Abstract
Few studies have examined panic attacks and social and demographic factors, amongst people who use methamphetamine. This study explores the prevalence and correlates of panic attacks amongst an Australian sample of 711 people who primarily smoke methamphetamine. Baseline data for this study was gathered from participants recruited from regional and metropolitan communities across Victoria, Australia, in an ongoing prospective cohort study. Sequential logistic regression was used to examine correlations between panic attacks and sociodemographic, mental health and methamphetamine use variables. Over one-third (36%) of participants reported experiencing a recent panic attack (within the last 4 weeks). The following characteristics were associated with an increased likelihood of panic attacks: being female [aOR 1.85, 95% CI 1.25, 2.60], younger (18–29 years) [aOR 1.82, 95% CI 1.16, 2.85], non-heterosexual [aOR 2.19, 95% CI 1.37, 3.49], having experienced interpersonal assault in the past 12 months [aOR 1.71, 95% CI 1.19, 2.45], being methamphetamine-dependent [aOR 1.78, 95% CI 1.22, 2.59] and reporting moderate to severe symptoms of anxiety [aOR 5.49, 95% CI 3.93, 7.69] and depression [aOR 3.98, 95% CI 2.86, 5.53]. Opportunities exist for health services to proactively engage and support this population when they present in distressed states, with a non-judgemental, trauma-informed approach.
Highlights
• It is estimated that over one third of people who smoke methamphetamine experience panic attacks.
• Methamphetamine smokers who are young, female and non-heterosexual are at increased risk of experiencing panic attacks.
• Presentations during mental distress are an opportunity for psychoeducation and harm reduction discussions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Methamphetamine is the most commonly used psychostimulant globally (Hurst, 2019) and is associated with increased risk of a range of mental health disorders including psychosis, depression and anxiety (Darke et al., 2008; Duncan et al., 2022; McKetin et al., 2019). Panic attacks are known to increase the risk of other psychiatric disorders and substance misuse (Goodwin & Hamilton, 2001). However, few, if any, studies have explored the experience of panic attacks in the context of methamphetamine use (Polcin et al., 2012).
Panic Attacks and Generalised Anxiety
Prevalence estimates for panic disorder in the USA and Australia are similar; respective lifetime prevalence estimates are 4.7% and 5.0% of the population with between 2.7 and 3.7% likely to experience panic disorder in any 12-month period (Harvard Medical School, 2007; Australian Bureau of Statistics (2022). Women are up to four times more likely to experience a panic attack than men (Eaton et al., 1994; McLean et al., 2011) and may experience different symptoms, more commonly reporting shortness of breath, choking and feeling smothered compared to male counterparts (Sheikh et al., 2002). As panic attack symptoms mimic cardiac conditions, people experiencing panic attacks frequently present to hospital emergency departments (EDs) numerous times before they seek support from a mental health service (Derrick et al., 2019).
Methamphetamine Use, Mental Health Difficulties
Rates of methamphetamine use in Australia are amongst the highest globally (Hurst, 2019) with 1.3% of the population aged over 14 years self-reporting meth/amphetamine use within the past 12 months (Australian Institute of Health and Welfare (2020)). While a recent Australian study found frequency of methamphetamine use and comorbid mental health disorders were associated with more frequent presentations to EDs (McKetin et al., 2018), no studies specifically report panic attacks in the context of ED presentations of people who use methamphetamine.
Predominantly, researchers have associated the experience of anxiety and panic with physiological effects of acute methamphetamine use and withdrawal, emphasising rates of use and dependence as key variables (e.g. Zweben et al., 2004) although some researchers have suggested a bidirectional hypothesis to describe the relationship between methamphetamine use and anxiety. Regardless, methamphetamine use intensifies risks of co-morbid psychiatric conditions and physiological illnesses (McKetin, et al., 2019).
Commonly, panic attacks occur within the context of an anxiety disorder. Co-morbid generalised anxiety disorder (GAD) and methamphetamine use is known to lead to poorer post-treatment outcomes across substance use and psychiatric domains, including increased risk of suicidality (Glasner-Edwards et al., 2010). While McKetin et al. (2019) failed to find evidence of a significant association between methamphetamine use disorder and anxiety, Duncan et al.’s (2022) findings identify a relationship between dependence and both depression and anxiety. A correlation between poor self-reported physical health was also found within the Duncan et al. (2022) study, substantiating well-established links between poor physical health and psychological distress (Gadalla, 2009). Treatment for co-existing methamphetamine dependence and anxiety is limited though, by a lack of efficacious pharmacological options compounded by poor medication adherence amongst people who use methamphetamine (Morley et al., 2017).
