Abstract
Despite the recognition of compulsive sexual behavior (CSB) as a diagnostic entity in the ICD-11, few works have reported on its natural course. The aim of this study was to explore the natural course of CSB over a 1-year period, as well as to analyze the predictive power of different risk factors. A convenience sample of 154 young adults were assessed at baseline and after 1 year. Dimensionally, we found that scores on most CSB symptoms significantly decreased at 1 year (d between .20 and .35). On the contrary, severity of problematic use of online sexual activities increased (d = 0.22). Regression analyses revealed that sexual orientation (being bisexual) and religious beliefs (atheist) were significant predictors of the trajectory of CSB. However, after controlling for baseline levels of CSB, only openness to experience (β between − .167 and − .199), sexual sensation seeking (β between .169 and .252), anxiety (β = .363), and depression (β between .163 and .297) predicted an increased risk of CSB over time. Categorically, diagnostic consistency of CSB at 1 year was modest. These findings suggest that the natural course of CSB tends to be highly transient and inconsistent, and that classic risk factors for its occurrence have a limited predictive power over its natural course.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
No consensus exists on the appropriate diagnostic framework for compulsive sexual behavior (CSB), as evidenced by the myriad of terms employed to designate this clinical condition, the multiplicity of measures designed for its assessment, or the number of models proposed for its classification (Walton et al., 2017). In this context, the ICD-11 recognized CSB—operationalized as “Compulsive Sexual Behavior Disorder”—as an impulse-control disorder (Kraus et al., 2018), providing diagnostic guidelines and facilitating a common framework for its diagnosis (Stein et al., 2020). The ICD-11 characterizes CSB as a “persistent pattern of failure to control intense, repetitive sexual impulses or urges, resulting in repetitive sexual behaviour over an extended period that causes marked distress or impairment in personal, family, social, educational, occupational or other important areas of functioning” (Kraus et al., 2018, p. 109). The use of sex as a coping mechanism aimed to compensate for unpleasant affective states or stressful life events is often included as a core symptom of this condition as well (Kafka, 2010). As for its main manifestations, individuals with CSB often engage in multiple sexual activities, including excessive pornography use (typically accompanied by compulsive masturbation), casual sex with multiple partners, excessive engagement in paid sexual services, or compulsive sexual intercourse within a stable relationship (Reid et al., 2012a, 2012b; Wéry et al., 2016). CSB produces a significant personal and psychological distress (Reid et al., 2009), as well as problems on various aspects of daily living (McBride et al., 2008). As a result, individuals struggling with CSB often require psychiatric and/or psychological treatment to gain control over their sexual behavior (Derbyshire & Grant, 2015).
Despite this recognition of CSB as a diagnostic entity and a public health issue, there are few data about its phenomenology and clinical presentation (Kuzma & Black, 2008). This is especially true when it comes to drawing the natural course of CSB (i.e., the progression of its clinical presentation over time), a surprising gap given the obvious relevance of this feature for the characterization of psychopathology (Eaton, 2011). Therefore, the aim of this study was to explore the natural course of CSB over a 1-year period in a convenience sample of 154 young adults, as well as to analyze the predictive power of different risk factors over the trajectory of this condition.
Natural Course of CSB: Persistence Vs. Transience
Conventional wisdom about the natural course of CSB (mainly based on anecdotal reports, clinicians’ impressions, and/or data derived from retrospective studies with clinical samples) suggests that the onset of CSB usually occurs early in life (for most patients, during adolescence and young adulthood), gradually escalating over a period of months or years and remaining “chronic” when untreated. The DSM-5 field trial for hypersexual disorder (HD) supported these observations (Reid et al., 2012a, 2012b): after screening the clinical course of CSB in a sample of 152 patients seeking treatment for HD, this study found that 54.1% began experiencing symptoms before the age of 18. Most patients (82%) reported a gradual escalation over time, in front of the 17.4% that experienced an acute presentation of the condition (i.e., a rapid escalation between the onset of CSB and the symptom peak in a short period of time). As for the clinical course of CSB, this study found that patients were evenly divided into two categories: 48.6% of patients reporting a continuous presentation of the condition (i.e., having no periods of remission or oscillations of the symptoms severity since its onset) and 51.4% reporting an episodic presentation (i.e., the alternation of periods of fully—or partial—remission followed by systematic relapses). This study concluded that natural course of CSB tends to the continuity for some patients and to remission and relapse for others, but in both cases, to the persistence of the condition when left untreated.
The emphasis on the chronicity of CSB resonates with the widely held belief that addictive disorders are enduring for most people (McKay & Hiller-Sturmhöfel, 2010). As there has been increasing consideration of conceptualizing CSB as an addictive disorder (Kowalewska et al., 2018; Kraus et al., 2016; Stark et al., 2018), it seems reasonable to posit that chronicity would be a central feature of out-of-control sexual behavior as well. Indeed, a recent study using network analysis found that relapse was a central symptom of problematic pornography use (one of the most prominent manifestations of CSB) (Chen et al., 2021). However, findings from robust empirical studies have challenged the notion that chronicity characterizes addictions, suggesting that many people experience a decrease in the symptom severity and a natural recovery from substance use disorders (SUDs) over time (Carballo et al., 2007). Similarly, longitudinal studies exploring the natural course of different non-substance-related addictive behaviors (e.g., gaming and gambling) have found evidence of notable symptoms instability, as well as a significant proportion of long-term remissions (Gooding et al., 2022; Thege et al., 2015).
Given these new findings about the high transience of SUDs and non-substance-related addictive behaviors, exploring the potential instability of CSB symptoms over time is warranted. However, tracing the natural course of CSB (including trajectories of persistent remission and natural recovery) requires a complex methodological approach that goes beyond retrospective studies with clinical samples (Rumpf et al., 2007). As patients seeking—or receiving—treatment for CSB experience “active symptoms,” an obvious limitation of retrospective studies with clinical samples is that they explore the natural course of CSB in patients displaying a persistent presentation of the condition—either continuous or episodic—but not trajectories characterized by a transient course (i.e., the remission of CSB after its onset due to active coping, natural, or spontaneous recovery) (Dhuffar & Griffiths, 2016). Furthermore, retrospective data about the history and course of CSB provided by clinical patients may be influenced by recall biases (Shiffman et al., 2008) and self-perceived addiction severity (Grubbs et al., 2018a, 2018b). Finally, as argued by several clinicians and researchers, the private nature of sex, the stigma around out-of-control sexual behavior, and the low perception of severity of CSB may discourage patients with mild or moderate symptoms from seeking treatment (Kuzma & Black, 2008; Lindsay et al., 2021). As a result, patients that receive treatment for CSB—and participate in clinical studies, field trials, or constitutes the usual clientele of mental health professionals—likely represent the most severe cases, and not the whole continuum of severity in which this condition may be expressed. As some authors argue that CSB is likely to be less stable over time in patients with a less severe clinical presentation (Smith et al., 2014), it is plausible to believe that the natural history and course of CSB may differ in patients in the lower end or the middle of this severity continuum.
