Abstract
This study examines cigarette smoking trajectories from homelessness to housing and assesses demographic and clinical characteristics associated with multiple longitudinal smoking behavior patterns. Data were drawn from a longitudinal prospective cohort study of 421 adults experiencing homelessness who entered permanent supportive housing (PSH). Four quantitative surveys (baseline [while homeless], 3-, 6-, and 12 months post-housing) gathered participants’ smoking frequency used for Repeated Measure Latent Class Analysis (RMLCA), which identified subgroups that share longitudinal smoking behavior patterns. Baseline and time-varying demographic, mental health (e.g., schizophrenia), and substance use (e.g., cannabis use) measures were examined as correlates of class membership. RMLCA estimates supported a three-class model: (1) mixed-frequency decreasers (n = 71): who smoked at differing frequencies while demonstrating a significant decrease over time; (2) high-frequency maintainers (n = 194): participants who smoked daily/almost-daily and maintained this smoking rate across waves; and (3) low-frequency increasers (n = 56): participants who generally were non-smokers at baseline and significantly increased to monthly or weekly consumption longitudinally. Compared to Black and African American participants, Hispanic and Latino participants had greater odds of low-frequency increaser and mixed-frequency decreaser membership. Schizophrenia and bipolar disorder diagnoses increased odds of high-frequency maintainer membership compared to the two less-frequent-using subgroups. Cannabis use increased longitudinally and was associated with greater odds of high-frequency maintainer membership. This is the first study to find smoking changes from homelessness to housing. While encouraging that some residents reduce their smoking post-housing, many maintained high smoking rates. Cessation services that address mental health and co-occurring substance use within PSH are warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Cigarette smoking among adults experiencing homelessness is nearly five times that of housed adults (Soar et al., 2020). While homeless, this population faces a multitude of hindrances to smoking cessation, including the experience of homelessness itself and subsequent health and social deficits that accompany housing instability. High smoking rates are frequently attributed to clinical characteristics that typify adults experiencing homelessness, including poor mental health and high-risk substance use behaviors (Soar et al., 2020). Particularly, mental health conditions with psychotic features (e.g., schizophrenia and bipolar disorder) and post-traumatic stress disorder (PTSD), along with moderate to high-risk use of cannabis, illicit substances, and alcohol exacerbate smoking frequency for this population (Baggett et al., 2016; Harris et al., 2019a; Tsai & Rosenheck, 2012; Vijayaraghavan et al., 2016). Moreover, there is disproportionate representation of persons living in extreme poverty, Black and African American persons, and persons with lower levels of educational attainment within the homeless adult population (Henry et al., 2018; Soar et al., 2020); demographic characteristics correlated with increased smoking and reduced cessation (Businelle et al., 2013; Kulak et al., 2016; Soar et al., 2020).
Adults experiencing homelessness desire to cease smoking and make quit attempts at rates comparable to domiciled adults (Baggett et al., 2013; Businelle et al., 2013), yet their cessation outcomes have not been promising following intervention. Randomized controlled trials using counseling and pharmacotherapy while persons are experiencing homelessness report low quit rates (4–14%; Baggett et al., 2020, Burling et al., 2001; Okuyemi et al., 2013; Rash et al., 2018; Segan et al., 2015), and few have assessed abstinence beyond 8 weeks due to challenges retaining this population in clinical trials (Vijayaraghavan et al., 2020). Permanent supportive housing (PSH) is a leading solution to reducing homelessness through the provision of long-term, affordable housing and supportive services (Tsemberis, 2010). Housing is a potential facilitator of smoking cessation as it is a social determinant of health and can be a catalyst for health recovery and improved quality of life for homeless-experienced persons (Fitzpatrick-Lewis et al., 2011; Harris et al., 2019b; Henwood et al., 2014). While there are several studies identifying post-housing improvements to physical and mental health, which may show promise for post-housing smoking cessation outcomes (Fitzpatrick-Lewis et al., 2011; Harris et al., 2019b; Henwood et al., 2014), more rigorous evidence is needed to support the claim that PSH improves health (National Academies of Sciences, Engineering & Medicine, 2018).
This study responds to this need by examining changes in tobacco use from homelessness to housing, which, to date, has been largely unresearched. To the authors’ knowledge, there is only one previous study that examined changes in smoking from homelessness to housing; in a sample of homeless Veterans — a subset of which entered housing within the observation year — Tsai & Rosenheck, (2012) found no significant changes in smoking after 12 months (Tsai & Rosenheck, 2012). This work is distinct from that of Tsai and Rosenheck in two prominent ways: a portion of their cohort entered housing whereas the total sample from the current study entered PSH, and their study assessed smoking changes in aggregate while ours identifies multiple patterns of smoking behavior over time. Such studies outlining differential smoking patterns are well-aligned with smoking pattern variation documented in representative, longitudinal studies with the general adult population (Choi et al., 2019; Lee et al., 2022), providing enhanced detail and granularity via the opportunity to assess etiological factors that correlate with each smoking behavior pattern.
