbidity in patients with physical diseases. For example, existing research has shown that individuals diagnosed with stroke (Beauchamp et al., 2023; Niu et al., 2022) and rheumatoid arthritis (Pradhan et al., 2007) significantly reduced their depressive symptoms after receiving MBI. A single study of patients with traumatic lower limb amputation proposes that mindfulness-related yoga programs can effectively decrease the anxiety levels (Mir et al., 2023). A systematic review conducted by Hearn and Cross (2020) showed that MBI was a recommended program for reducing the symptoms of both depression and anxiety in patients with spinal cord injury.
The prominent effects of MBI on improving other aspects of emotional well-being in individuals with physical diseases are also discussed. Pradhan et al. (2007) conducted a study on the effectiveness of a mindfulness-based stress reduction (MBSR) program among 63 patients with rheumatoid arthritis and found that their mindfulness levels improved significantly after the program. Similarly, another qualitative study on the effectiveness of online mindfulness intervention showed that patients with rheumatoid arthritis could develop better understanding and acceptance of mindfulness and learn more mindfulness skills through the practice of MBI (Leov, 2016). A number of systematic reviews suggested that self-compassion of people with chronic poor physical health could be enhanced via a series of mindfulness-related intervention strategies, such as MBSR, mindfulness meditation (MM), -body bridging (MBB)), Yoga and Mindful Self-Compassion Program (MSC). (Friis et al., 2016; Kılıç et al., 2021; Nakamura et al., 2013; Schellekens et al., 2017; Toise et al., 2014). MBSR has been confirmed its effectiveness in increasing levels of self-compassion in people with multiple sclerosis or acquired brain injury as well (Johansson et al., 2015; Simpson et al., 2017). Additionally, the effectiveness of MBI in improving health-related QOL is supported by some existing research evidence (Banth & Ardebil, 2015; Morone et al., 2016; Wong et al., 2011).
A survey of the literature shows that there are limited studies on the effect of mindfulness interventions on individuals with physical functional impairment. When we searched PsycINFO using “physical disability” and “mindfulness” on December 19, 2023, we found 245 citations only. If we add “Chinese” as a search term, the number dropped to 3. Similar observation was found using three Chinese databases (CNKI, Wanfang, and VIP), showing that studies on the effectiveness of MBI in Chinese people are highly inadequate.
With reference to mindfulness interventions in medical and healthcare fields, MBI was predominantly administered in offline settings, with implementation periods ranging from 2 to 8 weeks. Besides, the outcomes primarily revolved around the modulation of negative emotions, demonstrating a alleviation of symptoms related to depression and anxiety (Cui, 2016; Huang et al., 2017; Liu, 2017; Zhao, 2018). Some studies also indicated significant benefits of mindfulness interventions in enhancing mindfulness levels, capabilities of daily living, and health-related QOL (Gan et al., 2019; Zhang et al., 2015). Notably, the subjects targeted in these studies were patients undergoing treatment in hospitals with existing physical impairments, rather than individuals who were discharged into the community.
There are also several limitations of existing studies on the effectiveness of MBI in the Chinese context. These include small sample size involved, lack of information about the basic characteristics of the study subjects, absence of baseline measurements and control groups, excessively short intervention periods, and overly simple descriptions of the conceptualization and operational processes of the intervention activities (Bédard et al., 2014; Simpson et al., 2017; Wang et al., 2019; Xu et al., 2015). This underscores the pressing need to address these research gaps by refining methodologies and enhancing the presentation of intervention processes.
In summary, the preceding literature review highlights that while contemporary Western studies generally support the efficacy of MBI across diverse populations, there exists a significant gap in research dedicated to assessing the effectiveness of MBI tailored for individuals with physical disability (PD). This research gap is particularly significant in the Chinese context due to China's large population (Shek et al., 2022). The scarcity of empirical studies in this area highlights the need for thorough exploration and rigorous investigation. Against this background, the primary purpose of this research is to assess the impact of MBIs on enhancing mental health functioning, emotional well-being, and health-related QOL in this marginalized population. The research seeks to answer the following research questions:
-
1.
Does MBI reduce psychological morbidity (indexed by depression and anxiety) in individuals with PD? With reference to the literature (Beauchamp et al., 2023; Cui, 2016; Hearn & Cross, 2020; Huang et al., 2017; Liu, 2017; Niu et al., 2022; Mir et al., 2023; Pradhan et al., 2007; Zhao, 2018), we expected that there would be reduction in depression and anxiety in people with PD after they join MBI (Hypotheses 1a and 1b).
-
2.
Does MBI promote mindfulness and self-compassion in people with PD after they join MBI? Based on the previous work (Friis et al., 2016; Johansson et al., 2015; Kılıç et al., 2021; Leov, 2016; Nakamura et al., 2013; Pradhan et al., 2007; Schellekens et al., 2017; Simpson et al., 2017; Toise et al., 2014), we predicted that people with PD would have elevated levels of mindfulness and self-compassion after intervention (Hypothesis 2a and Hypothesis 2b, respectively).
-
3.
Does MBI improve the health-related QOL of people with PD? Consistent with the literature (Banth & Ardebil, 2015; Gan et al., 2019; Morone et al., 2016; Wong et al., 2011; Zhang et al., 2015), we expected that there would be an improvement of QOL of people with PD after joining the program (Hypothesis 3).