In the light of these limitations, prospective studies comprising multiple assessments over time are more suitable for exploring the natural course of CSB. So far, results from the few available longitudinal studies in the field have started to challenge the well-established notion of persistence of CSB, suggesting that its stability is notably lower than initially postulated. In a study among 258 male veterans, Smith et al. (2014) examined the longitudinal consistency of CSB diagnosis after 3 and 6 months of the initial assessment. These authors found that only 58% of participants diagnosed as sexually compulsives at baseline were identified as such at 3 months, and this figure dropped to 36% at 6 months. All in all, only 4% of those identified as sexually compulsives in one of the assessments presented the condition at all three time-points. Similarly, Štulhofer et al. (2020) conducted a longitudinal research to explore the consistency of CSB diagnosis in a sample of 262 male adolescents assessed with 5 months of difference. These authors found that only 37.5% of adolescents identified as problematic pornography users at baseline screened positive at follow-up. Furthermore, of 50 adolescents identified as sexually compulsives either at baseline or 5 months later, only 12 (i.e., 24%) met the cutoff for the diagnosis at both assessment’ points. Besides these studies with convenience samples, one study explored the natural course of CSB in a representative sample (Thege et al., 2015). These researchers used data from the Quinte Longitudinal Study (a cohort of 4121 Canadian adults assessed annually for a 5-year period) to analyze the temporal stability of six non-substance-related addictive behaviors (including CSB). Among the explored addictive behaviors, CSB was the most stable. Even so, CSB was predominantly transient (63.5% of those screening positive for CSB did so in one of the five follow-up assessments, whereas only 5.4% reported persistent CSB problems throughout all the study). This research also analyzed the dimensional course of CSB among those screening positive for CSB at the first study wave, finding a systematic decrease of its severity over time. Furthermore, these trends were consistent in both males and females, meaning that the transient nature of CSB diagnosis and the tendency towards the reduction of its severity over time did not differ according to gender. Only one prospective study obtained contrary results. Unlike previous research, in a 4-year longitudinal study with 572 college males, Thompson et al. (2015) found that scores on a scale assessing CSB remained relatively stable over time (1.52 at baseline vs. 1.47 at 4 years). Differences between this study and those listed before may be explained by the nature of the research sample: whereas previous studies comprised adolescents (Štulhofer et al., 2020) or predominantly adult populations (Smith et al., 2014; Thege et al., 2015), Thompson et al. (2015) assessed young adults (as demonstrated by previous studies, the age period in which potentially compulsive behaviors—e.g., pornography use—are more prevalent [Ballester-Arnal et al., 2021]). For this reason, young adults (i.e., the sample assessed in this research) constitute a sample of high interest in the study of the natural course of CSB.
The Present Study
The purpose of the present study was to investigate the natural course of CSB over a 1-year period in a convenience sample of 154 young adults between 18 and 27 years old. As previous studies demonstrate (Reid et al., 2012a, 2012b), most patients (around 85%) report developing symptoms of CSB before or during their college years, meaning that this period is optimal for the analysis of the natural course of the condition during its first stages. When addressing the natural course of CSB, we combined a dimensional and a categorical approach to CSB: the former aimed to explore changes in the score on different indicators of CSB over time, whereas the later aimed to provide information on the diagnostic consistency of CSB. Combining these approaches, we captured the natural course of CSB according to the two predominant conceptualizations of CSB (either as a discrete category [Kraus et al., 2018] or as a continuum [Graham et al., 2016]). Consistent with most longitudinal studies conducted so far (Smith et al., 2014; Štulhofer et al., 2020; Thege et al., 2015), we expect to find a decrease in CSB scores over time (dimensional approach) and a low diagnostic consistency between the two study waves (categorical approach).
Furthermore, as suggested by Eaton (2011), risk factors may have differential effects on the different stages of a psychiatric condition (i.e., on their onset, duration, and/or clinical course). In the field of CSB, a notable research effort has been invested on exploring risk factors associated with the onset (i.e., occurrence) of this condition (Castro-Calvo et al., 2020), but whether these factors impact on its natural course is yet to be tested. For this reason, a second aim of this study was to explore the predictive power of well-documented risk factors for CSB over the longitudinal trajectory of this condition. Given prior literature linking CSB to gender (Grubbs et al., 2019), religiousness (Bradley et al., 2016), age (Reid et al., 2012a, 2012b), sexual orientation (Bőthe et al., 2018), personality (Efrati et al., 2022), sexual sensation seeking (Kalichman & Rompa, 1995), anxiety (Grant-Weinandy et al., 2022), depression (Schultz et al., 2014), and self-esteem (Chaney & Burns, 2015), we included these variables as predictors of the longitudinal trajectory of CSB at 1 year. In particular, we expect to find that gender (male), religiousness (practicing believer), age ( +), sexual orientation (homosexual or bisexual), personality (extraversion [ +], neuroticism [ +], and conscientiousness [-]), sexual sensation seeking ( +), anxiety ( +), depression ( +), and self-esteem (-) would be associated with increased longitudinal risk of CSB at 1 year.
Materials and Methods
Participants and Procedure
Participants were assessed twice: at baseline (T1) and 1 year after the initial assessment (T2). Data acquisition for the 1st study wave was conducted as a part of a larger data collection effort examining the sociodemographic, sexual, and clinical profile of young people with and without CSB (for more information on the study methods, see Castro-Calvo et al., 2020). In brief, participants were recruited at T1 using a street intercept survey method. Junior members from the research team set an information table in the main entrance of different higher education centers, actively approaching potential participants. Those who accepted to participate, provided informed consent, fulfilled a brief paper-and-pencil survey to assess their eligibility, and were then cited to complete an individual in-office assessment. A total of 1581 individuals between 18 and 27 years old participated in the study at T1. At 1 year (T2), 200 participants in the first study wave were randomly selected and recontacted by mail to take part in a follow-up survey. According to our a priori calculus, this sample size would let us identify average differences in CSB scores between study waves (d = 0.50) and low-to-medium regression coefficients when predicting the trajectory of CSB over time with appropriate statistical power (α = 0.05; power [1-β] = 0.95). Furthermore, the random selection of participants at T2 prevented potential biases in participant selection and increased the representativity of the final sample. Of the invited participants, 154 (77%) accepted to take part in the second study wave and completed a new in-office assessment. As the aim of this research was to explore the longitudinal evolution of CSB, participants that completed the study at baseline but who did not participate in the follow-up were excluded. Therefore, the definitive study sample comprised 154 participants (80 men; 74 women) assessed at both T1 and T2. Participants’ characteristics at baseline (T1) are displayed in Table 1.
The study procedures were carried out in accordance with the Declaration of Helsinki. The Institutional Review Board of the Jaume I University approved the study.