This study is the first to use repeated measures of smoking frequency to identify trajectories of smoking behavior in the transition from homelessness to housing. Specifically, this study draws upon four waves of data from a cohort of adults who were homeless at baseline, and across their initial year in PSH in Los Angeles. By grouping participants based on their shared smoking behavior patterns over time, this study is also enabled to examine demographic and clinical characteristics associated with multiple smoking trajectories. Understanding differential smoking trajectories that occur when homeless adults are housed and identifying characteristics driving behavior change patterns is critical for targeting subpopulations of tobacco users and tailoring efforts accordingly to overcome cessation barriers for this highly vulnerable population.
Methods
Data for this study were drawn from a longitudinal prospective cohort study designed to understand clinical, behavioral, and social changes in the transition from homelessness to PSH. Participants were recruited between 2014 and 2016 via collaborations with 26 agencies that constitute most supportive housing providers in Los Angeles County (LAC). Participants were eligible if they were 39 years old or older, spoke English or Spanish, and were currently homeless, unaccompanied adults (without minor children). The minimum age of 39 (thereby turning 40 during the course of the study) was chosen to reduce variability attributed to differing developmental stages within the life course. Given the emphasis on addressing chronic homelessness, individuals in PSH increasingly tend to be older and unaccompanied (Henry et al., 2018). Persons experiencing homelessness are typically placed into supportive housing in LAC through housing-, social service-, or hospital-appointed staff. The Vulnerability Index Service Prioritization Decision Assistance Tool is used to assess health and risk status and designed to prioritize placement of the most vulnerable persons into supportive housing (United Way Greater Los Angeles, 2016).
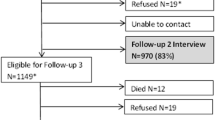
At baseline, while experiencing homelessness, 421 adults were recruited to participate in quantitative and social network surveys 1–1.5 hours in length, conducted in English or Spanish, and led by trained interviewers using iPads. Follow-up surveys were conducted at 3 months (n = 405; 96% retention), 6 months (n = 400; 95% retention), and 12 months (n = 383; 91% retention) post-housing entry. Interviewers maintained contact with participants between interviews via monthly phone calls. Although participants who were not interviewed at a midpoint wave were eligible for later interviews, there was some attrition due to death, incarceration, withdrawal, and loss of contact. Participants completed written informed consent prior to participation. All study procedures were approved by the University of Southern California institutional review board. Additionally, the study received a US Department of Health and Human Services certificate of confidentiality to protect participant data from subpoena.
Measures
Tobacco Use
Past-3-month smoking frequency, assessed at each wave, was used as the repeated indicator of latent class membership. Drawn from the National Institute on Drug Abuse-Modified Alcohol, Smoking and Substance Involvement Screening Test (NIDA-Modified ASSIST)—which is well-regarded for its accuracy of self-reported substance use, good to excellent sensitivity and specificity, and excellent test–retest reliability (McNeely et al., 2014; Zgierska et al., 2014)—inquired whether respondents used substances never, once or twice, monthly, weekly, or daily/almost-daily in the past 3 months (National Institute on Drug Abuse, 2009). If participants reported past-3-month smoking, a separate question on the NIDA-Modified ASSIST asked whether they had “tried and failed to control, cut down, or stop smoking” (National Institute on Drug Abuse, 2009). A dichotomous indicator of past-3-month cessation attempt was subsequently created for each wave.
Demographic Characteristics
Demographic characteristics included age, gender, race and ethnicity, education, Veteran status, lifetime literal homelessness, and income (California Health Interview Survey, 2014). A combined measure of race and ethnicity was created for analyses, leading to four subgroups: Black and African American, Non-Hispanic White, Hispanic and Latino, and Other (Native American, Alaska Native, Asian, Native Hawaiian, Pacific Islander, or Multiracial). Race and ethnicity terms used follow the response options used in the study survey and the US Department of Housing and Urban Development. Four participants identified as male-to-female transgender and were subsequently combined with the female subgroup for analytic purposes. Education captured total years of scholarship; completion of high school was equivalent to 12 years of education, and each year of post-high school education (e.g., vocational, trade school, and college) was subsequently added. Veteran status indicated whether participants served in any branch of the U.S. military. Participants’ lifetime history of unsheltered homelessness (i.e., staying outside on the streets, park, or beach; in an abandoned building, garage, shed, indoor public place, car, truck, van, or recreational vehicle; on a bus, subway, or train; or in a shelter) prior to PSH was assessed in years (U.S. Department of Housing and Urban Development, 2015).
All demographic characteristics were assessed at baseline except for past-30-day income from all sources (i.e., jobs, tips, welfare, general relief, governmental assistance, illegal activities, and under-the-table payments), which was assessed across each wave.
Mental Health
At baseline, an adapted measure (Parsons, 2014) assessed self-reported lifetime histories of mental health conditions (i.e., schizophrenia, major depressive disorder, bipolar disorder, anxiety, and PTSD) diagnosed by a mental health provider or other healthcare professional with response options informed by prior literature (Bassuk et al., 1998; Hwang, 2001; Wenzel, 2009). At each wave, participants’ past-month overall psychological functioning was assessed using the Modified Colorado Symptom Index; a cutoff score of 16 indicated the presence of a psychiatric disability (Boothroyd & Chen, 2008).