Depression is also common amongst people who use methamphetamine. McKetin et al. (2011) found 40% of people at intake to drug treatment services experienced depression in the past 12 months, and most (79%) met criteria indicating it was severe. While depressive symptoms can prompt help seeking (Kay-Lampkin et al., 2004), the implications are that substance use may be higher, the severity of psychosocial issues accompanying use may be more significant (Kay-Lambkin et al., 2011) and adherence to treatment can be poorer (Glasner-Edwards et al., 2008).
Psychosocial approaches have focused on harm reduction; however, barriers to treatment include service access, stigma and difficulty with engagement (Duncan et al., 2022; Glasner-Edwards et al., 2010). This existing literature suggests a potential relationship between anxiety (including panic attacks) and methamphetamine use, and further research is warranted to clarify how this manifests and for whom.
Environmental and Social Factors Linked to Methamphetamine Use
Social and environmental factors, particularly in early life, influence health outcomes across the lifespan, and are associated with substance use (Marshall et al., 2011). Experiences and motivations of methamphetamine use vary among people. Brecht et al. (2004) found experience of childhood sexual assault was significantly higher for women who used methamphetamine (44% compared to 24%), while males had markedly higher rates of arrest for criminal incidents. Across both genders, this study identified physical violence, suicide attempts and divorced parents to be prevalent, suggesting a variety of anxiety-provoking environmental and social factors may be present prior to initiation of methamphetamine use.
Experience of childhood adversity (Read and Bentall, 2012), a “rejecting and overprotective parenting style” (Koszycki et al., 2013, p.278), a history of depression (Duncan et al., 2022) and personality traits that preference internalising symptoms may precipitate the onset of panic attacks (Raskin et al., 1982) and increase the risks of experiencing substance use disorders. High rates of prejudice, social exclusion, discrimination and victimisation mean that identifying as part of a sexual minority (i.e. non-heterosexual or a non-binary gender) may also result in higher rates of suicidal ideation and behaviour (Williams et al., 2021) as well as anxiety, which can manifest as panic attacks (Math & Seshadri, 2013). This is reflected in higher rates of methamphetamine use among people who identify as non-heterosexual and/or gender diverse (Roxburgh et al., 2016). Cohen et al. (2003) found reports of violence to be extensive amongst a cohort of people who were methamphetamine dependent, with 58% of women and 16% of men in the study reporting sexual abuse and violence at some point in their lifetime.
Social support, as measured by subjective perceptions of the quality of one’s interpersonal relationships (Ozbay et al., 2007), is a significant predictor of mental health outcomes (Ozbay et al., 2007). Low social support has been established as an important precipitant to methamphetamine use (Farnia et al., 2018).
In Australia, the legacy of a violent and entrenched colonisation history has resulted in significantly higher rates of psychological distress and suicide amongst First Nations people, relative to the general population (Australian Institute of Health and Welfare, 2015; Parker & Milroy, 2014; Reilly, Wand, McKetin, et al., 2020). Rates of methamphetamine use amongst Indigenous populations is estimated to be more than twice that of the non-Indigenous population (Australian Institute of Health and Wellbeing, 2022) and Reilly and colleagues (2020) found that while substance use patterns were similar to non-Indigenous counterparts, a third of Aboriginal and Torres Strait Islander participants in an Australian methamphetamine study reported rates of distress in the very severe range. They were also more likely to have attended a mental health service and to have received a psychiatric diagnosis.
Methamphetamine Use and Panic Attack
Evidence on the experience of panic attacks among people who use methamphetamine is scant, only alluded to in literature related to anxiety and mental health symptomatology in general. A Canadian study investigating the mediating role of alcohol and other drug use in the context of different types of anxiety disorder found self-medication with both alcohol and other drugs to be most common amongst younger cohorts (18–44 years), those who were not in an intimate relationship, and individuals who had lower income and education (Robinson et al., 2009). Furthermore, “self-medication with both drugs and alcohol was most prevalent among individuals diagnosed with panic disorder with agoraphobia” (p. 42). Therefore, for some individuals, symptoms of anxiety (including panic attack) may pre-date methamphetamine use, and substance use may indeed constitute a strategy to manage unpleasant psychiatric symptoms.
