Abstract
The objective of this work is to deepen the analysis of the socioeconomic determinants of mental health, paying special attention to the impact of inequality, not only in income distribution but also in gender, racial, health and education inequality, social isolation, including new variables to measure loneliness, and healthy habits, on the mental health status. For this purpose, a cross-sectional model for a sample of 2735 counties in the United States is estimated using Ordinary Least Squares in its robust version to solve the detected heteroscedasticity problems. The results obtained show that inequality, social isolation and certain lifestyles, such as smoking or insomnia, are detrimental to mental health, while sexual activity prevents mental distress. On the other hand, poor counties suffer more cases of suicide, with food insecurity being the main problem for mental health. Finally, we found detrimental effects of pollution on mental health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
In recent decades, the role of mental health has grown in importance, not only for the scientific community, but also for policy makers as reflected by the fact that it has been incorporated into the Sustainable Development Goals. It is important to note that depression is one of the leading causes of disability and that suicide is the leading cause of death in the population between 15 and 29 years of age. In fact, according to the World Health Organization (WHO), more than 700,000 people die by suicide each year.
The United States is not immune to this problem and with a mortality rate of 16.1 per 100,000 inhabitants, it is one of the countries with the highest suicide rates. For all these reasons, in this paper we propose to analyze the socioeconomic determinants of mental health in the United States. To this end, we base our analysis on three pillars: firstly, inequality, understood in a broad sense, i.e., inequality in income distribution, gender, race, health, education and the labor market. This in-depth analysis of the incidence of inequality on mental health is the main novelty of this work. Second, we use several variables as proxies for social isolation to test how they affect mental health. In this sense, the use of new variables such as teleworking or driving alone every day to work is another important novelty of this article. Finally, the main lifestyle habits are analyzed to contribute to the analysis of the effect of these variables on mental health.
For this purpose, a robust cross-sectional model was estimated for a sample ranging from 1790 to 2735 U.S. counties (depending on the availability of data for certain variables). The results obtained show that inequality in all its aspects is indeed a risk factor for mental disorders, although social isolation is perhaps more important as an explanatory variable. Finally, tobacco addiction and insomnia are shown to be the habits most detrimental to mental health.
The second empirical analysis establishes the theoretical framework and then, in the third section, explains the model and discusses the results. Finally, in the fourth section, the conclusions are developed.
Theoretical Framework
The economic literature has extensively studied the effects of inequality on different health outcomes (Pickett & Wilkinson, 2015; Matthew & Brodersen, 2018), and among these, some authors have addressed the relationship between inequality and mental health. Thus, works such as Burns et al. (2017), have analyzed the relationship between inequality in income distribution and certain mental disorders. However, as pointed out by Patel et al. (2018), a review of the papers published on the relationship between income inequality and mental health shows inconsistent results, with only one third of them concluding that inequality in income distribution is a risk factor for mental health.
Less studied is the case of the association between other forms of inequality and the prevalence of mental disorders. In this sense, there is a lack of work addressing the incidence of gender inequality on mental health (Yu, 2018). Even so, we can highlight the works of Hopcroft and Bradley (2007), and Van de Velde et al. (2013), who perform a macro-level analysis of the effects of gender inequality on mental health. As with inequality in income distribution, research on the effects of gender inequality on mental health reflects inconclusive results (Hopcroft & Bradley, 2007; Seedat et al., 2009; Van de Velde et al., 2013; Hagen & Rosenstrôm, 2016).
Most papers that have studied racial inequality as a risk factor for mental health have measured this racial inequality through discrimination (Brown et al., 2000; Lewis et al., 2015; Wallace et al., 2016; Mouzon et al., 2017; Williams, 2018). In this case, the results are indeed conclusive and point out that racial discrimination negatively affects mental well-being. Our work aims to delve deeper into the impact of racial inequality on mental health, measuring this inequality through the unequal distribution of poverty across races.
Regarding social isolation as a determinant of mental health, there is a broad consensus from researchers about the positive impact of interpersonal relationships on mental well-being (Almedom, 2005; Bassett & Moore, 2013), However, an associated problem encountered by researchers is that it is unclear how social isolation, loneliness, and other related concepts should be measured when analyzing their effect on mental health (Windle et al., 2011; Courtin & Knapp, 2015; Rhode et al., 2016; Chirstiansen et al., 2021). Therefore, we propose new measures of social isolation such as teleworking and driving alone to work. In doing so, we aim to give robustness to the results obtained by the already published works.
Finally, the economic literature has also paid attention to the association between healthy habits and mental health. Thus, authors such as Reid et al. (2009), Taylor et al. (2011), Milojevich and Lukowaki (2016), Chattu et al. (2018), Sullivan and Ordiah (2018), and Merikanto and Partonen (2021) among others warn of the adverse effects of insomnia on mental health. Also, the impact of tobacco and alcohol addiction on mental health has aroused the interest of researchers, highlighting the works on the adolescent population by Mason et al. (2008), Balogun et al. (2014), Skogen et al. (2014), and Ferreira et al. (2019). Likewise, the relationship between obesity, physical activity, and mental health has been analyzed (Kivimâki et al., 2009). However, the mechanisms linking obesity and mental illness are unclear (Avila et al., 2015). Thus, there are authors who point out that mental disorders are the cause of obesity (Nicholson, 1946), others speak of a bidirectional relationship (Cameron et al., 2012) and others point to obesity as a risk factor for mental health (De Hert et al., 2011).
Therefore, as mental disorders cannot be explained solely through genetic factors (Sanders et al., 1999; Sullivan et al., 2000; Fava & Kendler, 2000), and given the importance of socioeconomic determinants, we propose, from here on, to continue to deepen the analysis of the incidence of these factors on mental health, with emphasis on inequality, social isolation and healthy living habits.
Empirical Analysis
A cross-sectional linear model has been estimated to analyze whether social isolation, lifestyle, and inequality, broadly understood, observed in each North American county have any effect on mental health in the United States. The mental health data were obtained from the County Health Rankings & Roadmaps, University of Wisconsin Health Institute, and refer to 2019. In this sense, we have worked with a database of 3,218 U.S. counties, which is almost 100% of all counties in the U.S. Even so, the inequality and mental health data by counties have only allowed us to use a sample between 1,790 and 2,735 counties, depending on the inequality and mental health measure used. In any case, the sample used is representative of the overall U.S. situation.