Substance Use
The NIDA-Modified ASSIST determined participants’ use of cannabis and illicit substances (cocaine, methamphetamine, hallucinogens, and street opioids [i.e., heroin and opium]) at each wave (National Institute on Drug Abuse, 2009). Participants who endorsed use of stimulant, sedative, or opioid prescriptions were asked a follow-up question about misuse of each type of prescription (Al-Tayyib et al., 2014; Rice, 2011). For analyses, illicit substances from the NIDA-Modified ASSIST were combined with prescription misuse indicators to determine any illicit substance use.
A National Institute on Alcohol Abuse and Alcoholism adapted item assessed past-3-month binge drinking at each survey (National Institute on Alcohol Abuse, 2003). Binge drinking was defined as consuming at least four (for women) or five (for men) alcoholic drinks during a 2-hour period (National Institute on Alcohol Abuse, 2003). Respondents who reported any past-3-month binge drinking were considered positive for binge drinking.
Analysis
Repeated Measures Latent Class Analysis (RMLCA) was used to determine subgroups that reflect distinct patterns of smoking change in the transition from homelessness to housing. Smoking frequency at each wave (baseline, 3, 6, and 12 months post-housing), totaling four variables, served as the RMLCA item indicators. The analysis was restricted to participants who reported using tobacco at least once across the four assessments, given our interest in identifying smoking trajectories. This resulted in 321 participants (76.24%) who served as the analytic sample. To determine the number of subgroups, or classes, estimations for one to four classes were conducted. Determination of the best model fit was based on several fit indexes: the Akaike information criterion, Bayesian information criteria, Lo-Mendell-Rubin likelihood ratio test, and latent class entropy and interpretability (Collins & Lanza, 2009). Missing data in RMLCA are treated using a missing at random assumption and are handled using the Mplus full information maximum likelihood estimation procedure (Muthén & Muthén, 1998). All models and model comparisons were conducted using Mplus version 8.0.
An RMLCA is ideal for these data and the aims of this study for several reasons. This statistical approach can garner new information about multiple patterns of smoking behavior longitudinally by grouping participants that share similar patterns (Collins & Lanza, 2009). RMLCA allows for the determination of latent patterns using categorical items and identifies proportions expected for each class, resting on the assumption of conditional independence; that is, the latent variable explains all variation between the repeated measures of smoking frequency used to identify each class (Collins & Lanza, 2009). Built up latent class modeling, like RMLCA, is considered a person-centered approach and is particularly valuable over variable-centered approaches, like mixed-effects modeling, which aggregates persons into a single group and examines them as a collective set of independent (i.e., predictor) and dependent variables (Collins & Lanza, 2009). We also conducted a mixed-effects model with a logit function using the same variables the RMLCA uses (time and smoking frequency) to determine whether there was a significant effect of time on smoking changes when participants were aggregated. By comparing the mixed-effects logit model and RMLCA results, we sought to highlight RMLCA’s value—that it offers a more granular understanding of longitudinal smoking behavior and enhances the ability to target cessation efforts by identifying multiple cigarette smoking trajectories and determining the characteristics serving as correlates to each longitudinal smoking pattern.
Following the identification of classes, we examined demographic characteristics, clinical characteristics, and cessation attempts associated with class membership using multinomial logistic regression. To account for time-variant predictors (i.e., income, psychological functioning, and substance use measures), distributed lag models were used. Distributed lag modeling is suitable for time-series data, wherein time-varying explanatory measures are fitted to the person levels and are regressed to predict person-level latent classes (Gasparrini & Leone, 2014). Each time-variant measure at baseline (T0) was modeled simultaneously with a change score that captured differences between baseline and final follow-up scores of that variable (T1; 12 months post-baseline). Predictor variables were initially assessed individually in univariable, unadjusted models with class membership serving as the multinomial categorical dependent variable. Comparisons of the smaller latent classes were made to the largest latent class (one vs. two, one vs. three). All univariable associations significant at p < 0.10 were subsequently analyzed in multivariable multinomial logistic regression models, which included all demographic control variables (regardless of demographics’ statistical significance in univariable models). In multivariable models, statistical significance was determined by p < 0.05. Mental health and substance use measures were examined in separate multivariable models due to collinearity of measures. All multinomial logistic regression models were conducted using Stata version 16.
Results
Participants
Across all participants who reported smoking during the study (N = 321), the average age was 54.54 years (SD = 7.21; range: 39–79). The sample was predominantly male (74.14%), and more than half were Black and African American (57.01%). On average, residents had 1 year of post-high school education (SD = 3.68) and approximately a third (31.15%) had military service experience. Participants experienced an average of 6.38 years of literal homelessness across their lifetime. The most prevalent mental health diagnosis reported was depression (57.01%).
Regarding time-varying measures—at baseline, the total sample reported an average of $565.41 (SD = $352.92) in monthly income and there was an approximate increase of $62 in past-month income 12 months post-housing (p < 0.01). Cannabis use was reported by 31.97% while participants were homeless, with the odds of cannabis use increasing by 2.03 at 6 months (p = 0.02) and 1.83 at 12 months (p = 0.04) post-housing. Baseline illicit substance use was reported by 22.12% with 45% lower odds at the 6-month follow-up (OR = 0.55, p = 0.04). Smoking cessation attempts were reported by 39.09% at baseline, with 33% lower odds of attempting cessation 12 months post-housing (OR = 0.67, p = 0.05). Table 1 presents descriptive statistics and changes in time-variant measures for the total sample and across each latent class.