Materials and methods
Participants
With the assistance of Guangzhou Ren Ren Social Service Centre (a local community rehabilitation service provider), participants were recruited from six communities in Guangzhou, China. The study took place between September 2020 and May 2021 (i.e., under COVID-19 pandemic). Participants were included if they: (1) were willing to participate in the intervention; (2) did not receive any psychological counseling or psycho-social treatment in the past three months; (3) did not experience cognitive impairment, substance abuse, or other mental disorders that may prevent effective understanding of the content of the intervention. The eligibility of participants was screened. Those who met the criteria were assigned to the MBI group or control group randomly. Both groups were invited to complete the pre-test and post-test after the intervention. Upon completion, the participants were given a gift valued RMB 50 (CYN) as a token of appreciation.
Measures
This study used a set of validated and standardized assessment tools to test the effectiveness of MBI interventions on a variety of emotional, psychological, and physical outcomes. These scales include the Self-Rating Depression Scale (SDS), the Self-Rating Anxiety Scale (SAS), the Mindful Attention Awareness Scale (MAAS), the Self-Compassion Scale Short-Form (SCS-SF), and the 12-item Short-Form Health Survey (SF-12).
The Self-Rating Depression Scale (SDS)
This scale was created to access a range of depressive symptoms, including mood, sleep patterns, appetite, and attention (Zung, 1971). It consists of 20 items and a 4-point Likert scale was used for each item. The scale calculates a cumulative score, with higher scores indicating more severe depressive symptoms. According to the results of the Chinese norm, the cutoff score of depression is 52, 53–62 is considered mild depression, 63–72 is considered moderate depression, and a score above 72 suggests severe depression (Zhang et al., 2016a, b). Reliability analyses showed that the SDS was internally consistent at baseline (alpha = 0.81) and post-test (alpha = 0.83).
The Self-Rating Anxiety Scale (SAS)
Developed by Zung et al. (1965), the SAS has been widely adopted to identify the severity of depressive symptoms in both clinical and research areas. Comprising 20 items, the SAS gauges diverse anxiety-related symptoms, including but not limited to nervousness, restlessness, and fear. Employing a 4-point Likert scale, it quantifies the severity of individual anxiety, with higher scores indicating heightened levels of severity. The Chinese normative criteria for the SAS categorize scores into specific bands (Xu et al., 2016): A score of 50–59 is considered mild anxiety, a score of 60–69 is considered moderate anxiety, and a score of 70 or above is considered severe anxiety. It was internally consistent at pretest (alpha = 0.83) and posttest (alpha = 0.84).
The Mindful Attention Awareness Scale (MAAS)
It is a self-report questionnaire comprising 15 items (Brown & Ryan, 2003). It aims to assess an individual's mindfulness level, gauging the extent to which they sustain attention to present-moment experiences. Respondents express their agreement with each statement on a 6-point Likert scale, typically spanning from 1 (almost always) to 6 (almost never). The total score is then computed, with elevated scores indicative of a heightened level of mindful attention awareness. In the context of this study, the MAAS exhibited very good reliability at baseline and posttest (alpha = 0.93 in both cases).
The Self-Compassion Scale-Short Form (SCS-SF)
This scale assesses an individual's self-compassion (Neff, 2003) and covers six dimensions with a total of 12 items: common humanity, self-isolation, self-kindness, self-criticism, present moment mindfulness, and excessive self-indulgence. Responses are provided on a 5-point Likert scale, ranging from "never" to "always." Elevated scores on the scale signify heightened levels of self-compassion. The scale was shown to be reliable at pretest (alpha = 0.91) and posttest (alpha = 0.94).
The 12-Item Short Form Health Survey (SF-12)
This scale assesses an individuals' health-related QOL (Jenkinson et al., 1997) in two domains: physical health and mental health, with higher scores indicating better health conditions. Studies have supported the validity of SF-12 in Chinese populations. In this study, reliability showed that the scale was reliable at pretest (alpha = 0.82) and posttest (alpha = 0.84).
Design and Procedure
The experimental design employed in this study employed both matching and random assignment techniques. Specifically, participants were initially matched based on demographic factors such as age, gender, and severity levels of disability. Subsequently, each matched pair was randomly allocated to either the MBI group or the control group. A two-armed randomized controlled design was adopted in this study with the involvement of two groups: a MBI group and a control group. The signed informed consent forms of participants were collected prior to the study. Ethical approval was obtained from the Guangdong University of Technology Review Board. Research data were collected through questionnaires administered during two periods: pre-test (prior to the intervention) and post-test (after the intervention). Baseline measurements were taken during the pre-test for levels of depression, anxiety, mindfulness, self-compassion, and overall health, and differences between the two groups were examined. If no significant differences were found between the groups, the MBI program was carried out within two weeks after the pre-test, and the post-test was conducted within a month after the intervention ended. The control group did not undergo MBI. Instead, they received routine home visit services. In contrast, the MBI group received weekly face-to-face mindfulness treatment sessions conducted by therapists during routine home visits over an eight-week period. It is important to note that participants in MBI group did not avail themselves of any other psychotherapy services during the study. Finally, in the post-test stage, the above indicators (i.e. levels of depression, anxiety, mindfulness, self-compassion, and overall health) were tested again to compare the differences between and within the groups.
Intervention
The mindfulness-based interventions were conducted at a community service center to individuals with PD in Guangzhou, China. A cohort of 257 participants in the MBI group underwent mindfulness-based therapy administered by trained therapists with 168 h of training. Each participant attended face to face intervention at their home once a week for a total of eight sessions weekly, amounting to eight sessions, each spanning 80 min. The therapist-to-participant ratio was maintained at 1:7–8, ensuring effective facilitation.