Measures
Sociodemographic Data (T1)
At baseline, participants were asked to report their gender, age, whether they were engaged or not in a stable relationship, sexual orientation, and religious beliefs.
Offline and Online Sexual Behavior (T1)
Participants reported basic aspects of their sexual behavior such as (a) whether they had ever engaged in sexual intercourse with a sex partner (yes/no); (b) lifetime number of sexual partners; (c) frequency of sexual activity (1 = less than six times per year; 7 = more than three times per week); and (d) average time spent per week on online sexual activities (in minutes). These ad hoc questions were answered at T1.
Compulsive Sexual Behavior (T1 and T2)
CSB was assessed at both baseline and 1 year later using the “composite index of CSB symptoms” (Castro-Calvo et al., 2020), an empirically derived index resulting from the selection of 41 items from three previously validated scales: the Hypersexual Behavior Inventory (HBI, Ballester-Arnal et al., 2019 [Spanish version]; Reid et al., 2011 [original version]), the Sexual Compulsivity Scale (SCS, Ballester-Arnal et al., 2013 [Spanish version]; Kalichman & Rompa, 1995 [original version]), and the Sexual Addiction Screening Test (SAST, Carnes, 1983 [original version]; Castro-Calvo et al., 2018 [Spanish version]). The composite index of CSB symptoms assessed the following subscales: (a) impaired control over sexual behavior; (b) neglecting health, personal care or other interests, activities, and responsibilities due to sexual behavior; (c) repetitive but unsuccessful efforts to control or reduce sexual fantasies, urges, or behaviors; (d) continued engagement despite interference; (e) use of sex to cope with unpleasant emotional states; and (f) preoccupation, salience, and self-perceived sexual problems. In the initial validation study (Castro-Calvo et al., 2020), reliability for this composite index ranged between 0.67 and 0.89 (paper-and-pencil format) and 0.68 and 0.91 (online version). In subsequent studies (Ballester-Arnal et al., 2020; Castro-Calvo et al., 2022), reliability for the total score (α = 0.93–0.95) and subscales (α between 0.67 and 0.89) remained appropriate. As for its validity, findings derived from these studies supported the usefulness of this composite index to distinguish between individuals with and without CSBD. In the present study, scale reliability at T1 (αtotal score = 0.94; αsubscales = 0.67–0.89) and T2 (αtotal score = 0.95; αsubscales = 0.77–0.92) was appropriate.
Participants also completed the “Internet Sex Screening Test” (ISST, Ballester-Arnal et al., 2010 [Spanish version]; Delmonico et al., 2003 [original version]), a scale focused on measuring compulsive engagement in online sexual activities. Cronbach’s alpha in the 1st and 2nd study waves was 0.84 and 0.83, respectively.
Personality (T1)
The Spanish adaptation of the “NEO Personality–Revised” (NEO PI-R, Cordero et al., 2008) was used to assess participants’ personality profile at baseline. The NEO PI-R comprises 240 items designed to measure personality according to the Five Factor Model (FFM). For the sake of parsimony, in the current study, we utilized the T score on the five global domains of personality (namely neuroticism, extraversion, openness, agreeableness, and conscientiousness) rather than scores on the six specific facets comprising each factor.
Sexual Sensation Seeking (T1)
At T1, participants completed the Spanish adaptation of the “Sexual Sensation Seeking Scale” (SSSS, Ballester-Arnal et al., 2018 [Spanish version]; Kalichman & Rompa, 1995 [original version]), an 11-item scale assessing the propensity to attain optimal levels of sexual excitement and to engage in novel sexual experiences. In this study, internal consistency was 0.83.
Anxiety and Depression (T1)
At baseline, current presence and severity of depression and trait/state anxiety were assessed through the Spanish version of the “Beck Depression Inventory” (BDI-II, Beck et al., 2011) and the “State-Trait Anxiety Inventory” (STAI, Spielberger et al., 2002). Cronbach’s alpha for the BDI-II, the STAI-Trait, and the STAI-State was 0.90, 0.91, and 0.90, respectively.
Self-esteem (T1)
Self-esteem was measured at T1 through the Spanish version of the “Rosenberg Self-Esteem Scale” (RSES, Martín-Albo et al., 2007), a unidimensional 10-item scale assessing general self-esteem. In the present study, Cronbach’s alpha (0.89) was excellent.
Data Analysis
All analyses—except for the estimation of Cohen’s d—were carried out using the SPSS statistic package (version 26.0). First, to explore the natural course of CSB from a “dimensional” approach, we conducted paired samples t tests to compare participants’ scores on the composite index of CSB symptoms and the ISST at T1 and T2. To test the effect size of the differences between the two study waves, Cohen’s d was computed (G*Power [version 3.1]). Effect sizes of about 0.20 were considered small, close to 0.50 moderate, and greater than 0.80 large (Cohen, 1988).
By subtracting the score obtained at T1 from the score at T2, we estimated an indicator of increased/decreased risk of out-of-control sexual behavior at 1 year (labelled “ΔM”). The sign and size of the resulting figure indicated the direction and the degree of the changes (positive scores indicated increased risk at the follow-up, whereas negative scores indicated the contrary). This “risk score” was then employed as dependent variable in two-step linear regressions (stepwise method) to analyze the predictive power of different independent variables measured at T1. In order to test how our key variables (i.e., sociodemographic data, personality, sexual sensation seeking, anxiety, depression, and self-esteem) predicted the longitudinal trajectory of CSB, in the first step, we entered our independent variables of interest. In the second step, we included baseline levels of CSB in order to test if these variables of interest remained significant when predicting the longitudinal trajectory of CSB when baseline levels of compulsivity were statistically controlled.
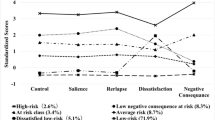
Finally, we analyzed diagnostic trajectories of CSB by comparing the proportion of participants above the clinical threshold at T1 and T2. Through this “categorical” approach, we identified four possible profiles: (a) participants without clinical scores at T1 and T2; (b) participants with clinical scores at T1 and T2; (c) participants with clinical scores at T1 but not at T2; and (d) participants without clinical scores at T1 but meeting the cut-off at T2.
Results
Natural Course of CSB at 1 Year and Predictive Power of Different Key Variables
Table 2 compares average scores at T1 and T2 on the composite index of CSB symptoms and the ISST. With the exception of the coping subscale (t = 1.49; p = 0.136), participants’ scores on the composite index of CSB symptoms significantly decreased at 1 year after the initial assessment. Effect sizes of the differences between study waves were small to moderate (d between 0.20 and 0.35). On the contrary, scores on the scale assessing problematic use of online sexual activities (i.e., the ISST) increased, on average, by 0.67 points (t = − 2.79; p = 0.006; d = 0.22).
To test the relationship between the longitudinal trajectory of CSB and the key variables assessed in this research, participants’ score on the variable “ΔM” (estimated for each subscale from the composite index of CSB symptoms and for the ISST) was correlated (Pearson’s r) with the other study measures (Table 3).