RMLCA
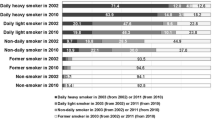
An assessment of fit indexes, model parameters of class membership probabilities, and gamma parameters of latent class prevalence revealed a three-class model best fit the data. Classes were labeled and described as (1) mixed-frequency decreasers (n = 71): residents who smoke at differing frequencies at baseline while demonstrating a significant decrease in smoking over time (β = − 0.28, p = 0.01, 95% CI = − 0.49, − 0.07); (2) high-frequency maintainers (n = 194): participants who smoked daily/almost-daily and maintained this smoking rate across waves (β = − 0.04, p = 0.18, 95% CI = − 0.10, 0.02); and (3) low-frequency increasers (n = 56): a subset of participants who were generally non-smokers at baseline and significantly increased their smoking to monthly or weekly consumption longitudinally (β = 0.13, p = 0.03, 95% CI = 0.01, 0.24). See Table 2 for a summary of model indexes and model comparisons. Figure 1 depicts the proportions of past 3-month smoking frequencies across latent classes and assessment waves and Fig. 2 depicts average smoking frequencies and linear trajectories of smoking across each latent class.
Comparison of RMLCA to Mixed-Effects Modeling
The authors sought to compare RMLCA results to a mixed-effects model: a more commonly used statistical approach that assesses participants in aggregate. The mixed-effects model with a logit function indicated that, when examining the total sample of tobacco-using participants together, smoking frequency significantly declined over time (β = − 0.07, SE = 0.03, p = 0.03).
Multinomial Logistic Regression – Univariable and Multivariable Models
All univariable model associations (Table 3) significant at p < 0.10 were retained for analyses in multivariable models (Table 4). With high-frequency maintainers serving as the reference group, results indicated Hispanic and Latino participants were 3.10 times as likely to be members of the mixed-frequency decreasers class (p < 0.01) and 2.97 times as likely to be members of the low-frequency increasers class, compared to Black and African American participants (p = 0.03). There were three clinical characteristics significant in univariable models, which were examined in separate multivariable models with demographic controls. Participants with schizophrenia had 56% reduced odds of low-frequency increaser membership (OR = 0.44, p = 0.03), while participants with a bipolar disorder diagnosis had 51% reduced odds of mixed-frequency maintainer membership (OR = 0.49, p = 0.03) and 56% reduced odds of low-frequency increaser membership (OR = 0.44, p = 0.01), indicating a greater prevalence of participants with these conditions in the high-frequency maintainers class. A change in cannabis use was associated with 62% reduced odds (OR = 0.38, p = 0.02) of being a low-frequency increaser in multivariable analyses, indicating high-frequency maintainers had a greater likelihood of baseline cannabis use and of increasing their cannabis use over time. Due to small cell size, low-frequency increasers were omitted from the model examining cessation attempts as a predictor of class membership; no significant difference in cessation attempts was detected between high-frequency maintainers and mixed-frequency decreasers.
Discussion
This study identified smoking frequency trajectories among a sample of adults experiencing homelessness who transitioned to PSH in Los Angeles. Of three identified latent classes, two classes were characterized by behavior change; one class increased their smoking, and one class decreased their smoking over time. The third class, who smoked daily, maintained their smoking behavior over time. When we conducted a mixed-effects logit model to compare to RMLCA results, we found that, when aggregated, the sample demonstrated significant decreases in smoking over time. Our results from this sample differ from Tsai and Rosenheck’s work, which did not find significant change in smoking in a cohort of Veterans in a supportive housing program, a portion who entered PSH (Tsai & Rosenheck, 2012). While our mixed-effects model finding a change in smoking from homelessness to housing is novel itself, it nonetheless highlights the importance of an RMLCA approach, which allowed trends in smoking change and maintenance to be parsed out. Specifically, RMLCA identified two integral target groups of tobacco-using residents: the low-frequency increasers, who may benefit from brief smoking cessation and prevention efforts in the nascent months of housing to thwart uptake or increased smoking frequency, and the high-frequency maintainers whose daily smoking maintenance over time likely necessitates more intensive cessation treatments and efforts.
RMLCA also enabled the examination of factors associated with class membership, which bolstered identification of characteristics that define each class. The sole demographic correlate of class membership was race and ethnicity, with more membership of Hispanic and Latino participants in low-frequency increaser and mixed-frequency decreaser classes compared to Black and African American participants. National and state-level data suggest Hispanic and Latino adults smoke less frequently compared to other racial and ethnic groups (Bandiera et al., 2016). Although mechanisms underlying these differences are less known, collectivism and connection to cultural identity may be protective in Hispanics and Latinos’ smoking behavior risk, as it has been for other health behaviors (Bandiera et al., 2016). For example, Latino subpopulations’ sense of community is protective against experiences of discrimination, which is tied to increased smoking frequency among racial minority subgroups (Ai et al., 2014). Discrimination, in addition to low socioeconomic status, high stress levels, living in food deserts, and use of mentholated cigarette brands, are common among Black and African American persons and are considered barriers to cessation (Brondolo et al., 2015; Kulak et al., 2016); such barriers may be at play in the high proportion of Black and African American participants in the high-frequency maintainers class. Future research would benefit from a deeper qualitative exploration of the role of race and ethnicity in PSH residents’ smoking behavior and cessation.