The framework guiding the mindfulness therapy program was anchored in the mindfulness meditation model proposed by Hölzel et al., (2011) delineated across four sequential stages: attention regulation (stage 1), body awareness (stage 2), emotional regulation (stage 3), and change in perspective on the self (stage 4). Throughout the intervention, the executive attention system (stage 1) enabled participants to discern conflicts hindering the maintenance of a mindful state during emotional triggers. Heightened body awareness (stage 2) facilitated the recognition of immediate physiological responses. Emotion regulation mechanisms,, encompassing reappraisal and exposure, extinction, and re-consolidation (Stage 3), aided in clearing reactive emotions, fostering the generation of new emotions, and consolidating emotional experiences. The dynamic interplay with perceptions, emotions, or cognition during the intervention engendered a transience that reshaped the participants' self-perception, culminating in self-transformation and heightened self-regulation ability (Stage 4). The design of the mindfulness intervention adhered to fundamental operational principles, with specific activities such as mindful breathing, body scanning, mindful eating, sitting meditation, and the incorporation of aromatherapy essential oils and relaxation music to enhance the experiential aspect (Fig. 1).
Given the potential for physical and emotional reactions like distraction, fatigue, or negative thoughts among participants, therapists were directed to integrate professional coaching skills, including active listening, motivational enhancement, empathy, goal clarification, and focus, to augment the effectiveness of the intervention. A detailed account of the intervention activities is presented in 1 (Table 1).
Data Analysis
The acquired data were analyzed using SPSS 27. Initially, descriptive statistics for the variables under investigation were examined. Subsequently, independent samples t-tests and chi-square tests were executed to compare demographic and baseline outcome variables among groups. Following this initial assessment, a series of 2 (group) * 2 (time) mixed-model ANOVAs were employed to explore whether the MBI group engaged in mindfulness practices demonstrated significant reductions in depression and anxiety, alongside increased levels of mindfulness, self-compassion, and health-related QOL in comparison to the control group.
Prior to conducting the mixed-model ANOVAs, adjustments were made to ensure the data adhered to normal distributions. This involved conducting homogeneity tests and the Box M test, which collectively affirmed the appropriateness of the data for subsequent analysis. In the ANOVAs, examination included the main effect of time, the main effect of group, and the interaction of group and time. In cases where the interaction between group and time was present, pairwise comparisons were conducted through post hoc tests to further identify within-subjects differences among outcome observations. The effect sizes were estimated and reported as partial eta squared (η2).
Results
In this study, 512 participants who met rigorous inclusion criteria were randomly assigned, with 257 individuals allocated to the Mindfulness-Based Intervention (MBI) group and 255 to the control group. Within the MBI group, there were 149 males and 108 females, with age ranging from 19 to 87 years (mean age = 64.13, SD = 11.95). Among them, 76.65% experienced moderate to lower levels of psychological distress (PD), and 91.44% had attained a junior high school level of education or lower. Furthermore, 80.54% were married, while the remainder were single (5.45%), widowed (10.12%), or divorced (3.89%). Additionally, over 60% were either unemployed or retired.
The control group consisted of 152 males and 103 females, aged between 20 and 91 years (mean age = 64.31, SD = 12.47). Within this group, 77.26% experienced moderate to lower levels of PD, and 90.98% had attained a junior high school level of education or lower. Similarly, 80% were married, with the remaining participants being single (5.49%), widowed (11.37%), or divorced (3.14%). Additionally, 63.92% were either unemployed or retired.
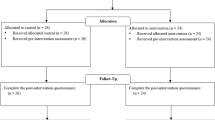
At post-intervention, 18 participants (3.51%) did not complete outcome measures, leaving 481 participants (MBI group: 248, control group: 233) for the post-test analysis, yielding an overall response rate of 93.94.0%, with rates of 96.50% in the MBI group and 91.37% in the control group. Figure 2 illustrates the flow of participant in the study.
Regarding the demographic characteristics, analysis of the baseline data indicated no statistically significant differences between both groups concerning age (t = -0.16, p > 0.5), gender (χ2 = 0.23, p > 0.5), severity levels of disability (χ2 = 0.72, p > 0.5), education level (χ2 = 4.28, p > 0.5), marital status (χ2 = -0.40, p > 0.5), and employment status (χ2 = 1.55, p > 0.5) (Table 2). The findings suggest that there was no pre-existing differences between the two groups in terms of these demographic characteristics.
Regarding depressive symptoms, the ANOVA test revealed significant main effects for both Time (F = 7.40, p < 0.05,η2 = 0.02) and Group (F = 7.73, p < 0.05,η2 = 0.02). Furthermore, a notable interaction emerged between Time and Group (F = 3.26, p < 0.05,η2 = 0.01). Post hoc testing, corroborated by visual inspection of plots, indicated no significant differences in depressive symptoms between both groups at baseline (F = 0.68, p > 0.05,η2 = 0.002). However, a discernible reduction in depressive symptoms was observed within the MBI group from baseline to post-test (F = 10.51, p < 0.01,η2 = 0.03). Conversely, no significant changes were noted in the control group over time (F = 0.41, p > 0.05,η2 = 0.001) (Table 3, Fig. 3). The findings supported Hypothesis 1a.
Regarding anxiety symptoms, the ANOVA results revealed a significant main effect for Group (F = 6.97, p < 0.05,η2 = 0.02), while the main effect for Time did not reach significance (F = 0.80, p > 0.05,η2 = 0.002). Additionally, a there was a significant Time X Group interaction (F = 9.90, p < 0.01,η2 = 0.03). Post hoc testing, confirmed with inspection of plots, disclosed no significant disparities in anxiety symptoms between both groups at baseline (F = 0.002, p > 0.05,η2 = 0.0001). Notably, within the MBI group, a significant reduction in anxiety symptoms was observed from baseline to post-test (F = 8.21, p < 0.01,η2 = 0.02). Conversely, no significant changes were observed in the control group throughout the study duration (F = 2.52, p > 0.05,η2 = 0.01) (Table 3, Fig. 4). The findings supported Hypothesis 1b.