This study adapts the classic model of Dalghren and Whitehead (1991) for a comparative analysis between counties in the United States. The model of these two economists has been widely used and shows the determinants of health in concentric layers, from structural determinants (external layer) to individual lifestyles (internal layer), placing at the center the characteristics of individuals that cannot be modified, such as sex, age or constitutional factors (Fig. 1).
The Dalghren-Whitehead model of determinants in health. Source: Dalghren and Whitehead (1991)
According to these authors, individuals are endowed with risk factors such as age, sex and other genetic factors that influence their potential for ultimate health. Likewise, personal behaviors and lifestyles also play a role. People who are economically disadvantaged tend to exhibit behaviors that depart from healthy living, such as smoking, alcohol and drug abuse, and poor diet. On the other hand, labor and environmental conditions, and access to basic services constitute another set of determinants of health status. Differences in housing conditions, occupational risks, whether one has a job, and the possibility of having free, quality education, basic health services, and infrastructure access to drinking water, sewage systems, paved roads, are key factors in the differences in health shown by different social groups. Finally, the economic, cultural and environmental conditions prevailing in society as a whole, as well as the economic situation of the country, will also affect the health outcomes of the population as a whole.
In our case, we adapt this model to analyze the socioeconomic determinants of mental health.
-
A. Data
The variables used in this work are summarized in the following table (Table 1):
-
B. The model
A linear model was developed and estimated through Ordinary Least Squares in its robust version of variances and covariances, since when the Breusch-Pagan test was performed, the p-value obtained showed the presence of heteroscedasticity. The model was estimated without a constant term. Although the decision to use a constant term or not is a problem that generates much discussion (Casella, 1983), nevertheless, there are circumstances in which it is appropriate or even necessary not to use the error term. As Eisenhauer (2003) points out, in the case where the dependent variable is zero if the vector of independent variables is also zero, the error term can be omitted. This is the case of the estimated model where variables such as population density are used. If this variable had a value equal to zero, the variables measuring mental health status would also have a value equal to zero.
The model used is as follows:
Where,
Mentalhealth is the dependent variable. In this sense, three variables that reflect the mental health status have been used, each of them implying an aggravation of mental disorders. Thus, first, the variable “Poor mental health days” has been used, which measures the average number of days of mental unhealthiness reported in the last 30 days during 2019. The second variable used is “Frequent mental distress” which reflects the percentage of adults reporting 14 or more poor mental health days per month (age-adjusted), therefore, it emphasizes the population experiencing more chronic and probably more severe mental health problems. Finally, the variable “Suicide” was used, which measures the number of suicide deaths per 100,000 population (age-adjusted). This variable reflects the extreme case of a mental health problem. The objective, therefore, is to analyze how the independent variables used affect mental health and how these effects change as mental illness worsens.
Income measures the average real income per household in the county in relation to the average real income per household in the state. It is, therefore, a first variable that measures inequality, in this case, between counties.
Inequality is one of the explanatory variables on which we have focused the objective of this work, i.e., the aim is to analyze how inequality within each county affects mental health. In this sense, we have tried to analyze inequality in a broad sense, that is, not only inequality in income distribution, but also gender inequality and racial inequality. For this purpose, six measures of inequality were used:
-
The Gini index and the 80/20 ratio have been used to measure inequality in income distribution.
-
In terms of gender inequality, the Gender Pay Gap, which measures the average earnings of women in relation to men, and the female poverty variable, which refers to the percentage of poor women in relation to the total poor population, have been used.
-
Racial inequality is measured by the percentage of the African American poor population out of the total population below the poverty line, and by racial segregation, i.e., the degree to which black and white residents live separately from each other in a county.
MHP refers to the number of mental health providers per 1,000 population. It is therefore a proxy variable for access to mental health care, since access to care requires not only financial coverage, but also access to providers.
Uninsured refers to the percentage of people under age 65 who did not have health insurance in 2019. This is a proxy variable for health inequality in terms of health coverage. Therefore, its use is intended to strengthen the analysis of the effects of inequality on mental health.
University measures the percentage of the population with university studies. As with the previous variable, this is a proxy variable for educational inequality and will allow us to delve deeper into inequality as a determinant of mental health.
Unemployment measures the unemployment rate in 2020. This variable shows, on the one hand, the inequality in the labor market between counties and, on the other hand, the lack of income.
Badhealth measures the percentage of adults in a county who consider themselves to be in poor or fair (age-adjusted) health during 2019. The purpose of using this variable is to test whether physical health has a relationship to mental health.
Sleep refers to the percentage of adults reporting having slept less than 7 h on average per day (age-adjusted) during 2018. Sleep is an important part of a healthy lifestyle, and by employing this variable we try to analyze whether lack of sleep can cause psychiatric disorders.
Smoke refers to the percentage of a county’s adult population reporting smoking every day or some days, and having smoked at least 100 cigarettes in their lifetime, in 2019. We use “Smoke” as a proxy variable for addiction.
Obesity is the percentage of the adult population with a body mass index (BMI) equal to or greater than 30 kg/m2. The objective is to see if obesity is a cause of poor mental health.
Inactivity is the percentage of adults aged 18 years and older reporting no leisure-time physical activity in the last month during 2019.
Alcohol measures the percentage of a county’s adult population reporting binge drinking in the past 30 days, during 2019.
STI refers to sexually transmitted diseases measured through the number of newly diagnosed chlamydia cases per 100,000 population in 2019. We use “STI” as a proxy variable for sexual activity.
Density is the population density of the county in 2020, i.e., number of inhabitants per km2. This is the first variable that will allow us to analyze the effects of social isolation on mental health.
Associations measures the number of membership associations per 10,000 inhabitants in 2019.
WFH refers to “work from home,“ i.e., the percentage of people who teleworked in 2018. Teleworking prevents physical contact with coworkers and is therefore a good proxy for loneliness.
Driving measures the percentage of the labor force that drives alone to work.
Broadband is the percentage of households with a broadband Internet connection. We use this variable as a proxy for home Internet use.
SHP is “Severe housing problems” and refers to the percentage of households with at least 1 of these 4 housing problems: overcrowding, high housing costs, lack of kitchen facilities or lack of plumbing facilities. With this, we want to check whether these types of problems lead to poorer mental health.
Food measures the percentage of the population lacking adequate access to food in 2019.