Poor mental health—specifically severe conditions characterized by psychotic features or chronic mood dysregulation—is believed to be a primary reason for high smoking rates among persons experiencing homelessness (Baggett et al., 2016; Harris et al., 2019a, b; Soar et al., 2020; Tsai & Rosenheck, 2012; Vijayaraghavan et al., 2016). In this study, bipolar disorder and schizophrenia were correlates of class membership, indicating high-frequency maintainers had significantly more members with these conditions than the two lower-risk classes. Research supports increased smoking risk among adults with these conditions: a meta-analysis of world-wide studies found persons with schizophrenia who smoke cigarettes have increased odds of heavy smoking, high nicotine dependence, and lower cessation rates (De Leon & Diaz, 2005), while a systematic review of adults with bipolar disorder indicates smoking initiation is two to three times higher, and cessation initiation and maintenance is less likely to occur, compared to individuals without bipolar disorder (Heffner et al., 2011).
For persons with more severe psychiatric conditions, smoking may be used as a mechanism of self-medicating, i.e., using a substance to reduce the effects of an undesired emotional state attributed to their diagnoses or antipsychotic medications (Gehricke et al., 2007). In particular, for persons with bipolar disorder, smoking may be a means to reduce negative affect during depressive episodes and enhance cognitive functioning during episodes of mania (Heffner et al., 2011). Bipolar disorder and schizophrenia are known to co-occur with other risk factors and health considerations, including suicidal ideation, co-occurring substance abuse, mood fluctuation, low social support, and lengthier hospital stays making smoking cessation an increased challenge (Heffner et al., 2011; Ostacher et al., 2006). Having bipolar or schizophrenia may also enhance exposure to social and environmental settings where smoking is pervasive and condoned, even by treatment staff or case managers (Heffner et al., 2011; Prochaska, 2011). These mental health conditions commonly elicit cautionary practices among providers, including a lower likelihood of prescribing smoking cessation medications (Taylor et al., 2020)—often out of concern cessation medications may worsen mental health or inhibit psychotropic medication effectiveness—despite research suggesting they are generally safe for this population and that quitting smoking positively affects mood regulation (Evins et al., 2021; Prochaska, 2011; Taylor et al., 2020). Though some aspects of mental health undoubtedly make cessation more challenging, the presence of a psychotic condition does not diminish readiness to quit or attempts at cessation (Prochaska, 2011). Incorporating cessation treatment into mental health treatments has proven to be an effective approach for promoting long-term smoking abstinence; one that may be particularly beneficial for PSH residents (Prochaska, 2011).
Across the sample, cannabis use increased over time and this change was associated with a greater likelihood of high-frequency maintainer class membership, when compared to the low-frequency increasers. This likely indicates participants who smoke cigarettes frequently also use cannabis frequently (Agrawal et al., 2012), rather than their substituting cannabis for tobacco; a topic worth exploring in future research as the significant decrease in illicit drug use over time may suggest harm reduction processes are involved in these relationships. Data for the present study were collected prior to Los Angeles’ increase in cigarette taxation effective in 2017; however, cannabis dispensaries had become commonplace prior to the legalization of cannabis effective in 2018 (Goldstein & Sumner, 2019). In other states where legalization and recreational cannabis use has been established, increased rates of tobacco and cannabis use have been observed (Wang & Cataldo, 2016). For a high-risk population like PSH residents, cannabis use can seem secondary to concerns with illicit substance use; however, in the context of improving cessation outcomes, more attention to this relationship may be needed.
Limitations
This study comes with limitations. Smoking frequency was reported using the NIDA Modified ASSIST which is not a fine-grain assessment of smoking frequency; the use of a different measure, such as number of cigarettes per day, may result in different latent classes. Mental health and substance use measures were self-reported which may increase bias, although this population’s self-reported health information has demonstrated high internal consistency and healthcare utilization has demonstrated good concurrent validity, even among chronically homeless persons with risky substance use (Conrad et al., 2001). E-cigarette usage and noncombustible cannabis routes of administration were not widely popular during the study observation period and may impact current smoking trajectories for this population. Additionally, these data draw from Los Angeles-based residents, and environmental factors not explored in this study may affect residents’ smoking differentially in other regions. Last, this study did not assess whether providers intervened on PSH residents’ smoking or if participants engaged in any cessation interventions; though it should be noted that cigarette smoking has been coined “the neglected addiction” for this population, with prior research suggesting providers place smoking cessation as lower priority to their other acute health and mental health needs (Baggett et al., 2013).