As shown in Table 3, longitudinal trajectories of CSB according to the different subscales from the composite index of CSB symptoms and the ISST were all related consistently and positively to each other (r between 0.124 and 0.764). However, we did not find a consistent pattern of correlations between trajectories of CSB and the other study measures. Among included personality domains, openness was associated negatively with the risk of CSB at one year (r = − 0.186; p = 0.021 [composite index total score]; r = − 0.213; p = 0.008 [coping]; r = − 0.173; p = 0.033 [ISST]), whereas neuroticism (r = 0.167; p = 0.038 [coping]) and conscientiousness (r = 0.211; p = 0.009 [neglect]; (r = 0.172; p = 0.033 [continued engagement]) were correlated positively. Finally, increased longitudinal risk according to the coping’s subscale correlated with higher scores on depression (r = 0.213; p = 0.009) and anxiety (r = 0.275; p = 0.001 [trait]; r = 0.201; p = 0.014 [state]).
Table 4 summarizes the results from the two-step linear regressions predicting longitudinal trajectories of CSB at one year. During the first step of each analysis, the explained variance of the resulting models was moderate to low (R2 between 2.7 and 19.7%) and the predictive power of the independent variables was limited. Being bisexual and atheist predicted the decrease in the longitudinal risk of CSB at 1 year according to different indicators. As for personality, openness to experience measured at T1 was related to a longitudinal reduction of coping symptoms (β = − 0.194) and to a reduction in the risk of problematic use of OSA (β = − 0.213). Sexual sensation seeking was a significant predictor of the increase in symptoms of impaired control over time (β = 0.181). Finally, anxiety showed a contradictory predictive pattern: at the same time, increased scores on trait anxiety were related to increased coping symptoms over time (β = 0.285), but also to an increase in the ability to stop out-of-control sexual behavior (β = -0.238). In the second step, upon entry of baseline CSB scores, most of the previously significant relationships between sexual orientation, religious beliefs, and the longitudinal trajectories of CSB were no longer significant. On the contrary, a clear pattern emerged between higher scores on sexual sensation seeking and depression and increased longitudinal risk in different CSB domains. Contrary to initial hypotheses, baseline levels of CSB and its longitudinal course over time were negatively associated (β between − 0.275 and − 0.638); in other words, participants scoring higher on CSB at baseline showed a systematic decrease in the risk for out-of-control sexual behavior at one year. As a result, explained variance of the regression models notably increased (R2 between 7.7 and 32.9%).
Diagnostic Trajectories of CSB at 1 Year
To explore the diagnostic trajectories of CSB at 1 year, we estimated the proportion of participants meeting the clinical threshold for the diagnosis of out-of-control sexual behavior at T1 and T2 (Table 5). As the composite index of CSB symptoms lacks a cutoff score for the diagnosis of this condition, participants were classified according to the SCS, HBI, SAST, and ISST cutoff scores. Most participants (between 87 and 98.7% depending on the scale) were classified as non-clinical at both T1 and T2. In contrast, the proportion of “new diagnoses” (i.e., participants without clinical scores at T1 but meeting the cut-off at T2) ranged between 0.7 and 6.5%. Of those scoring above the SCS cut-off score at T1 (i.e., 7.1%), around half (3.9%) remained in the same diagnostic category one year after the initial assessment, whereas the other 3.2% were no longer identified as potentially sexually compulsive (i.e., their condition was transient). Similarly, 5.2% of participants initially identified as clinical according to the HBI at T1 also scored above the threshold at T2, compared to the 3.9% that did not meet the cut-off at T2. As for the SAST, the prevalence of participants with clinical scores at T1 and T2 was 1.3%, in front of the 3.9% that scored above the threshold at T1 but not at T2. Finally, only 0.7% of the participants were classified as problematic users of online sexual activities at T1 according to the ISST, and all of them remained scoring above the clinical cut-off at T2.
Discussion
The main aim of the present study was to explore the natural course of CSB over a 1-year period in a convenience sample of young adults. When addressing this aim, we combined a dimensional and a categorical approach to CSB in order to capture the two predominant conceptualizations of out-of-control sexual behavior (Graham et al., 2016; Kraus et al., 2018). Dimensionally, participants experienced a systematic decrease in most CSB scores over time. Categorically, diagnostic consistency of CSB at 1 year was modest (between 43 and 75% of participants identified as sexually compulsives at baseline did not meet the threshold at 1 year). These findings are consistent with our hypothesis and prior literature suggesting that the natural course of CSB in community samples is characterized by a notable instability (Smith et al., 2014; Štulhofer et al., 2020; Thege et al., 2015).
Given that our sample comprised individuals in transition from late adolescence to young adulthood, mostly without clinical levels of out-of-control sexual behavior, this decline in CSB severity and the modest diagnostic consistence between study waves may be explained by normal processes of psychological and sexual maturation (e.g., reduction of impulsivity levels [Collado et al., 2014], age-related variations in sexual hormones associated with sexual arousal [Bancroft, 2005], and change of personal circumstances—such as the initiation of a stable relationship—that inhibits opportunities to engage in CSB [Garcia et al., 2012]). According to this view, certain age-related features associated with heightened levels of sexual experimentation and sexual risk-taking behaviors that are par for the course of young adulthood (e.g., the “sexual hookup culture” [Garcia et al., 2012]) would explain the decremental tendency of CSB scores over time. This speculation is supported by the fact that sexual sensation seeking predicted the trajectory of CSB at 1 year: in particular, we found that participants showing increased tendencies towards sexual excitement and novel sexual experiences were more prone to experience symptoms of excessive and uncontrolled sexual behavior over time, a finding that resonates with previous literature linking sexual sensation seeking and CSB (Castro-Calvo et al., 2020; Kalichman & Rompa, 1995). Whereas the influence of natural age-related transitions is a plausible explanation for the decremental course of CSB over time in non-clinical populations, this hypothesis seems less valid when explaining the low diagnostic consistency in individuals with clinical levels of CSB. In these individuals, the documented tendency to natural recovery may be associated with the severity of the clinical condition. As some authors argue that CSB is likely to be less stable over time in patients with a less severe clinical presentation (Smith et al., 2014), another compatible explanation is that our participants, even those meeting the threshold for the diagnosis of CSB, presented a mild or moderate severity. All in all, these results suggest that individuals with low or moderate levels of CSB will be more likely to experience a natural reduction of symptoms of out-of-control sexual behavior over time.
Collectively, these findings bear implications for the diagnosis of CSB. As the natural course of CSB in the transition between late adolescence and young adulthood tend to be inconsistent (at least, among non-treatment seekers), clinicians should take special precautions in order to prevent false positives diagnosis (i.e., the diagnosis of this condition in people experiencing symptoms of CSB—even meeting clinical thresholds—but with a probable longitudinal trajectory of natural recovery). In these cases, the accurate assessment of personal distress and other serious consequences associated with CSB may be of crucial importance when it comes to distinguishing normal experiences of heightened sexual desire from actual cases of CSB (Kafka, 2013).