Pollution refers to air pollution - particulate matter and is a measure of fine particles in the air. It is presented as the daily average density of fine particles in micrograms per cubic meter. Fine particulate matter is defined as air pollutant particles with an aerodynamic diameter of less than 2.5 micrometers (PM2.5).
-
C. Results and Discussion
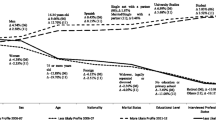
As mentioned above, the model was estimated by OLS in its robust version to solve the problem of heteroscedasticity detected. Eighteen estimates have been made, resulting from the use of 6 different measures of inequality and the three dependent variables used to characterize mental health. The results are reflected in the following tables (Tables 2, 3, and 4):
The first conclusion that can be drawn from the 18 estimates is that the model is robust since there are hardly any significant changes in either the estimated regressors or their significance. Likewise, the quality of the fit is good since the R2 ranges between 0.906 and 0.997.
As for the values obtained, in most cases they are those expected a priori. Starting with the variables measuring inequality, the first measure used is the real mean income of the county in relation to that of the state in which it is located. The parameter obtained is highly significant in almost all the estimates made, although the sign changes depending on the measure of mental health. Thus, it is observed that those counties that are richer in relative terms are the ones that suffer more days of poor mental health. However, when these mental health problems become more severe (“frequent mental distress”), the incidence of this variable decreases in value and significance. In the extreme case, i.e., suicide, the sign changes and it is the poorest counties that suffer the most from this problem. This changing result is consistent with what is happening in the economic literature. As Ridley et al. (2020) and Shah et al. (2021) point out, the results obtained in published work on the subject do not allow inferences to be drawn about causality between income and mental health, which hampers opportunities to inform public policy. Thus, for example, while Gresenz et al. (2001) find a strong correlation between individual income level and mental health, although not at the State level, Araya et al. (2003) find no association between income and prevalence of common mental disorders. In any case, the results obtained in our work agree with those obtained by Thomson et al. (2022), who demonstrate the existence of a deterioration in mental health as a result of lower income. It should be taken into account that in richer and therefore more economically dynamic counties, competition is greater and this can lead to some mental distress (Colantone et al., 2019).
In order to study in depth, the effects of inequality on mental health, six measures of inequality have been used for each county, with the aim of analyzing not only inequality in income distribution, commonly used in the literature, but also gender inequality and racial inequality. This allows us to study the effects of inequality, understood in a global way, on the dependent variables, and to test whether greater inequality within the county has effects on mental health. According to the results obtained, the positive (with one exception) and significant sign in 11 of the 18 estimates allows us to conclude that inequality is a determinant of mental health. The greater the inequality within the county, the worse the mental health. In this sense, precarious working conditions, the stress this entails and the comorbidities associated with poverty that may characterize these counties with higher inequality could explain these results (Llosa et al., 2018; Rönnblad et al., 2019). However, analyzing the inequality measures used one by one, these results can be nuanced. The first thing to note is that racial inequality is the most significant (Table 4). In all estimates, the estimated sign is significant. Moreover, in five of the six estimates made, the sign is positive, so that racial inequality leads to worse mental health, as Wallace et al. (2016) also show for the case of the United Kingdom. What is striking is the negative sign obtained when we use suicide as the dependent variable and the percentage of the black population below the poverty line as a measure of inequality. This result invites us to affirm that the black population is less prone to suicide in situations of poverty as Early and Akers (1993), Goldsmith et al. (2002) and more recently Riddell et al. (2018) have already shown. Regarding income inequality (Table 2), although the sign is always positive, it is only significant in 2 of the 6 estimates made. In this sense, the greater the income inequality within the county, the greater the mental problems, although we did not find any significant result for the extreme case of suicide. This inconclusive result is consistent with that reached by Gresenz et al. (2001), who find no relationship between inequality in income distribution and mental health, or that of Yu (2018) who does find a relationship between income inequality and mental health for men, but not for women. Something similar occurs with gender inequality since the estimated regressor is only significant in three of the six estimates made, although in this case we can indeed state that gender inequality harms mental health and is even a determinant of suicide. These results confirm the findings of McAllister et al. (2018), according to which better mental health is related to lower gender inequality. Mar et al. (2022) also find strong evidence for the relationship between gender inequality, mental health, and suicide.
There are other variants of inequality that can also affect mental health. One of them is health. In this regard, two variables have been used. First, we have employed access to mental health care measured through mental health providers. It is important to note that about 30% of the population lives in a county designated as a mental health professional shortage area (HRSA, 2022). However, the results we obtain are not significant, so we cannot draw conclusions about whether more mental health care facilities lead to a reduction in potential mental disorders. Therefore, we use a second variable, “uninsured”, to analyze whether health coverage, or lack thereof, influences mental health. The results obtained are significant, although different for the extreme case of suicide. Thus, in the case of poor mental health or frequent mental disorders, the parameter obtained is negative, which implies that the higher the percentage of the population that is not insured, the fewer the mental health problems. This result, a priori surprising, can be explained by the high health costs in the USA, which can lead the population without health coverage not to see a specialist when suffering from some type of disorder (Carter et al., 2020). However, when the disease worsens and leads individuals to the extreme solution of suicide, the sign changes and becomes positive, with the uninsured population suffering more from the most severe mental problems, as also shown by Johnson and Brookover (2020), and Ong et al. (2021).
Another form of inequality that can affect mental health is related to education. In this work we have used the percentage of the population with university studies since in the USA there is great inequality in access to higher education (Jerrim et al., 2015). The results obtained show a negative sign, although only significant in 7 of the 18 estimates made. This would show that higher education promotes better mental health (Jiang et al., 2020), since there is a certain correlation between the level of education attained and a better job, better life habits and a better health status. It is worth noting that when we use suicide as a dependent variable, education is significant in five of the six estimates made, making education a key factor in the fight against very serious mental disorders (Lorant et al., 2018).
As mentioned above, more education implies a higher probability of finding a job and thus covering all those material needs whose lack can lead to a deterioration of mental health. This is why we use the “unemployment” variable, which also reflects the inequalities between counties in terms of labor markets. However, the parameter obtained is only significant when suicide is used as the dependent variable. The positive sign allows us to conclude that a higher unemployment rate implies a higher suicide rate, as also shown by Amiri (2021).