Conclusion
While this was the first study to find post-housing smoking reductions, use of RMLCA demonstrated this was applicable to a portion of PSH residents, and the largest portion of tobacco-using participants smoked daily and maintained this smoking frequency over time. As interventions for smoking have faced challenges to improve cessation outcomes while adults are experiencing homeless, this study may offer insight into future experimental designs that examine whether housing itself is a catalyst for smoking reductions. These findings also highlight the great need for implementation of smoking cessation services within PSH. Efforts that address both mental health symptoms and co-occurring substance use, in conjunction with smoking cessation are warranted. This includes support with management of mental health symptomatology and incorporating smoking into PSH harm reduction practices. Additionally, adapting cessation interventions to incorporate racial and cultural factors related to residents’ smoking may advance the much-needed improvements in cessation outcomes for this highly disadvantaged population .
References
Agrawal, A., Budney, A. J., & Lynskey, M. T. (2012). The co-occurring use and misuse of cannabis and tobacco: A review. Addiction, 107, 1221–1233.
Ai, A. L., Aisenberg, E., Weiss, S. I., & Salazar, D. (2014). Racial/ethnic identity and subjective physical and mental health of Latino Americans: An asset within? American Journal of Community Psychology, 53, 173–184.
Al-Tayyib, A. A., Rice, E., Rhoades, H., & Riggs, P. (2014). Association between prescription drug misuse and injection among runaway and homeless youth. Drug and Alcohol Dependence, 134, 406–409.
Baggett, T. P., Lebrun-Harris, L. A., & Rigotti, N. A. (2013). Homelessness, cigarette smoking and desire to quit: results from a US national study. Addiction, 108, 2009–2018. among homeless-experienced adults.
Baggett, T. P., Campbell, E. G., Chang, Y., Magid, L. M., & Rigotti, N. A. (2016). Posttraumatic stress symptoms and their association with smoking outcome expectancies among homeless smokers in Boston. Nicotine & Tobacco Research, 18, 1526–1532.
Baggett, T. P., Chang, Y., Yaqubi, A., McGlave, C., Higgins, S. T., & Rigotti, N. A. (2018). Financial incentives for smoking abstinence in homeless smokers: A pilot randomized controlled trial. Nicotine and Tobacco Research, 20(12), 1442–1450.
Bandiera, F. C., Assari, S., Livaudais-Toman, J., & Pérez-Stable, E. J. (2016). Latino and Black smokers in the Health and Retirement Study are more likely to quit: The role of light smoking. Tobacco Induced Diseases, 14, 1–6.
Bassuk, E. L., Buckner, J. C., Perloff, J. N., & Bassuk, S. S. (1998). Prevalence of mental health and substance use disorders among homeless and low-income housed mothers. American Journal of Psychiatry, 155, 1561–1564.
Boothroyd, R. A., & Chen, H. J. (2008). The psychometric properties of the Colorado Symptom Index. Administration and Policy in Mental Health and Mental Health Services Research, 35, 370–378.
Brondolo, E., Monge, A., Agosta, J., Tobin, J. N., Cassells, A., Stanton, C., & Schwartz, J. (2015). Perceived ethnic discrimination and cigarette smoking: Examining the moderating effects of race/ethnicity and gender in a sample of Black and Latino urban adults. Journal of Behavioral Medicine, 38, 689–700.
Burling, T. A., Seidner Burling, A., & Latini, D. (2001). A controlled smoking cessation trial for substance-dependent inpatients. Journal of Consulting and Clinical Psychology, 69(2), 295.
Businelle, M. S., Cuate, E. L., Kesh, A., Poonawalla, I. B., & Kendzor, D. E. (2013). Comparing homeless smokers to economically disadvantaged domiciled smokers. American Journal of Public Health, 103, S218–S220.
California Health Interview Survey. (2014). CHIS 2011–2012 Adult Questionnaire Version 10.3 (U. C. f. H. P. Research, Trans.) Regents of the University of California.
Choi, K., Chen, J. C., Tan, A. S., Soneji, S., & Moran, M. B. (2019). Receipt of tobacco direct mail/email discount coupons and trajectories of cigarette smoking behaviours in a nationally representative longitudinal cohort of US adults. Tobacco Control, 28(3), 282–288.
Collins, L. M., & Lanza, S. T. (2009). Latent class and latent transition analysis: With applications in the social, behavioral, and health sciences. John Wiley & Sons.
Conrad, K. J., Yagelka, J. R., Matters, M. D., Rich, A. R., Williams, V., & Buchanan, M. (2001). Reliability and validity of a modified Colorado Symptom Index in a national homeless sample. Mental Health Services Research, 3, 141–153.
De Leon, J., & Diaz, F. J. (2005). A meta-analysis of worldwide studies demonstrates an association between schizophrenia and tobacco smoking behaviors. Schizophrenia Research, 76, 135–157.
Evins, A. E., West, R., Benowitz, N. L., Russ, C., Lawrence, D., Mcrae, T., Maravic, M. C., Heffner, J. L., & Anthenelli, R. M. (2021). Efficacy and safety of pharmacotherapeutic smoking cessation AIDS in schizophrenia spectrum disorders: Subgroup analysis of eagles. Psychiatric Services, 72, 7–15.