Concerning mindfulness, the ANOVA results indicate a significant main effect for Group (F = 6.21, p < 0.05,η2 = 0.02) but not for Time (F = 2.15, p > 0.05,η2 = 0.004). Besides, a statistically significant interaction between Group and Time was identified (F = 5.29, p < 0.05,η2 = 0.01). Post hoc analyses, validated through plot inspection, revealed no substantial differences in mindfulness levels between both groups at baseline (F = 0.14, p > 0.05,η2 = 0.0005). As predicted, a notable improvement in mindfulness emerged from baseline to post-test in the experimental group (F = 7.31, p < 0.01,η2 = 0.02), whereas no statistically significant changes were observed in the control group across time (F = 0.34, p > 0.05,η2 = 0.001) (Table 3, Fig. 5). The findings support Hypothesis 2a.
For self-compassion, the ANOVA results indicated that both main effects for Group (F = 10.94, p < 0.01,η2 = 0.02) and Time (F = 14.40, p < 0.001,η2 = 0.03) were statistically significant. The interaction between Group and Time was also significant (F = 17.18, p < 0.001,η2 = 0.04). Post hoc testing, validated through careful examination of plots, revealed no substantial differences in self-compassion between both groups at baseline (F = 0.30, p > 0.05,η2 = 0.001). Nevertheless, within the MBI group, a significant improvement in self-compassion was observed from baseline to post-test (F = 34.41, p < 0.001,η2 = 0.06), while no significant changes were detected in the control group throughout the entirety of the study (F = 0.06, p > 0.05,η2 = 0.0001) (Table 3, Fig. 6). This observation provided support for Hypothesis 2b.
Two domains of health-related QOL were assessed: the physical domain and mental health domain. For the physical domain, the ANOVA results demonstrated that both the main effects for Group (F = 2.51, p < 0.05, η2 = 0.01) and Time (F = 4.23, p < 0.05, η2 = 0.01) were statistically significant. The interaction between Group and Time was also found to be significant (F = 6.36, p < 0.05, η2 = 0.02). Post hoc testing, confirmed with the plot inspections, revealed no significant differences in physical domain between both groups at baseline (F = 0.44, p > 0.05,η2 = 0.001). However, within the MBI group, a noteworthy improvement in PCS was observed from baseline to post-test (F = 10.88, p < 0.05,η2 = 0.02), while no significant changes were detected in the control group throughout the entire study duration (F = 0.11, p > 0.05,η2 = 0.0003) (Table 3, Fig. 7). This provides support for Hypothesis 3.
Similarly, for the results of mental health domain, the ANOVA outcomes indicated that both the main effects for Group (F = 13.60, p < 0.001,η2 = 0.03) and Time (F = 17.54, p < 0.001,η2 = 0.04) were statistically significant. The interaction between Group and Time was also found to be significant (F = 16.38, p < 0.001,η2 = 0.04). Post hoc testing, supported by a thorough examination of plots, revealed no substantial differences in mental health domain between both groups at baseline (F = 0.0004, p > 0.05,η2 = 0.0001). Nevertheless, within the MBI group, a significant enhancement in mental health domain was observed from baseline to post-test (F = 35.18, p > 0.05,η2 = 0.07), while no significant changes were detected in the control group throughout the entirety of the study (F = 0.01, p > 0.05,η2 = 0.0001) (Table 3, Fig. 8). This finding also provided support for Hypothesis 3.
Discussion
The current study explored the effects of MBI on psychological morbidity (indexed by depression and anxiety) as well as emotional well-being (mindfulness and self-compassion), along with the health-related QOL of individuals with PD in China. The findings demonstrated a significant impact of mindfulness-based intervention in this population. Participants who received MBI exhibited significant alleviation of psychological symptoms (depression and anxiety) compared to individuals with PD who did not undergo such interventions, giving support to Hypotheses 1a and 1b. These outcomes align with conclusions drawn from previous research on individuals with impaired physical functions in both Western and Chinese contexts (Beauchamp et al., 2023; Cui, 2016; Hearn & Cross, 2020; Huang et al., 2017; Liu, 2017; Mir et al., 2023; Niu et al., 2022; Pradhan et al., 2007; Zhao, 2018).
This study also showed that the mindfulness level of individuals with PD was significantly enhanced through MBI, and Hypothesis 2a was supported. This conclusion is in line with the findings of earlier Western studies (Leov, 2016; Pradhan et al., 2007). By practicing MBI, participants can focus more on the present moment and be more open to self-awareness and acceptance. This not only helps improve their QOL, but also encourages them to play a more active role in the psychological recovery process, thereby further gaining better adaptation to physical symptoms. The present findings offer practical guidance for introducing mindfulness to this population. Consequently, it provides insightful implications for both the academic community and clinical practitioners, advancing the application and development of mindfulness research among Chinese individuals with disabilities.