From here, the next group of variables that have been studied refer to the health status and life habits. First, we analyzed whether there was any relationship between physical and mental health status. The results obtained, significant in all cases except for suicide, show that there is a direct relationship between both variables, i.e., poor physical health leads to poor mental health (Ohrnberger et al., 2017; Luo et al., 2020). However, as we have discussed above, when we use suicide as the dependent variable, the parameter ceases to be significant, contrary to what most of the economic literature says (Fairweather et al., 2006; Phillips & Hempstead, 2022; Qin et al., 2022). Even so, as Fiske et al. (2008) argue, the relationship between poor health and suicide tends to occur in older population groups. Furthermore, according to Ahmedani et al. (2017) it is important to nuance which determinants of physical health status most affect mental health and suicide. These authors find that lack of sleep is a key factor. This is why we included the variable “sleep” in our analysis. The results obtained show a positive and significant relationship between the percentage of people with sleep problems and the three variables used to measure mental health problems. Therefore, we can affirm that insomnia is a risk factor for mental health as also shown by Chattu et al. (2018), Sullivan and Ordiah (2018), and Merikanto and Partonen (2021) among others.
Other variables that reflect the lifestyle of the population have been included in this analysis. Thus, the estimated parameter for the variable “smoke” is always positive and highly significant, whereby the higher the percentage of smokers the worse the mental health, as also argued by Ferreira et al. (2019). There is a common perception that smoking generally helps people to manage stress and can be a form of “self-medication” in people with mental health problems, although this addiction, like others, generates withdrawal symptoms that worsen mental health (Taylor et al., 2021). However, when we estimate the relationship between excessive alcohol consumption and mental health, the result obtained is surprising. The sign is negative and significant in all estimates except when we use suicide as the dependent variable. In this case, the estimated parameter is not significant. Therefore, we cannot affirm that excessive alcohol consumption is a risk factor for mental health. In this regard, Li et al. (2022) also conclude that, for certain population groups, alcohol consumption is a protective factor against mental disorders. On the other hand, the economic literature has also analyzed the relationship between obesity and physical activity on mental health (Avila et al., 2015). The results obtained in our work show a negative and significant sign for these two variables. Therefore, we cannot affirm that those counties with a higher percentage of obese people and those who report not doing any physical activity have greater mental problems. In this sense, Biddle et al. (2019) also do not obtain evidence of a causal association between physical activity and mental health. To our knowledge, obesity and lack of physical activity would not be a cause but a consequence of mental disorders, as Van der Valk et al. (2018) also demonstrate. In fact, Rajan and Menon (2017) point to a bidirectional relationship between obesity and mental health. Finally, the variable “STI” was used as a proxy for sexual activity. The results obtained, significant in 12 of the 18 estimates made, show that sexual activity reduces mental disorders (Brody, 2010; Mollaioli et al., 2021; Gianotten, 2021).
The economic literature has discussed in depth the relationship between social isolation and mental disorders (Wang et al., 2017). This paper aims to delve into the relationship between the two concepts with the use of five variables. Thus, first, we employ the variable measuring population density to test whether denser counties have lower mental problems. Epidemiological studies show that the risk of serious mental illness is higher in cities than in rural areas, where population density is lower (Gruebner et al., 2017) since higher density is associated with lower social contacts (Giacco et al., 2022). However, the negative and significant sign in 11 of the 18 estimates made allow us to affirm that in those counties with higher population per km2 makes personal relationships closer and fosters better mental health. This result, contrary to that shown by other authors, perhaps requires a more specific analysis of this relationship, as Lai et al. (2021) have done. These authors conclude that rather than population density per se, it is urban design that determines the relationship between density and mental health. In fact, the evidence of the impacts of increasing urban densification on loneliness and social isolation in humans is still inconclusive. For this reason, we use other variables that reflect social isolation. Thus, for the case of the variable “associations”, we did not find a significant relationship with respect to mental health, making it unclear whether these types of social associations improve mental health (Wakefield et al., 2019). Regarding teleworking, a variable that reflects the lack of social contact in the workplace, the positive and highly significant sign obtained in all the estimates made shows that, indeed, a higher percentage of teleworkers and, therefore, greater social isolation, leads to greater mental disorders and even the extreme case of suicide. Authors such as Mann and Holdsworth (2003) and De Sio et al. (2021) have already demonstrated the harmful effects of teleworking on mental health. This result is confirmed when we use the variable “driving” which reflects the percentage of people who drive alone every day to work. Again, this variable is used as a proxy for social isolation, and the results obtained (positive and highly significant sign in all the estimates made) allow us to conclude that social isolation is a key risk factor for mental disorders. Finally, Internet access was used as a proxy variable for Internet use at home and, therefore, less social contact. The positive and highly significant sign shows that the higher the use of the Internet and social networks, the higher the probability of suffering from mental disorders. These results agree with those obtained by Grant et al. (2019), Arzani-Birgani et al. (2021), and Golin (2022).
Other problems that can cause mental distress are material problems in a household and food insecurity. Now, which of the two generates more distress? Our analysis reveals that food insecurity is a risk factor for mental health, whereas we did not find a clear result for the variable reflecting severe household problems. Probably, as suggested by Singh et al. (2019), it would be necessary to analyze each of the household problems to see how they individually impact mental health. The harmful effects of food insecurity on mental health have also been shown by authors such as Pourmotabbed et al. (2020) among others.
Finally, the effect of pollution on mental health has been analyzed. The results obtained allow us to affirm that pollution is a risk factor for mental health, although in the extreme case of suicide, the sign changes, so we cannot affirm that those more polluting counties suffer from a higher suicide rate (Heo et al., 2021). As Ventriglio et al. (2021) argue, the impact of pollution on public health is well known, but the association between environmental pollutants and mental health has been little analyzed, and most of these yield inconclusive results. In any case, our results confirm the theses of Chen et al. (2018) and Yang et al. (2021).
Conclusion
Is inequality a risk factor for mental health? What lifestyle habits worsen mental health the most? What are the effects of the implementation of teleworking on mental disorders? To these and other questions we have tried to answer in this paper. Using a sample of 2,735 U.S. counties, a cross-sectional linear model has been estimated. The results obtained allow us to conclude that income is a key factor determining mental health status. While wealthier counties are more likely to suffer from mild mental disorders, when these worsen to the extreme case of suicide, it is the poorer counties that suffer the most. However, it is not severe housing problems that lead to the extreme deterioration of mental health, but rather the food insecurity suffered by poor families. For this reason, public assistance programs to meet the most basic needs are necessary in this country, since there are many households that suffer as a result of the strong inequality that exists. In fact, inequality, understood in a broad sense, is a key determinant of mental health. For this reason, public policies must be implemented to mitigate income differences, and to fight against gender inequality and all types of racial discrimination. In addition, the health coverage network should continue to be extended to the entire American population, and a scholarship plan should be promoted to allow greater access to higher education. All of this will result in fewer mental health problems.