That said, we found two exceptions to this decline of CSB symptoms over time. First, the use of sex as a coping mechanism remained stable at 1 year, probably because unlike other CSB symptoms, this feature is not per se problematic and many individuals without CSB show an increase in their sexual arousal while anxious or depressed (Bancroft et al., 2003). Even more notably, scores on the ISST (i.e., the scale assessing problematic use of online sexual activities) increased at 1 year. As this rise was not followed by a proportional increase in the percentage of participants meeting the threshold for the diagnosis of online sexual compulsivity (note that only one participant—0.7% of the sample—met the criteria for the diagnosis of problematic use of online sexual activities), it would be the result of the increasing accessibility and proliferation of the use of the Internet for sexual purposes (Ballester-Arnal et al., 2021), rather than an actual indicator of increased severity over time. This conclusion goes in line with the results reported by Smith et al. (2014): these authors found that whereas CSB remained stable 4 years after the baseline assessment, pornography use (in general, not particularly focused on problematic use) significantly increased.
Over a 1-year period, the greatest predictor of the longitudinal trajectory of CSB was baseline levels of CSB. However, contrary to our initial hypothesis and literature (Grubbs et al., 2018a, 2018b), baseline levels of CSB and its longitudinal course over time were negatively associated (i.e., higher CSB scores at T1 predicted a longitudinal trajectory of descendent CSB risk). This finding reinforces and extends the conclusion outlined before about the transience of CSB, further indicating that individuals with greater initial levels of CSB experience a more pronounced reduction in its severity over time. Well-stablished risk factors for CSB such as sexual orientation (bisexuality) or religious beliefs (atheist) showed moderate associations with the reduction in the risk of CSB over time in the initial steps of regression analyses, but were no longer relevant after controlling for baseline levels of CSB. Even more, other variables (such as gender or self-esteem) were not correlated at all with the longitudinal trajectory of CSB, thus suggesting that traditional risk factor for the occurrence of out-of-control sexual behavior barely predicts its natural course over time. This conclusion goes in line with previous studies reporting a limited predictive power of individual differences over the longitudinal expression of problematic pornography use (Grubbs et al., 2018a, 2018b). In contrast, there were more consistent links between anxiety/depression, sexual sensation seeking, and the trajectory of CSB at 1 year, even after controlling for baseline levels of CSB. We also noted that openness to experience was the only personality domain related (negatively) to the longitudinal trajectory of CSB, a finding that resonates with studies linking lower scores on this facet to infidelity and promiscuity (Schmitt, 2004) or alcohol symptoms (Grekin et al., 2006). However, previous studies on the personality profile linked to CSB showed inconsistent or not significant associations between this facet and out-of-control sexual behavior (Efrati et al., 2022), once again indicating that factors leading to the occurrence of a psychopathology and predicting its natural course often differ (Eaton, 2011).
As for the implications of the study findings, previous literature has suggested different ways in which characterizing the natural course of psychopathology may advance its management (see Maisto et al., 2014). First, information about how CSB symptoms change over time can influence the general conceptualization and nosological status of the condition (for instance, supporting its recognition as a diagnostic entity or upholding a particular diagnostic framework). As noted before, CSB constitutes a condition with a disputed nosological status (Potenza et al., 2017), and some have even called into question its recognition as a clinical condition (Moser, 2013). In this line, the relative consistency of CSB diagnosis for a subset of patients diagnosed as sexually compulsives (between 25 and 57% of those diagnosed at T1) means that, for some patients, this condition remains stable and impacts on their daily living over time, thus warranting its recognition as a diagnostic entity in its own right. Furthermore, the compatibility of our findings with those observed for substance (Carballo et al., 2007) and non-substance-related addictive behaviors (Thege et al., 2015) may support the suitability of the addiction framework for the conceptualization of CSB, although confirming this point requires further research and more direct evidence. Second, the knowledge of the factors predicting a positive or negative clinical course may help to design preventive interventions (for instance, by manipulating factors leading to trajectories of natural recovery) or inform treatment decisions (by focusing interventions on factors leading to more favorable treatment outcomes—such as trajectories of long-term remission). To date, there is an obvious lack of preventive interventions for CSB (Gola & Potenza, 2018) and available treatments are focused on a myriad of therapeutic targets (Efrati & Gola, 2018). Our study revealed that certain psychological dispositions, anxiety or depression, or sexual dispositional traits, sexual sensation seeking, predicts long-term trajectories of CSB, and may therefore constitute important therapeutic targets for the treatment of CSB. This finding may also explain why psychological interventions aimed to promote healthy emotion regulation strategies through mindfulness-based interventions (Blycker & Potenza, 2018), cognitive-behavioral therapy, or cognitive analytic therapy (Efrati & Gola, 2018) are showing promising results in reducing CSBD symptoms. Finally, the characterization of the natural course of a condition may aid in evaluating the efficacy and effectiveness of a treatment by providing a reference for the expected evolution of the condition (Scott et al., 2008). As revealed in our study, symptoms of CSB tend to decline over time, an aspect that should be considered when rating the relative efficacy of new therapeutic approaches compared to the expected declining trajectory when left untreated.
This study is not without limitations. First, participants were assessed only twice. Longitudinal studies comprising two assessments are limited when it comes to yielding valid inferences about the clinical course of CSB, as at least three data points are recommendable to depict the chronic relapsing pattern that may characterize a substantial proportion of individuals with lifetime out-of-control sexual behavior in long-term prospective studies (Dawson, 2013). Second, the limited sample size prevents us to provide definitive conclusions on the natural course of CSB. This is especially true for the findings related to the diagnostic consistency of CSB, where some subgroups of participants (e.g., participants with clinical scores at T1 and T2 or with clinical scores at T1 but not at T2) comprised a low sample size. Third, participants were not asked to report whether they sought psychological and/or psychiatric treatment for CSB between T1 and T2 (an aspect that may impact the trajectory of CSB scores and the diagnostic consistency) (Dhuffar & Griffiths, 2016). At a methodological level, the lack of reliable and valid clinical thresholds for the identification of CSB through the composite index of CSB symptoms prevented us to conduct our dimensional and categorical analytic approach on the basis of the same assessment indices; instead, we relied on the cutoff score of different screening scales for the identification of patients with CSB. Finally, our sample was recruited from the general community. Even when some participants (between 1.3 and 13%) met the clinical threshold for the diagnosis of CSB either at T1 or T2, we recommend that future work examine the natural course of CSB also in populations seeking treatment. Despite these limitations, the present research represents a step forward to trace the natural course of CSB, as well as the factors impacting on its long-term trajectory, through a robust methodological approach (including longitudinal data derived from well-stablished measures to assess CSB and combining a dimensional and a categorical approach).