Besides promotion of mindfulness, self-compassion improved in the participants giving support to Hypothesis 2b. Although the effectiveness of MBI in promoting self-compassion levels among individuals with physical functional impairments has received attention in Western studies, scholarly discourse on this topic is scarce in China. This study confirms that MBI effectively enhances the self-compassion of individuals with PD. Participants who underwent MBI exhibited improvements in self-kindness, a reduction in self-criticism, self-isolation, and excessive self-indulgence, enhancement of common humanity, and improvement in present-moment mindfulness, aligning with conclusions from Western studies (Johansson et al., 2015; Kılıç et al., 2021; Simpson et al., 2017). Results of this study also support Hypothesis 3 that QOL for individuals with PD improved across time. Participation in MBI led to effective improvements in the health functioning of these individuals on both physical and psychological levels. This aligns with previous Western and Chinese research indicating consistent positive effects of MBI across different cultural backgrounds (Banth & Ardebil, 2015; Gan et al., 2019; Morone et al., 2016; Wong et al., 2011; Zhao et al., 2015). Firstly, the study results resonate with the positive influence of mindfulness on physical health. Individuals with PD, following a period of MBI training, demonstrated not only physiological improvements but also significant progress in disease management and rehabilitation. Mindfulness practice improves physical function by helping individuals perceive body signals more effectively and increase their tolerance for pain and discomfort. For individuals with PD, this physical and mental transformation process will bring them a more positive recovery experience, such as improving their QOL. Second, this research identified the positive influences of MBI on mental health. For individuals with PD, long-term physical illness may result in significant negative emotional burden, such as anxiety, depression, etc. Mindfulness methods can play an important role in improving the mental health of them and helping them establish a more positive attitude towards life. This intervention can educate individuals on how to release psychological stress, deal with negative emotions, and promote emotional stability in daily life. These research findings provide a reasonable theoretical basis for introducing MBI to a broader spectrum of individuals with PD, transcending cultural differences. In short, the present study provides valuable insights for future rehabilitation interventions and psychological health treatments. In practice, a deeper understanding of the mechanisms of MBI could enhance their potential in the rehabilitation and psychological well-being maintenance of individuals with physical disabilities.
As previous MBI practices were predominantly conducted in Western societies and targeted Western populations, this study's practical application and effectiveness evaluation demonstrate the efficacy of MBI in implementing interventions for individuals with PD in Chinese society. Similar to some earlier Chinese research, this study confirms that an intervention period of eight weeks is optimal for achieving effectiveness. Furthermore, in contrast to some projects utilizing group-based MBI, this study implements one-on-one, home-based sessions. Despite the higher personnel and time investment required for this intervention method, it better suits the practical needs of local communities with individuals with PD. As a majority of this population encounters significant challenges in traveling, and local support for transportation aids is limited, conducting activities outside the home would add to the barriers and burdens. Home-based, one-on-one services not only address transportation obstacles but also provide participants with more individualized attention during mindfulness activities, ensuring greater privacy in the service.
Overall, the findings from this research hold the potential to facilitate and encourage the incorporation of mindfulness-based methodologies into the comprehensive landscape of disability care and rehabilitation within the healthcare system in China. These results could serve as a catalyst, promoting the adoption and utilization of mindfulness-based practices as an integral component within the framework of providing care and support for individuals with PD. The present findings have the potential to inspire and guide clinical practices, offering actionable recommendations to healthcare professionals in China. Ultimately, this may facilitate the integration of mindfulness-based approaches into the broader framework of disability care and rehabilitation within the Chinese healthcare system. The study is also important in the context of COVID-19 because mental health and QOL were much impaired under COVID-19 (Shek, 2021; Shek et al., 2023).
Acknowledging the limitations of this study is crucial. The aftermath of the COVID-19 pandemic, marked by prolonged lockdowns and administrative disruptions in the study area following the implementation of MBI, hindered the opportunity for conducting subsequent tracking of intervention effectiveness. As a result, the study was unable to observe the enduring impacts of MBI on the physical and mental well-being of individuals with PD. Furthermore, the study's sample predominantly focused on older individuals with PD, with insufficient consideration for the circumstances of younger and middle-aged groups. Future research endeavors should focus on continuous tracking of intervention efficacy, ensuring a balanced age distribution within the research sample, exploring the impact of MBI on pain management and social interactions, and evaluating the varying effectiveness of this treatment across various categories of disabled individuals.
Data availability
For original data, please contact the corresponding author. Ethical approval does not cover making data openly accessible.
References
Anderson, N., & Ozakinci, G. (2018). Effectiveness of psychological interventions to improve quality of life in people with long-term conditions: Rapid systematic review of randomised controlled trials. BMC Psychology, 6(1), 1–17. https://doi.org/10.1186/s40359-018-0225-4
Apolinário-Hagen, J., Drüge, M., & Fritsche, L. (2020). Cognitive behavioral therapy, mindfulness-based cognitive therapy and acceptance commitment therapy for anxiety disorders: Integrating traditional with digital treatment approaches. Anxiety Disorders: Rethinking and Understanding Recent Discoveries, 1191, 291–329. https://doi.org/10.1007/978-981-32-9705-017
Banth, S., & Ardebil, M. D. (2015). Effectiveness of mindfulness meditation on pain and quality of life of patients with chronic low back pain. International Journal of Yoga, 8(2), 128. https://doi.org/10.4103/0973-6131.158476
Battalio, S. L., Tang, C. L., & Jensen, M. P. (2020). Resilience and function in adults with chronic physical disabilities: A cross-lagged panel design. Annals of Behavioral Medicine, 54(5), 297–307. https://doi.org/10.1093/abm/kaz048
Beauchamp, J. E., Sharrief, A., Chaoul, A., Casameni Montiel, T., Love, M. F., Cron, S., Prossin, A., Selvaraj, S., Dishman, D., & Savitz, S. I. (2023). Feasibility of a meditation intervention for stroke survivors and informal caregivers: A randomized controlled trial. BMC Psychology, 11(1), 9. https://doi.org/10.1186/s40359-022-01031-z
Bédard, M., Felteau, M., Marshall, S., Cullen, N., Gibbons, C., Dubois, S., ... & Moustgaard, A. (2014). Mindfulness-based cognitive therapy reduces symptoms of depression in people with a traumatic brain injury: results from a randomized controlled trial. The Journal of Head Trauma Rehabilitation, 29(4), E13-E22. https://doi.org/10.1097/htr.0b013e3182a615a0
Bishop, S. R., Lau, M., Shapiro, S., Carlson, L., Anderson, N. D., Carmody, J., & Devins, G. (2004). Mindfulness: A proposed operational definition. Clinical Psychology: Science and Practice, 11, 230–241. https://doi.org/10.1093/clipsy.bph077
Brown, K. W., & Ryan, R. M. (2003). The benefits of being present: mindfulness and its role in psychological well-being. Journal of personality and social psychology, 84(4), 822.