On the other hand, because of the COVID-19 pandemic, many companies have adapted to increased teleworking. This, although it has served to prevent the virus, is a problem for mental health, as our results show. Thus, we show that the social isolation produced by teleworking, driving alone to work and the increased use of the Internet at home are seriously damaging to mental health. Therefore, a more detailed analysis of the pros and cons of promoting teleworking should be carried out by policy makers and companies.
The third pillar on which we have based our analysis of mental disorders is healthy lifestyle habits. In this regard, we emphasize that lack of sleep and addiction to tobacco are risk factors for mental health, while sexual activity is a good medicine against this type of disorder.
Finally, pollution also harms mental health. Thus, we find yet another argument for policymakers to step up measures to combat climate change.
However, this work is not without limitations. The first limitation is the lack of post-COVID-19 mental health data, which would have allowed us to draw stronger conclusions about the incidence of social isolation and mental health. The data we have been able to work with refer to 2019, so future updates of the data will allow the effect of COVID-19 to be included and will undoubtedly improve the analysis performed. Likewise, it would have been desirable to have more measures of both gender and racial inequality to make the analysis more robust. Thus, for example, it would have been very interesting to have available measures of gender inequality by US counties such as the Global Gender Gap, Gender Inequality Index or the Social Watch Gender Equity Index. Likewise, having a database on multidimensional racial inequality, as calculated by Rohde and Guest (2013) might have solved some of the problems of non-significance that we have encountered.
Data Availability
All the data used in this work are available in the web pages listed in Table 1.
References
Ahmedani, B. K., Peterson, E. L., Hu, Y., Rossom, R. C., Lynch, F., Lu, C. Y., … Simon, G. E. (2017). Major physical health conditions and risk of suicide. American Journal of Preventive Medicine, 53(3), 308–315.
Almedom, A. M. (2005). Social capital and mental health: an interdisciplinary review of primary evidence. Social Science & Medicine, 61(5), 943–964.
Amate-Fortes, I., Guarnido-Rueda, A., & Molina-Morales, A. (2020). World analysis of the determinants of the inequality in health. Is the measurement of Inequality important? Revija za Socijalnu Politiku, 27(1), 83–98.
Amiri, S. (2021). Unemployment and suicide mortality, suicide attempts, and suicide ideation: a meta-analysis. International Journal of Mental Health. https://doi.org/10.1080/00207411.2020.1859347
Araya, R., Lewis, G., Rojas, G., & Fritsch, R. (2003). Education and income: which is more important for mental health? Journal of Epidemiology & Community Health, 57(7), 501–505.
Arzani-Birgani, A., Zarei, J., Favaregh, L., & Ghanaatiyan, E. (2021). Internet addiction, mental health, and sleep quality in students of medical sciences, Iran: a cross-sectional study. Journal of Education and Health Promotion. https://doi.org/10.4103/jehp.jehp_1506_20
Avila, C., Holloway, A. C., Hahn, M. K., Morrison, K. M., Restivo, M., Anglin, R., & Taylor, V. H. (2015). An overview of links between obesity and mental health. Current Obesity Reports, 4(3), 303–310.
Balogun, O., Koyanagi, A., Stickley, A., Gilmour, S., & Shibuya, K. (2014). Alcohol consumption and psychological distress in adolescents: a multi-country study. Journal of Adolescent Health, 54(2), 228–234.
Bassett, E., & Moore, S. (2013). Mental health and social capital: Social capital as a promising initiative to improving the mental health of communities. In A.J. Rodriguez-Morales (Ed.), Current Topics in Public Health (Ch. 28) InTech.
Biddle, S. J., Ciaccioni, S., Thomas, G., & Vergeer, I. (2019). Physical activity and mental health in children and adolescents: an updated review of reviews and an analysis of causality. Psychology of Sport and Exercise, 42, 146–155.
Burns, J. K., Tomita, A., & Lund, C. (2017). Income inequality widens the existing income-related disparity in depression risk in post-apartheid South Africa: Evidence from a nationally representative panel study. Health & place, 45, 10–16.
Brody, S. (2010). The relative health benefits of different sexual activities. The Journal of Sexual Medicine, 7(4), 1336–1361.
Brown, T. N., Williams, D. R., Jackson, J. S., Neighbors, H. W., Torres, M., Sellers, S. L., & Brown, K. T. (2000). Being black and feeling blue”: the mental health consequences of racial discrimination. Race and Society, 2(2), 117–131.
Cameron, A. J., Magliano, D. J., Dunstan, D. W., Zimmet, P. Z., Hesketh, K., Peeters, A., & Shaw, J. E. (2012). A bi-directional relationship between obesity and health-related quality of life: evidence from the longitudinal AusDiab study. International Journal of Obesity, 36(2), 295–303.
Carter, S. P., Cowan, T., Snow, A., Cerel, J., & Tucker, R. (2020). Health insurance and mental health care utilization among adults who identify as transgender and gender diverse. Psychiatric Services, 71(2), 151–157.
Casella, G. (1983). Leverage and regression through the origin. The American Statistician, 37(2), 147–152. https://doi.org/10.1080/00031305.1983.10482728
Centers for Disease Control and Prevention. (2009). Sociodemographic differences in binge drinking among adults–14 states, 2004. MMWR: Morbidity and Mortality Weekly Report, 58(12), 301–304.
Chattu, V. K., Manzar, M. D., Kumary, S., Burman, D., Spence, D. W., & Pandi-Perumal, S. R. (2018, December). The global problem of insufficient sleep and its serious public health implications. In Healthcare (Vol.7, No. 1, p.1). MDPI.
Chen, S., Oliva, P., & Zhang, P. (2018). Air pollution and mental health: evidence from China. NBER Working Paper w24686.
Christiansen, J., Qualter, P., Friis, K., Pedersen, S. S., Lund, R., Andersen, C. M., … Lasgaard, M. (2021). Associations of loneliness and social isolation with physical and mental health among adolescents and young adults. Perspectives in Public Health, 141(4), 226–236.