Data Availability
Data are available on justified request to the first author or corresponding author.
References
Ballester-Arnal, R., Gil-Llario, M. D., Gómez-Martínez, S., & Gil-Juliá, B. (2010). Psychometric properties of an instrument for assessing cyber-sex addiction. Psicothema, 22(4), 1048–1053.
Ballester-Arnal, R., Gómez-Martínez, S., Gil-Llario, M. D., & Salmerón-Sánchez, P. (2013). Sexual compulsivity scale: Adaptation and validation in the Spanish population. Journal of Sex & Marital Therapy, 39(6), 526–540. https://doi.org/10.1080/0092623X.2012.665816
Ballester-Arnal, R., Ruiz-Palomino, E., Espada, J. P., Morell-Mengual, V., & Gil-Llario, M. D. (2018). Psychometric properties and validation of the sexual sensation seeking scale in Spanish adolescents: Brief screening method for use in research and clinical practice. Personality and Individual Differences, 122, 47–54. https://doi.org/10.1016/J.PAID.2017.10.006
Ballester-Arnal, R., Castro-Calvo, J., Gil-Juliá, B., Giménez-García, C., & Gil-Llario, M. D. (2019). A validation study of the Spanish version of the Hypersexual Behavior Inventory (HBI): Pencil and paper versus online administration. Journal of Sex & Marital Therapy, 45(4), 283–302.
Ballester-Arnal, R., Castro-Calvo, J., Giménez-García, C., Gil-Juliá, B., & Gil-Llario, M. D. (2020). Psychiatric comorbidity in compulsive sexual behavior disorder (CSBD). Addictive Behaviors, 107, 106384. https://doi.org/10.1016/j.addbeh.2020.106384
Ballester-Arnal, R., Castro-Calvo, J., García-Barba, M., Ruiz-Palomino, E., & Gil-Llario, M. D. (2021). Problematic and non-problematic engagement in online sexual activities across the lifespan. Computers in Human Behavior, 120, 106774. https://doi.org/10.1016/j.chb.2021.106774
Bancroft, J. (2005). The endocrinology of sexual arousal. Journal of Endocrinology, 186, 411–427. https://doi.org/10.1677/joe.1.06233
Bancroft, J., Janssen, E., Strong, D., Carnes, L., Vukadinovic, Z., & Long, J. S. (2003). The relation between mood and sexuality in heterosexual men. Archives of Sexual Behavior, 32(3), 217–230. https://doi.org/10.1023/a:1023409516739
Beck, A. T., Steer, R. A., & Brown, G. K. (2011). BDI-II, Inventario de Depresión de Beck-II, Adaptación Española. Pearson.
Blycker, G. R., & Potenza, M. N. (2018). A mindful model of sexual health: A review and implications of the model for the treatment of individuals with compulsive sexual behavior disorder. Journal of Behavioral Addictions, 7(4), 917–929. https://doi.org/10.1556/2006.7.2018.127
Bőthe, B., Bartók, R., Tóth-Király, I., Reid, R. C., Griiths, M. D., Demetrovics, Z., & Orosz, G. (2018). Hypersexuality, gender, and sexual orientation: A large-scale psychometric survey study. Archives of Sexual Behavior, 47(8), 2265–2276. https://doi.org/10.1007/s10508-018-1201-z
Bradley, D. F., Grubbs, J. B., Uzdavines, A., Exline, J. J., & Pargament, K. I. (2016). Perceived addiction to internet pornography among religious believers and nonbelievers. Sexual Addiction and Compulsivity, 23(2–3), 225–243. https://doi.org/10.1080/10720162.2016.1162237
Carballo, J. L., Fernández-Hermida, J. R., Secades-Villa, R., Sobell, L. C., Dum, M., & García-Rodríguez, O. (2007). Natural recovery from alcohol and drug problems: A methodological review of the literature from 1999 through 2005. In H. Klingemann & L. Carter-Sobell (Eds.), Promoting self-change from addictive behaviors: Practical implications for policy, prevention, and treatment (pp. 87–101). Springer, Boston, MA. https://doi.org/10.1007/978-0-387-71287-1_5
Carnes, P. J. (1983). Out of the shadows: Understanding sexual addiction. CompCare Publishers.
Castro-Calvo, J., Ballester-Arnal, R., Billieux, J., Gil-Juliá, B., & Gil-Llario, M. D. (2018). Spanish validation of the sexual addiction screening test. Journal of Behavioral Addictions, 7(3), 584–600. https://doi.org/10.1556/2006.7.2018.57
Castro-Calvo, J., Gil-Llario, M. D., Giménez-García, C., Gil-Juliá, B., & Ballester-Arnal, R. (2020). Ocurrence and clinical characteristics of Compulsive Sexual Behavior Disorder (CSBD): A cluster analysis in two independent community samples. Journal of Behavioral Addictions, 9(12), 446–468. https://doi.org/10.1556/2006.2020.00025
Castro-Calvo, J., Giménez-García, C., García-Barba, M., Gil-Llario, M. D., & Ballester-Arnal, R. (2022). Atypical sexual interests in compulsive sexual behavior (CSB): Results from a phallometric study. Sexual Abuse. https://doi.org/10.1177/10790632221098358
Chaney, M. P., & Burns, C. M. (2015). Examining coming out, loneliness, and self-esteem as predictors of sexual compulsivity in gay and bisexual men. Sexual Addiction & Compulsivity, 22, 71–88. https://doi.org/10.1080/10720162.2014.1001543
Chen, L., Luo, X., Bőthe, B., Jiang, X., Demetrovics, Z., & Potenza, M. N. (2021). Properties of the Problematic Pornography Consumption Scale (PPCS-18) in community and subclinical samples in China and Hungary. Addictive Behaviors, 112, 2. https://doi.org/10.1016/j.addbeh.2020.106591
Cohen, J. (1988). Statistical power analysis for the behavioral sciences. Routledge: New York. https://doi.org/10.4324/9780203771587
Collado, A., Felton, J. W., MacPherson, L., & Lejuez, C. W. (2014). Longitudinal trajectories of sensation seeking, risk taking propensity, and impulsivity across early to middle adolescence. Addictive Behaviors, 39(11), 1580–1588. https://doi.org/10.1016/j.addbeh.2014.01.024
Cordero, A., Pamos, A., & Seisdedos, N. (2008). NEO PI-R, Revised Neo Personality Inventory (Spanish adaptation). TEA Ediciones.
Dawson, D. A. (2013). Commentary on Tuithof et al. (2013):mplications of the DSM-5 revision for the analysis of persistence/remission of alcohol use disorder. Addiction, 108(12), 2100–2101.