Cui, J. (2016). The impact of mindfulness stress reduction training on negative emotions in stroke patients during the rehabilitation period. Chinese Journal of Rehabilitation Medicine, 25(7), 703–704. https://doi.org/10.1155/2018/1986820
Friis, A. M., Johnson, M. H., Cutfield, R. G., & Consedine, N. S. (2016). Kindness matters: A randomized controlled trial of a mindful self-compassion intervention improves depression, distress, and HbA1c among patients with diabetes. Diabetes Care, 39(11), 1963–1971. https://doi.org/10.2337/dc16-0416
Gan, L., Qian, H., Li, H., & Han, S. (2019). The impact of mindfulness stress reduction combined with functional exercise rehabilitation training on the prognosis of elderly stroke patients. International Journal of Nursing, 5(38), 1358–1361. https://doi.org/10.3760/cma.j.issn.1673-4351.2019.10.005
Goodrich, E., Wahbeh, H., Mooney, A., Miller, M., & Oken, B. S. (2015). Teaching mindfulness meditation to adults with severe speech and physical impairments: An exploratory study. Neuropsychological Rehabilitation, 25(5), 708–732. https://doi.org/10.1080/09602011.2014.970201
Grossman, P., Niemann, L., Schmidt, S., & Walach, H. (2004). Mindfulness-based stress reduction and health benefits: A meta-analysis. Journal of Psychosomatic Research, 57(1), 35–43. https://doi.org/10.1016/S0022-3999(03)00573-7
Hardison, M. E., & Roll, S. C. (2016). Mindfulness interventions in physical rehabilitation: A scoping review. The American Journal of Occupational Therapy, 70(3), 7003290030p1–7003290030p9. https://doi.org/10.5014/ajot.2016.018069
Hearn, J. H., & Cross, A. (2020). Mindfulness for pain, depression, anxiety, and quality of life in people with spinal cord injury: A systematic review. BMC Neurology, 20(1), 1–11. https://doi.org/10.1186/s12883-020-1619-5
Hickey, A., Merriman, N. A., Bruen, C., Mellon, L., Bennett, K., Williams, D., Pender, N., & Doyle, F. (2019). Psychological interventions for managing cognitive impairment after stroke. The Cochrane Database of Systematic Reviews, 2019(8), 1–14. https://doi.org/10.1002/14651858.CD013406
Hofmann, S. G., Sawyer, A. T., Witt, A. A., & Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology, 78(2), 169. https://doi.org/10.1037/a0018555
Hölzel, B. K., Lazar, S. W., Gard, T., Schuman-Olivier, Z., Vago, D. R., & Ott, U. (2011). How does mindfulness meditation work? Proposing mechanisms of action from a conceptual and neural perspective. Perspectives on Psychological Science, 6(6), 537–559. https://doi.org/10.1177/1745691611419671
Huang, X., Zou, J., & Yang, M. (2017). The effects of mindfulness stress reduction therapy on anxiety and depression levels in post-stroke patients. Journal of Nursing. 24(7):62–64. CNKI:SUN:NFHL.0.2017–07–017
Jenkinson, C., Layte, R., Jenkinson, D., Lawrence, K., Petersen, S., Paice, C., & Stradling, J. (1997). A shorter form health survey: Can the SF-12 replicate results from the SF-36 in longitudinal studies? Journal of Public Health, 19(2), 179–186. https://doi.org/10.1093/oxfordjournals.pubmed.a024606
Johansson, B., Bjuhr, H., Karlsson, M., Karlsson, J. O., & Rönnbäck, L. (2015). Mindfulness-based stress reduction (MBSR) delivered live on the internet to individuals suffering from mental fatigue after an acquired brain injury. Mindfulness, 6, 1356–1365. https://doi.org/10.3109/02699052.2012.700082
Kabat-Zinn, J. (2003). Mindfulness-based interventions in context: Past, present, and future. Clinical Psychology, 10(2), 144–156. https://doi.org/10.1093/clipsy/bpg016
Kılıç, A., Hudson, J., McCracken, L. M., Ruparelia, R., Fawson, S., & Hughes, L. D. (2021). A systematic review of the effectiveness of self-compassion-related interventions for individuals with chronic physical health conditions. Behavior Therapy, 52(3), 607–625. https://doi.org/10.1016/j.beth.2020.08.001
Lebrasseur, A., Fortin-Bédard, N., Lettre, J., Bussières, E. L., Best, K., Boucher, N., Hotton, M., Beaulieu-Bonneau, S., Mercier, C., Lamontagne, M., & Routhier, F. (2021). Impact of COVID-19 on people with physical disabilities: A rapid review. Disability and Health Journal, 14(1), 101014. https://doi.org/10.1016/j.dhjo.2020.101014
Ledesma, D., & Kumano, H. (2009). Mindfulness-based stress reduction and cancer: A meta-analysis Psycho-Oncology: Journal of the Psychological. Social and Behavioral Dimensions of Cancer, 18(6), 571–579. https://doi.org/10.1002/pon.1400
Leov , J. N. (2016). An Online Mindfulness Intervention for Pain and Wellbeing (Thesis, Master of Health Sciences). University of Otago. Retrieved from http://hdl.handle.net/10523/6586
Liu, H. (2017). The effectiveness of mindfulness therapy intervention in improving depressive emotions in rheumatoid arthritis patients with bone and joint disorders. Chinese Journal of Traumatology Medicine, 25(5), 13–14. https://doi.org/10.13214/j.cnki.cjotadm.2017.05.008
Liu, F. B., Zhang, Z., Li, A. Q., Sheng, Z., & Zhang, M. (2022). Effects of mindfulness training on emotion and acceptance for people with disabilities: A systematic review. Chinese Journal of Rehabilitation Theory and Practice, 12, 105–110. https://doi.org/10.3969/j.issn.1006-9771.2022.01.016
Mace, C. (2007). Mindfulness and mental health: Therapy, theory and science. Routledge.