Colantone, I., Crino, R., & Ogliari, L. (2019). Globalization and mental distress. Journal of International Economics, 119, 181–207.
Courtin, E., & Knapp, M. (2015). Health and wellbeing consequences of social isolation and loneliness in old age. NIHR School for Social Care Research.
Dalghren, G., & y Whitehead, M. (1991). Policies and strategies to promote social equity in health. Institute for Future Studies.
De Hert, M., Correll, C. U., Bobes, J., Cetkovich-Bakmas, M., Cohen, D. A. N., Asai, I., … Leucht, S. (2011). Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry, 10(1), 52.
De Sio, S., Cedrone, F., Nieto, H. A., Lapteva, E., Perri, R., Greco, E., … Buomprisco, G. (2021). Telework and its effects on mental health during the COVID-19 lockdown. European Review for Medical And Pharmacological Sciences, 25(10), 3914–3922.
Early, K. E., & Akers, R. L. (1993). “It’s a white thing”: an exploration of beliefs about suicide in the african-american community. Deviant Behavior, 14(4), 277–296.
Eisenhauer, J. G. (2003). Regression through the origin. Teaching Statistics, 25, 76–80.
Fairweather, A. K., Anstey, K. J., Rodgers, B., & Butterworth, P. (2006). Factors distinguishing suicide attempters from suicide ideators in a community sample: social issues and physical health problems. Psychological Medicine, 36(9), 1235–1245.
Fava, M., & Kendler, K. S. (2000). Major depressive disorder. Neuron, 28(2), 335–341.
Ferreira, V. R., Jardim, T. V., Sousa, A. L. L., Rosa, B. M. C., & Jardim, P. C. V. (2019). Smoking, alcohol consumption and mental health: data from the Brazilian study of cardiovascular risks in adolescents (ERICA). Addictive Behaviors Reports, 9, 100147.
Fiske, A., O’Riley, A. A., & Widoe, R. K. (2008). Physical health and suicide in late life: an evaluative review. Clinical Gerontologist, 31(4), 31–50.
Gee, G. C., & Ford, C. L. (2011). Structural racism and health inequities: old issues, New Directions1. Du Bois Review: Social Science Research on Race, 8(1), 115–132.
Giacco, D., Kirkbride, J. B., Ermakova, A. O., Webber, M., Xanthopoulou, P., & Priebe, S. (2022). Neighbourhood characteristics and social isolation of people with psychosis: a multi-site cross-sectional study. Social Psychiatry and Psychiatric Epidemiology, 57(9), 1907–1915. https://doi.org/10.1007/s00127-021-02190-x
Gianotten, W. L. (2021). The (mental) health benefits of sexual expresión. In M. Lew-Starowicz, A. Giraldi, T. H. C. Krüger (Eds.), Psychiatry and sexual medicine: A comprehensive guide for clinical practitioners. Springer International Publishing. https://doi.org/10.1007/978-3-030-52298-8
Goldsmith, S. K., Pellmar, T. C., Kleinman, A. M., & Bunney, W. E. (2002). Reducing suicide: a national imperative. National Academy Press.
Golin, M. (2022). The effect of broadband internet on the gender gap in mental health: Evidence from Germany. Health Economics, 31, 6–21.
Grant, J. E., Lust, K., & Chamberlain, S. R. (2019). Problematic smartphone use associated with greater alcohol consumption, mental health issues, poorer academic performance, and impulsivity. Journal of Behavioral Addictions, 8(2), 335–342.
Gresenz, C. R., Sturm, R., & Tang, L. (2001). Income and mental health: unraveling community and individual level relationships. Journal of Mental Health Policy and Economics, 4(4), 197–204.
Gruebner, O., Rapp, M. A., Adli, M., Kluge, U., Galea, S., & Heinz, A. (2017). Cities and mental health. Deutsches Ärzteblatt International, 114(8), 121.
Hagen, E. H., & Rosenström, T. (2016). Explaining the sex difference in depression with a unified bargaining model of anger and depression. Evolution Medicine and Public Health, 2016(1), 117–132.
Heo, S., Lee, W., & Bell, M. L. (2021). Suicide and associations with air pollution and ambient temperature: a systematic review and meta-analysis. International Journal of Environmental Research and Public Health, 18(14), 7699.
Hopcroft, R. L., & Bradley, D. B. (2007). The sex difference in depression across 29 countries. Social Forces, 85(4), 1483–1507.
HRSA (Health Resources and Services Administration) (2022). Designated health professional shortage areas statistics. US Department of Health & Human Services. Available at https://data.hrsa.gov. Accessed 29 July 2022.
Jerrim, J., Chmielewski, A. K., & Parker, P. (2015). Socioeconomic inequality in access to high-status colleges: a cross-country comparison. Research in Social Stratification and Mobility, 42, 20–32.
Jiang, W., Lu, Y., & Xie, H. (2020). Education and mental health: evidence and mechanisms. Journal of Economic Behavior & Organization, 180, 407–437.
Johnson, K. F., & Brookover, D. L. (2020). Counselors’ role in decreasing suicide in mental health professional shortage areas in the United States. Journal of Mental Health Counseling, 42(2), 170–186.
Kawachi, I., Kennedy, B. P., Gupta, V., & Prothrow-Stith, D. (1999). Women’s status and the health of women and men: a view from the States. Social Science & Medicine, 48(1), 21–32.
Kivimäki, M., Batty, G. D., Singh-Manoux, A., Nabi, H., Sabia, S., Tabak, A. G., … Jokela, M. (2009). Association between common mental disorder and obesity over the adult life course. The British Journal of Psychiatry, 195(2), 149–155.
Kramer, M. R., & Hogue, C. R. (2009). Is segregation bad for your health? Epidemiologic Reviews, 31(1), 178–194.
Lai, K. Y., Sarkar, C., Kumari, S., Ni, M. Y., Gallacher, J., & Webster, C. (2021). Calculating a national anomie density ratio: Measuring the patterns of loneliness and social isolation across the UK’s residential density gradient using results from the UK Biobank study. Landscape and Urban Planning, 215, 104194.
Lee, K. H., Dvorak, R. G., Schuett, M. A., & van Riper, C. J. (2017). Understanding spatial variation of physical inactivity across the continental United States. Landscape and Urban Planning, 168, 61–71.