Delmonico, D. L., Miller, J., & Miller, J. A. (2003). The Internet Sex Screening Test: A comparison of sexual compulsives versus non-sexual compulsives. Sexual and Relationship Therapy, 18(3), 261–276. https://doi.org/10.1080/1468199031000153900
Derbyshire, K. L., & Grant, J. E. (2015). Compulsive sexual behavior: A review of the literature. Journal of Behavioral Addictions, 4(2), 37–47. https://doi.org/10.1556/2006.4.2015.003
Dhuffar, M. K., & Griffiths, M. D. (2016). Barriers to female sex addiction treatment in the UK. Journal of Behavioral Addictions, 5(4), 562–567. https://doi.org/10.1556/2006.5.2016.072
Eaton, W. W. (2011). Studying the natural history of psychopathology. In M. T. Tsuang, M. Tohen, & P. B. Jones (Eds.), Textbook in Psychiatric Epidemiology (Third Edit, pp. 183–198). John Wiley & Sons. https://doi.org/10.1002/9780470976739
Efrati, Y., & Gola, M. (2018). Treating compulsive sexual behavior. Current Sexual Health Reports, 10(2), 57–64. https://doi.org/10.1007/s11930-018-0143-8
Efrati, Y., Kraus, S. W., & Kaplan, G. (2022). Common features in compulsive sexual behavior, substance use disorders, personality, temperament and attachment—A narrative review. International Journal of Environmental Research and Public Health, 19(1), 296. https://doi.org/10.3390/ijerph19010296
Garcia, J. R., Reiber, C., Massey, S. G., & Merriwether, A. M. (2012). Sexual hookup culture: A review. Review of General Psychology, 16(2), 161–176. https://doi.org/10.1037/a0027911
Gola, M., & Potenza, M. N. (2018). Promoting educational, classification, treatment, and policy initiatives. Journal of Behavioral Addictions, 7(2), 208–210. https://doi.org/10.1556/2006.7.2018.51
Gooding, N. B., Williams, J. N., & Williams, R. J. (2022). Addiction chronicity: Are all addictions the same? Addiction Research & Theory, 0(0), 1–7. https://doi.org/10.1080/16066359.2022.2035370
Graham, F. J., Walters, G. D., Harris, D. A., & Knight, R. A. (2016). Is hypersexuality dimensional or categorical? Evidence from male and female college samples. The Journal of Sex Research, 53(2), 224–238. https://doi.org/10.1080/00224499.2014.1003524
Grant-Weinandy, J. T., Lee, B., Hoagland, K. C., Grubbs, J. B., & Bőthe, B. (2022). Anxiety and compulsive sexual behavior disorder : A systematic review. The Journal of Sex Research, 1–13. https://doi.org/10.1080/00224499.2022.2066616
Grekin, E. R., Sher, K. J., & Wood, P. K. (2006). Personality and substance dependence symptoms: Modeling substance-specific traits. Psychology of Addictive Behaviors, 20(4), 415–424. https://doi.org/10.1037/0893-164X.20.4.415
Grubbs, J. B., Wilt, J. A., Exline, J. J., & Pargament, K. I. (2018). Predicting pornography use over time: Does self-reported “addiction” matter? Addictive Behaviors, 82, 57–64. https://doi.org/10.1016/j.addbeh.2018.02.028
Grubbs, J. B., Wilt, J. A., Exline, J. J., Pargament, K. I., & Kraus, S. W. (2018). Moral disapproval and perceived addiction to internet pornography: A longitudinal examination. Addiction, 113(3), 496–506. https://doi.org/10.1111/add.14007
Grubbs, J. B., Kraus, S. W., & Perry, S. L. (2019). Self-reported addiction to pornography in a nationally representative sample: The roles of use habits, religiousness, and moral incongruence. Journal of Behavioral Addictions, 8(1), 88–93. https://doi.org/10.1556/2006.7.2018.134
Kafka, M. P. (2010). Hypersexual disorder: A proposed diagnosis for DSM-V. Archives of Sexual Behavior, 39(2), 377–400. https://doi.org/10.1007/s10508-009-9574-7
Kafka, M. P. (2013). The development and evolution of the criteria for a newly proposed diagnosis for DSM-5: Hypersexual disorder. Sexual Addiction & Compulsivity, 20(1–2), 19–26.
Kalichman, S. C., & Rompa, D. (1995). Sexual sensation seeking and sexual compulsivity scales: Reliability, validity, and predicting HIV risk behavior. Journal of Personality Assessment, 65(3), 586–601. https://doi.org/10.1207/s15327752jpa6503_16
Kowalewska, E., Grubbs, J. B., Potenza, M. N., Gola, M., Draps, M., & Kraus, S. W. (2018). Neurocognitive mechanisms in compulsive sexual behavior disorder. Current Sexual Health Reports, 10, 255–264. https://doi.org/10.1007/s11930-018-0176-z
Kraus, S. W., Voon, V., & Potenza, M. N. (2016). Should compulsive sexual behavior be considered an addiction? Addiction, 111(12), 2097–2106. https://doi.org/10.1111/add.13297
Kraus, S. W., Krueger, R. B., Briken, P., First, M. B., Stein, D. J., Kaplan, M. S., Voon, V., Abdo, C. H. N., Grant, J. E., Atalla, E., & Reed, G. M. (2018). Compulsive sexual behaviour disorder in the ICD-11. World Psychiatry, 17(1), 109–110. https://doi.org/10.1002/wps.20499
Kuzma, J. R., & Black, D. (2008). Epidemiology, prevalence, and natural history of compulsive sexual behavior. Psychiatric Clinics of North America, 31, 603–611. https://doi.org/10.1016/j.psc.2008.06.005
Lindsay, B. L., Bernier, E., & Szeto, A. C. H. (2021). An exploration on the public stigma of sexual addiction. Sexual Addiction and Compulsivity, 27(3–4), 293–321. https://doi.org/10.1080/10720162.2021.1904471
Maisto, S. A., Kirouac, M., & Witkiewitz, K. (2014). Alcohol use disorder clinical course research: Informing clinicians’ treatment planning now and in the future. Journal of Studies on Alcohol and Drugs, 75(5), 799–807. https://doi.org/10.15288/jsad.2014.75.799
Martín-Albo, J., Núñez, J. L., Navarro, J. G., & Grijalvo, F. (2007). The Rosenberg Self-Esteem Scale: Translation and validation in university students. The Spanish Journal of Psychology, 10(02), 458–467. https://doi.org/10.1017/S1138741600006727
McBride, K. R., Reece, M., & Sanders, S. A. (2008). Predicting negative outcomes of sexuality using the compulsive sexual behavior inventory. International Journal of Sexual Health, 19(4), 51–62. https://doi.org/10.1300/J514v19n04_06
McKay, J. R., & Hiller-Sturmhöfel, S. (2010). Treating alcoholism as a chronic disease: Approaches to long-term continuing care. Alcohol Research and Health, 33(4), 356–370.