McCracken, L. M., Gauntlett-Gilbert, J., & Vowles, K. E. (2007). The role of mindfulness in a contextual cognitive-behavioral analysis of chronic pain-related suffering and disability. Pain, 131(1–2), 63–69. https://doi.org/10.1016/j.pain.2006.12.013
Merkes, M. (2010). Mindfulness-based stress reduction for people with chronic diseases. Australian Journal of Primary Health, 16(3), 200–210. https://doi.org/10.1071/PY09063
Mir, N., Sen, M. S., Mani, K., Sagar, R., Arulselvi, S., Kumar, S., Gupta, A., & Sagar, S. (2023). Impact of yoga intervention in lower limb amputees following trauma in relation to behavior and quality of life: A randomized controlled trial. International Journal of Yoga, 16(2), 106–115. https://doi.org/10.4103/ijoy.ijoy_156_23
Morone, N. E., Greco, C. M., Moore, C. G., Rollman, B. L., Lane, B., Morrow, L. A., Glynn, N. W., & Weiner, D. K. (2016). A mind-body program for older adults with chronic low back pain: A randomized clinical trial. JAMA Internal Medicine, 176(3), 329–337. https://doi.org/10.1001/jamainternmed.2015.8033
Na, L., & Yang, L. (2022). Psychological and behavioral responses during the COVID-19 pandemic among individuals with mobility and/or self-care disabilities. Disability and Health Journal, 15(1), 101216. https://doi.org/10.1016/j.dhjo.2021.101216
Nakamura, Y., Lipschitz, D. L., Kuhn, R., Kinney, A. Y., & Donaldson, G. W. (2013). Investigating efficacy of two brief mind-body intervention programs for managing sleep disturbance in cancer survivors: A pilot randomized controlled trial. Journal of Cancer Survivorship, 7(2), 165–182. https://doi.org/10.1007/s11764-012-0252-8
Neff, K. D. (2003). The development and validation of a scale to measure self-compassion. Self and identity, 2(3), 223–250.
Niu, Y., Sheng, S., Chen, Y., Ding, J., Li, H., Shi, S., Wu, J., & Ye, D. (2022). The efficacy of group acceptance and commitment therapy for preventing post-stroke depression: A randomized controlled trial. Journal of Stroke and Cerebrovascular Diseases, 31(2), 106225. https://doi.org/10.1016/j.jstrokecerebrovasdis.2021.106225
Pascoe, M. C., Thompson, D. R., & Ski, C. F. (2017). Yoga, mindfulness-based stress reduction and stress-related physiological measures: A meta-analysis. Psychoneuroendocrinology, 86, 152–168. https://doi.org/10.1016/j.psyneuen.2017.08.008
Plaza, I., Demarzo, M. M. P., Herrera-Mercadal, P., & García-Campayo, J. (2013). Mindfulness-based mobile applications: Literature review and analysis of current features. JMIR mHealth and uHealth, 1(2), e24. https://doi.org/10.2196/mhealth.2733
Pradhan, E. K., Baumgarten, M., Langenberg, P., Handwerger, B., Gilpin, A. K., Magyari, T., Hochberg, M. C., & Berman, B. M. (2007). Effect of mindfulness-based stress reduction in rheumatoid arthritis patients. Arthritis Care & Research, 57(7), 1134–1142. https://doi.org/10.1002/art.23010
Reibel, D., & McCrown, D. (2019). Mindfulness Based Stress Reduction: theory, practice and evidence base. In I. Ivtzan (Ed.), Handbook of mindfulness-based programmes. Routlege.
Schellekens, M. P. J., van den Hurk, D. G. M., Prins, J. B., Donders, A. R. T., Molema, J., Dekhuijzen, R., van der Drift, M. A., & Speckens, A. E. M. (2017). Mindfulness-based stress reduction added to care as usual for lung cancer patients and/or their partners: A multicentre randomized controlled trial. Psycho-Oncology, 26(12), 2118–2126. https://doi.org/10.1002/pon.4430
Second National Sample Survey Office for Persons with Disabilities. (2008). Data analysis report of the second national sample survey on persons with disabilities [In Chinese]. Huaxia Publishing House.
Shapiro, S. L., Carlson, L. E., Astin, J. A., & Freedman, B. (2006). Mechanisms of mindfulness. Journal of Clinical Psychology, 62, 373–386. https://doi.org/10.1002/jclp.20237
Shek, D. T. (2021). COVID-19 and quality of life: Twelve reflections. Applied Research in Quality of Life, 16(1), 1–11. https://doi.org/10.1007/s11482-020-09898-z
Shek, D. T., Peng, H., & Zhou, Z. (2022). Children and adolescent quality of life under socialism with Chinese characteristics. Applied Research in Quality of Life, 17(5), 2447–2453. https://doi.org/10.1007/s11482-021-09999-3
Shek, D. T., Leung, J. T., & Tan, L. (2023). Social policies and theories on quality of life under COVID-19: in search of the missing links. Applied Research in Quality of Life, 24, 1–17.
