Abstract
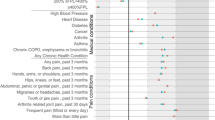
Evidence indicates that veterans using VA healthcare services have poor health-related quality of life (HRQOL). Little is known, however, about differences in HRQOL among those who only use VA services and those who also use non-VA services. We sought to evaluate differences in HRQOL among veterans who use: (1) only non-VA services (2) only VA services and (3) both VA and non-VA services (i.e., dual users). A cross-sectional study of 39,942 US veterans who completed the CDC’s 2004 Behavioral Risk Factor Surveillance System (BRFSS) survey was analyzed. Self-rated measures of global health status and the number of days per month that veterans were limited by physical or mental problems were extracted from BRFSS survey data as outcomes. Multivariate logistic regression demonstrated that, compared to those receiving all healthcare outside of VA, veterans receiving VA care were more likely to report poorer health outcomes, including worse global health status, greater impairments in physical functioning, and increased limitations regarding routine activities (p’s ≤ .05). Both exclusive and dual users of VA services reported poorer HRQOL than individuals not using VA services. More research is needed regarding veterans’ health status, particularly in the context of dual use.
Similar content being viewed by others
Notes
As derived from self-reported height and weight in BRFSS.
Unfortunately, however, questions regarding other important comorbid health conditions that may influence self-reported health such as the presence of hypertension, coronary heart disease, or stroke, were not included within the core module for 2004. Thus, we were unable to fully account for these health conditions in our model.
Fully adjusted (Model 2) odds ratios reported here. See Table 2 for results of both models.
Odds ratios for the most severe degree of impairment (i.e., 14+ days in the previous month) are reported here. See Table 2 for results of both impairment categories.
References
Agha, Z., Lofgren, R. P., VanRuiswyk, J. R., & Layde, P. M. (2000). Are patients at Veterans Affairs medical centers sicker? Archives of Internal Medicine, 160, 3252–7.
Borowsky, S. J., & Cowper, D. C. (1999). Dual use of VA and non-VA primary care. Journal of General Internal Medicine, 14, 274–80.
Centers for Disease Control and Prevention. (2004). Behavioral Risk Factor Surveillance System, Summary Data Quality Report. Available from: ftp://ftp.cdc.gov/pub/Data/Brfss/2004SummaryDataQualityReport.pdf.
Centers for Disease Control and Prevention. (2005). Health-related quality of life surveillance—United States, 1993–2002. Morbidity and Mortality Weekly Report, 54, SS-4.
Crosby, R. D., Kolotkin, R. L., & Williams, G. R. (2003). Defining clinically meaningful change in health- related quality of life. Journal of Clinical Epidemiology, 56, 395–407.
Guyatt, G. H., Fenny, D. H., & Patrick, D. L. (1993). Measuring health-related quality of life. Annals of Internal Medicine, 118, 622–9.
Hankin, C. S., Spiro, A., Miller, D. R., & Kazis, L. (1999). Mental disorders and mental health treatment among U.S. Department of Veterans Affairs outpatients: the Veterans Health Study. American Journal of Psychiatry, 156, 1924–30.
Helmer, D., Sambamoorthi, U., Shen, Y., et al. (2008). Opting out of an integrated healthcare system: dual-system use is associated with poorer glycemic control in veterans with diabetes. Primary Care Diabetes, 2, 73–80.
Hynes, D. M., Koelling, K., Stroupe, K., et al. (2007). Veterans’ access to and use of Medicare and Veterans Affairs healthcare. Medical Care, 45, 214–23.
Idler, E. L., & Benyamini, Y. (1997). Self-rated health and mortality: a review of twenty-seven community studies. Journal of Health & Social Behavior, 38, 21–37.
Jia, H., & Lubetkin, E. I. (2005). The impact of obesity on health-related quality of life in the general adult US population. Journal of Public Health, 27, 156–64.
Jia, H., Zheng, Y., Reker, D. M., et al. (2007). Multiple system utilization and mortality for veterans with stroke. Stroke, 38, 355–60.
Kazis, L. E. (2000). The Veterans SF-36 health status questionnaire: development and application in the Veterans Health Administration. Monitor, Medical Outcomes Trust, 5, 1–14.