Moser, C. (2013). Hypersexual Disorder: Searching for Clarity. Sexual Addiction & Compulsivity, 20(1–2), 48–58. https://doi.org/10.1080/10720162.2013.775631
Potenza, M. N., Gola, M., Voon, V., Kor, A., & Kraus, S. W. (2017). Is excessive sexual behaviour an addictive disorder? The Lancet Psychiatry, 4(9), 663–664. https://doi.org/10.1016/S2215-0366(17)30316-4
Reid, R. C., Carpenter, B. N., & Lloyd, T. Q. (2009). Assessing psychological symptom patterns of patients seeking help for hypersexual behavior. Sexual and Relationship Therapy, 24(1), 47–63. https://doi.org/10.1080/14681990802702141
Reid, R. C., Garos, S., & Carpenter, B. N. (2011). Reliability, validity, and psychometric development of the hypersexual behavior inventory in an outpatient sample of men. Sexual Addiction & Compulsivity, 18(1), 30–51. https://doi.org/10.1080/10720162.2011.555709
Reid, R. C., Carpenter, B. N., Hook, J. N., Garos, S., Manning, J. C., Gilliland, R., Cooper, E. B., McKittrick, H., Davtian, M., & Fong, T. (2012). Report of findings in a DSM-5 field trial for hypersexual disorder. The Journal of Sexual Medicine, 9(11), 2868–2877. https://doi.org/10.1111/j.1743-6109.2012.02936.x
Reid, R. C., Garos, S., & Fong, T. (2012). Psychometric development of the hypersexual behavior consequences scale. Journal of Behavioral Addictions, 1(3), 115–122. https://doi.org/10.1556/JBA.1.2012.001
Rumpf, H. J., Bischof, G., & John, U. (2007). Remission without formal help: New directions in studies using survey data. In H. Klingemann & L. Carter-Sobell (Eds.), Promoting Self-Change From Addictive Behaviors: Practical Implications for Policy, Prevention, and Treatment (pp. 73–85). Boston, MA: Springer. https://doi.org/10.1007/978-0-387-71287-1_4
Schmitt, D. P. (2004). The big five related to risky sexual behaviour across 10 world regions: Differential personality associations of sexual promiscuity and relationship infidelity. European Journal of Personality, 18(4), 301–319. https://doi.org/10.1002/per.520
Schultz, K., Hook, J. N., Davis, D. E., Penberthy, J. K., & Reid, R. C. (2014). Nonparaphilic hypersexual behavior and depressive symptoms: A meta-analytic review of the literature. Journal of Sex & Marital Therapy, 40(6), 477–487. https://doi.org/10.1080/0092623X.2013.772551
Scott, D. M., Williams, C. D., Cain, G. E., Kwagyan, J., Kalu, N., Ehlers, C. L., Hesselbrock, V., & Taylor, R. E. (2008). Clinical course of alcohol dependence in African Americans. Journal of Addictive Diseases, 27(4), 43–50. https://doi.org/10.1080/10550880802324754
Shiffman, S., Stone, A. A., & Hufford, M. R. (2008). Ecological momentary assessment. Annual Review of Clinical Psychology, 4, 1–32. https://doi.org/10.1146/annurev.clinpsy.3.022806.091415
Smith, P., Potenza, M., Mazure, C., McKee, S., Park, C., & Hoff, R. (2014). Compulsive sexual behavior among male military veterans: Prevalence and associated clinical factors. Journal of Behavioral Addictions, 3(4), 214–222. https://doi.org/10.1556/JBA.3.2014.4.2
Spielberger, C. D., Gorsuch, R. L., & Lushene, R. E. (2002). STAI: Cuestionario de Ansiedad Estado-Rasgo. Manual. (6a edición). TEA Ediciones.
Stark, R., Klucken, T., Potenza, M. N., Brand, M., & Strahler, J. (2018). A current understanding of the behavioral neuroscience of compulsive sexual behavior disorder and problematic pornography use. Current Behavioral Neuroscience Reports, 5(4), 218–231. https://doi.org/10.1007/s40473-018-0162-9
Stein, D. J., Szatmari, P., Gaebel, W., Berk, M., Vieta, E., Maj, M., de Vries, Y. A., Roest, A. M., de Jonge, P., Maercker, A., Brewin, C. R., Pike, K. M., Grilo, C. M., Fineberg, N. A., Briken, P., Cohen-Kettenis, P. T., & Reed, G. M. (2020). Mental, behavioral and neurodevelopmental disorders in the ICD-11: An international perspective on key changes and controversies. BMC Medicine, 18(21), 1–24. https://doi.org/10.1186/s12916-020-1495-2
Štulhofer, A., Rousseau, A., & Shekarchi, R. (2020). A two-wave assessment of the structure and stability of self-reported problematic pornography use among male Croatian adolescents. International Journal of Sexual Health, 32(2), 151–164. https://doi.org/10.1080/19317611.2020.1765940
Thege, B. K., Woodin, E. M., Hodgins, D. C., & Williams, R. J. (2015). Natural course of behavioral addictions: A 5-year longitudinal study. BMC Psychiatry, 15(1), 4. https://doi.org/10.1186/s12888-015-0383-3
Thompson, M. P., Kingree, J. B., Zinzow, H., & Swartout, K. (2015). Time-varying risk factors and sexual aggression perpetration among male college students. Journal of Adolescent Health, 57(6), 637–642. https://doi.org/10.1016/j.jadohealth.2015.08.015
Walton, M. T., Cantor, J. M., Bhullar, N., & Lykins, A. D. (2017). Hypersexuality: A critical review and introduction to the “sexhavior cycle.” Archives of Sexual Behavior, 46, 2231–2251. https://doi.org/10.1007/s10508-017-0991-8
Wéry, A., Vogelaere, K., Challet-Bouju, G., Poudat, F.-X., Caillon, J., Lever, D., Billieux, J., & Grall-Bronnec, M. (2016). Characteristics of self-identified sexual addicts in a behavioral addiction outpatient clinic. Journal of Behavioral Addictions, 5(4), 623–630. https://doi.org/10.1556/2006.5.2016.071
Funding
Open Access funding provided thanks to the CRUE-CSIC agreement with Springer Nature. This research was supported by grant P1.1B2012-49 and P1.1B2015-82 of the University Jaume I of Castellón and grant PSI2011-27992/11 I 384 of the Ministry of Science and Innovation (Spain).
Author information
Authors and Affiliations
Contributions
RBA and MDG contributed to study design, obtaining funding, and/or study supervision. JCC, CGG, and MGB participated in recruiting participants, collecting data, analysis/interpretation of data, and/or writing of the paper. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Castro-Calvo, J., Ballester-Arnal, R., Giménez-García, C. et al. Natural Course of Compulsive Sexual Behavior (CSB): a 1-Year Follow-up Study. Int J Ment Health Addiction (2023). https://doi.org/10.1007/s11469-023-01061-7
Accepted:
Published:
DOI: https://doi.org/10.1007/s11469-023-01061-7