Fitzpatrick-Lewis, D., Ganann, R., Krishnaratne, S., Ciliska, D., Kouyoumdjian, F., & Hwang, S. W. (2011). Effectiveness of interventions to improve the health and housing status of homeless people: A rapid systematic review. BMC Public Health, 11, 1–14.
Gasparrini, A., & Leone, M. (2014). Attributable risk from distributed lag models. BMC Medical Research Methodology, 14, 1–8.
Gehricke, J. G., Loughlin, S. E., Whalen, C. K., Potkin, S. G., Fallon, J. H., Jamner, L. D., ... & Leslie, F. M. (2007). Smoking to self-medicate attentional and emotional dysfunctions. Nicotine & tobacco research, 9(Suppl_4), S523-S536.
Goldstein, R., & Sumner, D. (2019). California cannabis regulation: An overview. California Agriculture, 73, 101–102.
Harris, T., Winetrobe, H., Rhoades, H., & Wenzel, S. (2019a). The role of mental health and substance use in homeless adults’ tobacco use and cessation attempts. Journal of Dual Diagnosis, 15, 76–87.
Harris, T., Rhoades, H., Duan, L., & Wenzel, S. L. (2019b). Mental health change in the transition to permanent supportive housing: The role of housing and social networks. Journal of Community Psychology, 47(8), 1834–1849.
Heffner, J. L., Strawn, J. R., DelBello, M. P., Strakowski, S. M., & Anthenelli, R. M. (2011). The co-occurrence of cigarette smoking and bipolar disorder: Phenomenology and treatment considerations. Bipolar Disorders, 13(5–6), 439–453.
Henry, M., Mahathey, A., Morrill, T., Robinson, A., Shivji, A. & Watt, R. (2018). The 2018 Annual Homeless Assessment Report (AHAR) to Congress, Part 1: Point-in-Time Estimates of Homelessness. https://www.wpr.org/sites/default/files/2018-ahar-part-1-compressed.pdf
Henwood, B. F., Matejkowski, J., Stefancic, A., & Lukens, J. M. (2014). Quality of life after housing first for adults with serious mental illness who have experienced chronic homelessness. Psychiatry Research, 220, 549–555.
Hwang, S. W. (2001). Homelessness and Health. Cmaj, 164, 229–233.
Kulak, J. A., Cornelius, M. E., Fong, G. T., & Giovino, G. A. (2016). Differences in quit attempts and cigarette smoking abstinence between whites and African Americans in the United States: Literature review and results from the International Tobacco Control US Survey. Nicotine & Tobacco Research, 18, S79–S87.
Lee, B., Levy, D. E., Macy, J. T., Elam, K. K., Bidulescu, A., & Seo, D. C. (2022). Smoking trajectories from adolescence to early adulthood as a longitudinal predictor of mental health in adulthood: Evidence from 21 years of a nationally representative cohort. Addiction, 117(6), 1727–1736.
Mcneely, J., Strauss, S. M., Wright, S., Rotrosen, J., Khan, R., Lee, J. D., & Gourevitch, M. N. (2014). Test–retest reliability of a self-administered Alcohol, Smoking and Substance Involvement Screening Test (ASSIST) in primary care patients. Journal of Substance Abuse Treatment, 47, 93–101.
Muthén, L.K. and Muthén, B.O., (1998). Mplus user’s guide. Los Angeles. CA: Muthén & Muthén, 2017.
National Academies of Sciences, Engineering, and Medicine. (2018). Permanent supportive housing: Evaluating the evidence for improving health outcomes among people experiencing chronic homelessness.
National Institute on Alcohol Abuse and Alcoholism. (2003). Recommended alcohol questions. National Institute on Alcohol Abuse and Alcoholism [cited 2021 Mar 16]. Available from: http://www.niaaa.nih.gov/research/guidelines-and-resources/recommended-alcohol-questions
National Institute on Drug Abuse. (2009). Screening for drug use in general medical settings: a resource guide for providers. Available at: http://www.nida.nih.gov/nidamed/screening/. Accessed 1 May 2021
Okuyemi, K. S., Goldade, K., Whembolua, G. L., Thomas, J. L., Eischen, S., Sewali, B., Guo, H., Connett, J. E., Grant, J., Ahluwalia, J. S., & Resnicow, K. (2013). Motivational interviewing to enhance nicotine patch treatment for smoking cessation among homeless smokers: A randomized controlled trial. Addiction, 108(6), 1136–1144.
Ostacher, M. J., Nierenberg, A. A., Perlis, R. H., Eidelman, P., Borrelli, D. J., Tran, T. B., Ericson, G. M., Weiss, R. D., & Sachs, G. S. (2006). The relationship between smoking and suicidal behavior, comorbidity, and course of illness in bipolar disorder. Journal of Clinical Psychiatry, 67, 1907–1911.
Parsons, V. L. (2014). Design and estimation for the national health interview survey, 2006-2015 (No. 2014). US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics.
Prochaska, J. J. (2011). Smoking and mental illness—breaking the link. New England Journal of Medicine, 365, 196–198.
Rash, C. J., Petry, N. M., & Alessi, S. M. (2018). A randomized trial of contingency management for smoking cessation in the homeless. Psychology of Addictive Behaviors, 32, 141.