Lewis, T. T., Cogburn, C. D., & Williams, D. R. (2015). Self-reported experiences of discrimination and health: scientific advances, ongoing controversies, and emerging issues. Annual Review of Clinical Psychology, 11, 407.
Li, Y., Zhang, C., Ding, S., Li, J., Li, L., Kang, Y., … Duan, Y. (2022). Physical activity, smoking, alcohol consumption and depressive symptoms among young, early mature and late mature people: a cross-sectional study of 76,223 in China. Journal of Affective Disorders, 299, 60–66.
Llosa, J. A., Menéndez-Espina, S., Agulló-Tomás, E., & Rodríguez-Suárez, J. (2018). Job insecurity and mental health: a meta-analytical review of the consequences of precarious work in clinical disorders. Anales de Psicología, 34(2), 211–221. https://doi.org/10.6018/analesps.34.2.281651
Lorant, V., de Gelder, R., Kapadia, D., Borrell, C., Kalediene, R., Kovács, K., … Mackenbach, J. P. (2018). Socioeconomic inequalities in suicide in Europe: the widening gap. The British Journal of Psychiatry, 212(6), 356–361.
Luo, M. S., Chui, E. W. T., & Li, L. W. (2020). The longitudinal associations between physical health and mental health among older adults. Aging & Mental Health, 24(12), 1990–1998.
Mann, S., & Holdsworth, L. (2003). The psychological impact of teleworking: stress, emotions and health. New Technology Work and Employment, 18(3), 196–211.
Mar, J., Larrañaga, I., Ibarrondo, O., González-Pinto, A., las, Hayas, C., Fullaondo, A., …. UPRIGHT Consortium. (2022). Socioeconomic and gender inequalities in mental disorders among adolescents and young adults. Revista de Psiquiatría y Salud Mental. https://doi.org/10.1016/j.rpsm.2022.07.001
Mason, W. A., Kosterman, R., Haggerty, K. P., Hawkins, J. D., Redmond, C., Spoth, R. L., & Shin, C. (2008). Dimensions of adolescent alcohol involvement as predictors of young-adult major depression. Journal of Studies on Alcohol and Drugs, 69(2), 275–285.
Matthew, P., & Brodersen, D. M. (2018). Income inequality and health outcomes in the United States: an empirical analysis. The Social Science Journal, 55(4), 432–442.
McAllister, A., Fritzell, S., Almroth, M., Harber-Aschan, L., Larsson, S., & Burström, B. (2018). How do macro-level structural determinants affect inequalities in mental health?–a systematic review of the literature. International Journal for Equity in Health, 17(1), 1–14.
Merikanto, I., & Partonen, T. (2021). Eveningness increases risks for depressive and anxiety symptoms and hospital treatments mediated by insufficient sleep in a population-based study of 18,039 adults. Depression and Anxiety, 38(10), 1066–1077.
Milner, A., Kavanagh, A., Scovelle, A. J., O’Neil, A., Kalb, G., Hewitt, B., & King, T. L. (2021). Gender equality and health in high-income countries: a systematic review of within-country indicators of gender equality in relation to health outcomes. Women’s Health Reports, 2(1), 113–123.
Milojevich, H. M., & Lukowski, A. F. (2016). Sleep and mental health in undergraduate students with generally healthy sleep habits. PLoS One, 11(6), e0156372.
Mollaioli, D., Sansone, A., Ciocca, G., Limoncin, E., Colonnello, E., Di Lorenzo, G., & Jannini, E. A. (2021). Benefits of sexual activity on psychological, relational, and sexual health during the COVID-19 breakout. The Journal of Sexual Medicine, 18(1), 35–49.
Mouzon, D. M., Taylor, R. J., Keith, V. M., Nicklett, E. J., & Chatters, L. M. (2017). Discrimination and psychiatric disorders among older African Americans. International Journal of Geriatric Psychiatry, 32(2), 175–182.
Nicholson, W. M. (1946). Emotional factors in obesity. The American Journal of the Medical Sciences, 211, 443–447.
Ohrnberger, J., Fichera, E., & Sutton, M. (2017). The relationship between physical and mental health: a mediation analysis. Social Science & Medicine, 195, 42–49.
Ong, M. S., Lakoma, M., Gees Bhosrekar, S., Hickok, J., McLean, L., Murphy, M., … Ross-Degnan, D. (2021). Risk factors for suicide attempt in children, adolescents, and young adults hospitalized for mental health disorders. Child and Adolescent Mental Health, 26(2), 134–142.
Patel, V., Burns, J. K., Dhingra, M., Tarver, L., Kohrt, B. A., & Lund, C. (2018). Income inequality and depression: a systematic review and meta-analysis of the association and a scoping review of mechanisms. World Psychiatry, 17(1), 76–89.
Phillips, J. A., & Hempstead, K. (2022). The role of context in shaping the relationship between physical health and suicide over the life course. SSM-Population Health, 17, 101059.
Pickett, K. E., & Wilkinson, R. G. (2015). Income inequality and health: a causal review. Social Science & Medicine, 128, 316–326.
Pourmotabbed, A., Moradi, S., Babaei, A., Ghavami, A., Mohammadi, H., Jalili, C., … Miraghajani, M. (2020). Food insecurity and mental health: a systematic review and meta-analysis. Public Health Nutrition, 23(10), 1778–1790.
Qin, P., Syeda, S., Canetto, S. S., Arya, V., Liu, B., Menon, V., & Gunnell, D. (2022). Midlife suicide: A systematic review and meta-analysis of socioeconomic, psychiatric and physical health risk factors. Journal of Psychiatric Research, 154, 233–241.
Rajan, T. M., & Menon, V. (2017). Psychiatric disorders and obesity: a review of association studies. Journal of Postgraduate Medicine, 63(3), 182.
Reid, G. J., Hong, R. Y., & Wade, T. J. (2009). The relation between common sleep problems and emotional and behavioral problems among 2-and 3‐year‐olds in the context of known risk factors for psychopathology. Journal of Sleep Research, 18(1), 49–59.
Riddell, C. A., Harper, S., Cerdá, M., & Kaufman, J. S. (2018). Comparison of rates of firearm and nonfirearm homicide and suicide in black and white non-hispanic men, by US state. Annals of Internal Medicine, 168(10), 712–720.