Shelov, D. V., Suchday, S., & Friedberg, J. P. (2009). A pilot study measuring the impact of yoga on the trait of mindfulness. Behavioural and Cognitive Psychotherapy, 37(5), 595–598. https://doi.org/10.1017/S1352465809990361
Simpson, R., Mair, F. S., & Mercer, S. W. (2017). Mindfulness-based stress reduction for people with multiple sclerosis–a feasibility randomised controlled trial. BMC Neurology, 17(1), 1–12. https://doi.org/10.1186/s12883-017-0880-8
Tirch, D., Silberstein, L. R., & Kolts, R. L. (2015). Buddhist psychology and cognitive-behavioral therapy: A clinician’s guide. The Guilford Press.
Toise, S. C. F., Sears, S. F., Schoenfeld, M. H., Blitzer, M. L., Marieb, M. A., Drury, J. H., Slade, M. D., & Donohue, T. J. (2014). Psychosocial and cardiac outcomes of yoga for ICD patients: A randomized clinical control trial. Pace - Pacing and Clinical Electrophysiology, 37(1), 48–62. https://doi.org/10.1111/pace.12252
Wahbeh, H., & Oken, B. S. (2016). Internet mindfulness meditation intervention for the general public: Pilot randomized controlled trial. JMIR Mental Health, 3, e37. https://doi.org/10.2196/mental.5900
Wang, M., Liao, W., & Chen, X. (2019). Effects of a short-term mindfulness-based intervention on comfort of stroke survivors undergoing inpatient rehabilitation. Rehabilitation Nursing Journal, 44(2), 78–86. https://doi.org/10.1097/rnj.0000000000000098
Wang, J., Wei, Y., Xie, H., Xu, Z., Wang, X., Zeng, X., & Chang, F. (2022). The overall impact on the daily life of people with disabilities in Mainland China: two cross-sectional studies. Research Square, 1–16. https://doi.org/10.21203/rs.3.rs-2396934/v1
Wielgosz, J., Goldberg, S. B., Kral, T. R., Dunne, J. D., & Davidson, R. J. (2019). Mindfulness meditation and psychopathology. Annual Review of Clinical Psychology, 15, 285–316. https://doi.org/10.1146/annurev-clinpsy-021815-093423
Wong, S. Y. S., Chan, F. W. K., Wong, R. L. P., Chu, M. C., Lam, Y. Y. K., Mercer, S. W., & Ma, S. H. (2011). Comparing the effectiveness of mindfulness-based stress reduction and multidisciplinary intervention programs for chronic pain: A randomized comparative trial. The Clinical Journal of Pain, 27(8), 724–734. https://doi.org/10.1097/AJP.0b013e3182183c6e
Xu, J. W., Li, B. R., Pu, X. B., Huang, C., Li, J., Zhang, Y. L., Qin, Y., & Yu, T. (2015). Effect of mindfulness-based stress reduction for post-stroke depression. Sichuan Phychological Health, 28(6), 523–525. https://doi.org/10.11886/j.issn.1007-3256.2015.06.011
Xu, W. X., Yao, J. W., & Chen, L. F. (2016). Anxiety in patients with chronic Corpulmonale and its effect on exercise capacity. Iranian Journal of Public Health, 45(8), 1004.
Zhang, S., & Chen, Z. (2021). China’s prevention policy for people with disabilities during the COVID-19 epidemic. Disability & Society, 36(8), 1368–1372. https://doi.org/10.1080/09687599.2021.1933913
Zhang, Y., Hao, Z., & Guo, X. (2015). Clinical effects of mindfulness-based behavioral training intervention on post-stroke depression. Journal of Integrated Traditional Chinese and Western Medicine on Cardio-Cerebrovascular Disease, 13(14), 1679–1681. https://doi.org/10.1002/gps.5273
Zhang, J., Xu, R., Wang, B., & Wang, J. (2016a). Effects of mindfulness-based therapy for patients with breast cancer: A systematic review and meta-analysis. Complementary Therapies in Medicine, 26, 1–10. https://doi.org/10.1016/j.ctim.2016.02.012
Zhang, Y. X., Zhang, X. Q., Wang, Q. R., Yuan, Y. Q., Yang, J. G., Zhang, X. W., & Li, Q. (2016b). Psychological burden, sexual satisfaction and erectile function in men whose partners experience recurrent pregnancy loss in China: A cross-sectional study. Reproductive Health, 13(1), 1–5. https://doi.org/10.1001/archpsyc.1965.01730060026004
Zhao, Y. (2018). The impact of mindfulness stress reduction therapy on anxiety and depression levels in post-stroke patients. International Journal of Nursing, 7, 956–958. https://doi.org/10.3760/cma.j.issn.1673-4351.2018.07.029
Zung, W. W. (1971). A rating instrument for anxiety disorders Psychosomatics. Journal of Consultation and Liaison Psychiatry, 12(6), 371–379. https://doi.org/10.1016/S0033-3182(71)71479-0
Zung, W. W., Richards, C. B., & Short, M. J. (1965). Self-rating depression scale in an outpatient clinic: Further validation of the SDS. Archives of General Psychiatry, 13(6), 508–515. https://doi.org/10.1001/archpsyc.1965.01730060026004
Funding
This work was supported by The National Social Science Fund of China under Grant 19CSH069 and Guangdong Provincial Social Science Planning Regular Project under Grant GD22CSH01.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors report no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Liang, Ly., Shek, D.T.L. A randomized controlled trial of mindfulness-based intervention on individuals with physical disabilities in China. Applied Research Quality Life (2024). https://doi.org/10.1007/s11482-024-10305-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11482-024-10305-0