Rice, E. (2011). HIV risk in large social networks of homeless youth (Grant No. R01MH093336). National Institute of Mental Health.
Segan, C. J., Maddox, S., & Borland, R. (2015). Homeless clients benefit from smoking cessation treatment Delivered by a Homeless Persons’ Program. Nicotine & Tobacco Research, 17, 996–1001.
Soar, K., Dawkins, L., Robson, D., & Cox, S. (2020). Smoking amongst adults experiencing homelessness: A systematic review of prevalence rates, interventions and the barriers and facilitators to quitting and staying quit. Journal of Smoking Cessation, 15, 94–108.
Taylor, G. M., Itani, T., Thomas, K. H., Rai, D., Jones, T., Windmeijer, F., Martin, R. M., Munafò, M. R., Davies, N. M., & Taylor, A. E. (2020). Prescribing prevalence, effectiveness, and mental health safety of smoking cessation medicines in patients with mental disorders. Nicotine and Tobacco Research, 22, 48–57.
Tsai, J., & Rosenheck, R. A. (2012). Smoking among chronically homeless adults: Prevalence and correlates. Psychiatric Services, 63, 569–576.
Tsemberis, S. (2010). Housing First: ending homelessness, promoting recovery and reducing costs. How to house the homeless (pp. 37–56).
U.S. Department of Housing and Urban Development. (2015). Homeless Emergency Assistance and Rapid Transition to Housing (HEARTH): Defining “chronically homeless” final rule. Washington, DC. Retrieved from https://www.hudexchange.info/resources/documents/Defining-Chronically-Homeless-Final-Rule.pdf
United Way Greater Los Angeles. (2016). Greater Los Angeles Coordinated Entry System survey packet version 2.2. The Vulnerability Index‐Service Prioritization Decision Assistance Tool (VI‐SPDAT). Los Angeles, CA. http://ceslosangeles.weebly.com/uploads/1/2/2/1/1221685/ces-packet_2.2.pdf
Vijayaraghavan, M., Tieu, L., Ponath, C., Guzman, D., & Kushel, M. (2016). Tobacco cessation behaviors among older homeless adults: Results from the HOPE HOME study. Nicotine & Tobacco Research, 18, 1733–1739.
Vijayaraghavan, M., Elser, H., Frazer, K., Lindson, N., & Apollonio, D. (2020). Interventions to reduce tobacco use in people experiencing homelessness. Cochrane Database of Systematic Reviews, 2020(12), CD013413.
Wang, J. B., & Cataldo, J. K. (2016). Medical marijuana legalization and co-use in adult cigarette smokers. American Journal of Health Behavior, 40, 205–214.
Wenzel, S. (2009). Heterosexual HIV risk behavior in homeless men (Grant No. 1R01HD059307). Eunice Kennedy Shriver National Institute for Child Health.
Zgierska, A., Amaza, I. P., Brown, R. L., Mundt, M., & Fleming, M. F. (2014). Unhealthy drug use: How to screen, when to intervene. The Journal of Family Practice, 63, 524.
Funding
Open access funding provided by SCELC, Statewide California Electronic Library Consortium This study is supported a Ruth L. Kirschstein Predoctoral Individual National Research Service Award from the National Institute on Drug Abuse (F31DA045429-0) and the “Transitions to Housing” parent award (R01DA036345). This paper was developed as part of Dr. Harris’ 3-paper dissertation For the University of Southern California. Dr. Harris was supported by the VA Office of Academic Affiliations and the National Center on Homelessness Among Veterans to complete this work and prepare it for publication.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Consent to Participate
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (University of Southern California Institutional Review Board) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Written informed consent was obtained from all patients included in the study.
Competing Interests
Taylor Harris was supported by a Ruth L. Kirschstein Predoctoral Individual National Research Service Award from the National Institute on Drug Abuse (F31DA045429-0) and the “Transitions to Housing” parent award (R01DA036345). This paper was developed as part of Dr. Harris’ 3-paper dissertation For the University of Southern California. Dr. Harris was supported by the VA Office of Academic Affiliations and the National Center on Homelessness Among Veterans to complete and submit this work for publication. Sara Semborski has no relevant financial or non-financial interests to disclose. Jennifer Unger is a project leader and core leader on the USC Tobacco Center of Regulatory Science (TCORS). She serves on the national committee for the National Cancer Institute (NCI) Society for Research on Nicotine and Tobacco (SRNT) Tobacco-Related Health Disparities Network. Chi Ping Chou has no relevant financial or non-financial interests to disclose. Suzanne Wenzel was the Principal Investigator for the parent award for the current study. She received support from the National Institute on Drug Abuse (R01DA036345). The authors have no other conflicts of interest.
Disclaimer
The contents of this manuscript do not represent the views of the US Department of Veterans Affairs or the United States Government. The views expressed in this paper are those of the authors and do not reflect the official policy or position of the US Government.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Harris, T., Semborski, S., Unger, J. et al. Identifying Cigarette Smoking Trajectories from Homelessness to Housing. Int J Ment Health Addiction (2023). https://doi.org/10.1007/s11469-023-01106-x
Accepted:
Published:
DOI: https://doi.org/10.1007/s11469-023-01106-x