Kazis, L. E., Miller, D. R., Clark, J., et al. (1998). Health-related quality of life in patients served by the Department of Veterans Affairs: results from the Veterans Health Study. Archives of Internal Medicine, 158, 626–32.
Kazis, L. E., Ren, X. S., Lee, A., et al. (1999). Health status in VA patients: results from the Veterans Health Study. American Journal of Medical Quality, 14, 28–38.
Liu, C. F., Chapko, M., Bryson, C. L., et al. (2010). Use of outpatient care in Veterans Health Administration and Medicare among veterans receiving primary care in community-based and hospital outpatient clinics. Health Services Research [epub ahead of print]. doi:10.1111/j.14756773.2010.01123.x.
McKinney, W. P., McIntire, D. D., Carmody, T. J., & Joseph, A. (1997). Comparing the smoking behavior of veterans and non-veterans. Public Health Reports, 112, 212–17.
Miller, D. R., Safford, M. M., & Pogach, L. M. (2004). Who has diabetes? Best estimates of diabetes prevalence in the Department of Veterans Affairs based on computerized patient data. Diabetes Care, 27(Suppl 2), B10–21.
Nelson, K. M. (2006). The burden of obesity among a national probability sample of veterans. Journal of General Internal Medicine, 21, 915–19.
Petersen, L. A., Byrne, M. M., Daw, C. N., Hasche, J., Reis, B., & Pietz, K. (2010). Relationship between clinical conditions and use of Veterans Affairs Health Care among Medicare-enrolled veterans. Health Services Research, 45, 762–91.
Randall, M., Kilpatrick, K. E., Pendergast, J. F., Jones, K. R., & Vogel, W. B. (1987). Differences in patient characteristics between Veterans Administration and community hospitals: Implications for VA planning. Medical Care, 25, 1099–1104.
Rosen, A. K., Gardner, J., Montez, M., et al. (2005). Dual-system use: are there implications for risk adjustment and quality assessment? American Journal of Medical Quality, 20, 182–194.
Salomon, J. A., Nordhagen, S., Oza, S., & Murray, C. J. L. (2009). Are Americans feeling less healthy? The puzzle of trends in self-rated health. American Journal of Epidemiology, 170, 343–51.
SPSS Inc., an IBM Company. (2010). Complex Samples Module v. 17.0 for Windows. Chicago: Author.
Stewart, A. L., Greenfield, S., Hays, R. D., et al. (1989). Functional status and well-being of patients with chronic conditions: Results from the medical outcomes study. JAMA, 262, 907–13.
Strine, T. W., Kroenke, K., Dhingra, S., et al. (2009). The associations between depression, health-related quality of life, social support, life satisfaction, and disability in community-dwelling adults. Journal of Nervous & Mental Disease, 197, 61–64.
U.S. Department of Health and Human Services. (2000). Healthy People 2010: Understanding and improving health (2nd ed.). Washington, DC: U.S. Government Printing Office.
Ware, J. E., & Sherbourne, C. D. (1992). The MOS 36-item short-form health survey (SF-36). Medical Care, 30, 473–83.
Wilson, D., Parsons, J., & Wakefield, M. (1999). The health-related quality of life of never smokers, ex-smokers, and light, moderate, and heavy smokers. Preventive Medicine, 29, 139–44.
Wolinsky, F. D., Coe, R. M., Mosely, R. R., & Homan, S. M. (1985). Veterans’ and nonveterans’ use of health services: a comparative analysis. Medical Care, 23, 1358–71.
Wolinsky, F. D., Miller, T. R., An, H., et al. (2006). Dual use of medicare and the Veterans Health administration: are there adverse health outcomes? BMC Health Services Research, 6, 131.
Wolinsky, F. D., An, H., Liu, L., et al. (2007). Exploring the association of dual use of the VHA and Medicare with mortality: separating the contributions of inpatient and outpatient services. BMC Health Services Research, 7, 70.
Acknowledgements
The views expressed are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Author information
Authors and Affiliations
Corresponding author
Additional information
The views expressed are those of the authors and do not necessarily represent the views of the Department of Veterans Affairs.
Rights and permissions
About this article
Cite this article
Howren, M.B., Cai, X., Rosenthal, G. et al. Associations of Health-Related Quality of Life with Healthcare Utilization Status in Veterans. Applied Research Quality Life 7, 83–92 (2012). https://doi.org/10.1007/s11482-011-9147-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11482-011-9147-5