Ridley, M., Rao, G., Schilbach, F., & Patel, V. (2020). Poverty, depression, and anxiety: causal evidence and mechanisms. Science, 370(6522), eaay0214.
Rohde, N., & Guest, R. (2013). Multidimensional racial inequality in the United States. Social Indicators Research, 114(2), 591–605.
Rohde, N., D’Ambrosio, C., Tang, K. K., & Rao, P. (2016). Estimating the mental health effects of social isolation. Applied Research in Quality of Life, 11(3), 853–869.
Rönnblad, T., Grönholm, E., Jonsson, J., Koranyi, I., Orellana, C., Kreshpaj, B., … Bodin, T. (2019). Precarious employment and mental health. Scandinavian Journal of Work Environment & Health, 45(5), 429–443.
Sanders, A. R., Detera-Wadleigh, S. D., & Gershon, E. S. (1999). Molecular genetics of mood disorders. In D. S. Charney, E. J. Nestler, & B. S. Bunney (Eds.), Neurobiology of Mental Illness (299–316). Oxford.
Seedat, S., Scott, K. M., Angermeyer, M. C., Berglund, P., Bromet, E. J., Brugha, T. S., … Kessler, R. C. (2009). Cross-national associations between gender and mental disorders in the World Health Organization World Mental Health surveys. Archives of General Psychiatry, 66(7), 785–795.
Shah, N., Walker, I. F., Naik, Y., Rajan, S., O’Hagan, K., Black, M., … Stansfield, J. (2021). National or population level interventions addressing the social determinants of mental health–an umbrella review. BMC Public Health, 21(1), 1–14.
Singh, A., Daniel, L., Baker, E., & Bentley, R. (2019). Housing disadvantage and poor mental health: a systematic review. American Journal of Preventive Medicine, 57(2), 262–272.
Skogen, J. C., Sivertsen, B., Lundervold, A. J., Stormark, K. M., Jakobsen, R., & Hysing, M. (2014). Alcohol and drug use among adolescents: and the co-occurrence of mental health problems. Ung@ hordaland, a population-based study. BMJ Open, 4(9), e005357.
Sullivan, P. F., Neale, M. C., & Kendler, K. S. (2000). Genetic epidemiology of major depression: review and meta-analysis. American Journal of Psychiatry, 157(10), 1552–1562.
Sullivan, K., & Ordiah, C. (2018). Association of mildly insufficient sleep with symptoms of anxiety and depression. Neurology Psychiatry and Brain Research, 30, 1–4.
Taylor, D. J., Gardner, C. E., Bramoweth, A. D., Williams, J. M., Roane, B. M., Grieser, E. A., & Tatum, J. I. (2011). Insomnia and mental health in college students. Behavioral Sleep Medicine, 9(2), 107–116.
Taylor, G. M., Lindson, N., Farley, A., Leinberger-Jabari, A., Sawyer, K., te Water Naudé, R., … Aveyard, P. (2021). Smoking cessation for improving mental health. Cochrane Database of Systematic Reviews, (3), CDO13522. https://doi.org/10.1002/14651858.CD013522.pub2
Thomson, R. M., Igelström, E., Purba, A. K., Shimonovich, M., Thomson, H., McCartney, G., … Katikireddi, S. V. (2022). How do income changes impact on mental health and wellbeing for working-age adults? A systematic review and meta-analysis. The Lancet Public Health, 7(6), e515–e528.
Van der Valk, E. S., Savas, M., & van Rossum, E. F. (2018). Stress and obesity: are there more susceptible individuals? Current Obesity Reports, 7(2), 193–203.
Van de Velde, S., Huijts, T., Bracke, P., & Bambra, C. (2013). Macro-level gender equality and depression in men and women in Europe. Sociology of Health & Illness, 35(5), 682–698.
Ventriglio, A., Bellomo, A., di Gioia, I., Di Sabatino, D., Favale, D., De Berardis, D., & Cianconi, P. (2021). Environmental pollution and mental health: a narrative review of literature. CNS Spectrums, 26(1), 51–61.
Wakefield, J. R., Bowe, M., Kellezi, B., McNamara, N., & Stevenson, C. (2019). When groups help and when groups harm: Origins, developments, and future directions of the “Social Cure” perspective of group dynamics. Social and Personality Psychology Compass, 13(3), e12440.
Wallace, S., Nazroo, J., & Bécares, L. (2016). Cumulative effect of racial discrimination on the mental health of ethnic minorities in the United Kingdom. American Journal of Public Health, 106(7), 1294–1300.
Wang, J., Lloyd-Evans, B., Giacco, D., Forsyth, R., Nebo, C., Mann, F., & Johnson, S. (2017). Social isolation in mental health: a conceptual and methodological review. Social Psychiatry and Psychiatric Epidemiology, 52(12), 1451–1461.
Williams, D. R. (2018). Stress and the mental health of populations of color: advancing our understanding of race-related stressors. Journal of Health and Social Behavior, 59(4), 466–485.
Windle, K., Francis, J., & Coomber, C. (2011). Preventing loneliness and social isolation: interventions and outcomes (pp. 1–16). Social Care Institute for Excellence. Available from: http://www.scie.org.uk/publications/briefings/files/briefing39.pdf. Accessed 5 Aug 2022.
Yang, Z., Song, Q., Li, J., Zhang, Y., Yuan, X. C., Wang, W., & Yu, Q. (2021). Air pollution and mental health: the moderator effect of health behaviors. Environmental Research Letters, 16(4), 044005.
Yu, S. (2018). Uncovering the hidden impacts of inequality on mental health: a global study. Translational Psychiatry, 8(1), 1–10.
Acknowledgements
The authors Ignacio Amate-Fortes and Almudena Guarnido-Rueda are grateful for all the suggestions received during the research stay at the Economics Department of UC Santa Barbara.
Funding
Open Access funding provided thanks to the Universidad de Almería/CBUA. This study was funded by the European Union, Junta de Andalucía and University of Almeria, with reference number UAL-FEDER 2020, UAL2020-SEJ-D1999.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
There is no financial interest or benefit.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Amate-Fortes, I., Guarnido-Rueda, A., Martínez-Navarro, D. et al. Social Isolation, Healthy Habits, Inequality and Mental Health in the United States. Applied Research Quality Life 18, 1617–1643 (2023). https://doi.org/10.1007/s11482-023-10155-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11482-023-10155-2