Increasing understanding of panic attacks amongst people who use methamphetamine is important because the intense discomfort of such experiences may induce help-seeking behaviour, although it may also prompt increased substance use, potentially leading to substance related harm. Learning more about panic attacks within this population may help address gaps in care of people who use methamphetamine, particularly considering the high occurrence of comorbid mental health issues and the relative limitations of pharmacotherapies. People who report that they are “bothered” by their panic attacks may be more likely to seek support (Harris et al., 2016); therefore, implications for practice may emerge from increasing understanding of the prevalence and correlates of panic attacks. Extant literature on the prevalence and correlates of panic attacks have largely derived from research with cohorts of young people or populations diagnosed with specific chronic illnesses and predominantly in clinical settings (Moreno-Peral et al., 2014). The methamphetamine literature is largely derived from studies within treatment settings where participants are more likely to inject methamphetamine (McKetin et al., 2019). In Australia, the most common route of administration is smoking (Australian Institute of Health and Welfare, 2020). It is unknown whether the experience of panic attacks for people outside treatment settings who mainly smoke methamphetamine differs from those of people within treatment settings who mainly inject methamphetamine. Research suggests that smoking methamphetamine may intensify and expedite the drug effect (Cook et al., 1993) which could amplify panic symptoms and can contribute to more impulsive and risky behaviours (McKetin et al., 2021). The ramifications of such behaviours may also lead to increased anxiety and panic.
While some studies have examined methamphetamine use and dependence variables in the context of anxiety (e.g. McKetin et al., 2019; Vik, 2007), an integrated exploratory approach to developing understanding of the factors that may contribute to experience of panic attack amongst this cohort has not previously been undertaken. Polcin et al. (2012) observed that “the prevalence of specified subgroups of anxiety disorders have not been well documented, such as panic disorder, agoraphobia and social phobia” (p. 3).
An Australian study identified high rates of generalised anxiety disorder (GAD) amongst a community sample of methamphetamine smokers (BLINDED et al., 2021). Although a meta-analysis found no significant association between methamphetamine use and anxiety, authors identified that the evidence was weak, warranting further research on the issue (McKetin et al., 2019). This study addresses the knowledge gap surrounding the prevalence of panic attack in a cohort who smoke methamphetamine, and to explore the correlating social, economic, mental health and substance use factors. To our knowledge, this is the first study to examine panic attack within this population.
Aims of the Study
The aim of this cross-sectional study was to determine the prevalence and key correlates of panic attacks among a community-recruited cohort of Australians who primarily smoke methamphetamine. We expected to find higher rates of panic attack experiences than reported for the general Australian population and variables such as gender, age, Aboriginal and Torres Strait Islander status, homelessness and social support to be associated with panic attack prevalence.
Material and Methods
Cross-sectional analysis was conducted on baseline data collected for VMAX, a prospective cohort study examining the trajectory of people who predominantly smoke methamphetamine from Victoria, Australia. Ethics approval was provided by the Human Research Ethics Committees of both the Burnet Institute (project number: 171/16) and Monash University (project number: 2938). Written informed consent was gained prior to data collection.
Design
The sample and methods have been described in detail previously (Quinn et al., 2021). In brief, eligible participants were aged over 18 years, reported at least monthly methamphetamine use over the past 6 months, primarily used non-injecting means of administration of methamphetamine (e.g. snorting or smoking) and resided in metropolitan Melbourne or one of three rural locations in the state of Victoria, Australia. These locations were chosen as they had recorded high levels of methamphetamine-related harms such as ambulance attendances (Quinn et al., 2021). Respondent-driven sampling was the most common recruitment method (53%). Other recruitment approaches included social media, hard copy advertising (posters and flyers) and health service referrals. Data were collected through face-to-face interviews using a structured questionnaire that included tailored questions and validated measures. Questions were organised into the following sections—demographics, drug use history and recent drug use, social support, mental health and general health, methamphetamine treatment utilisation and barriers and criminal behaviour and victimisation. Data were entered directly into a mobile device using REDCap software (Harris et al., 2009).
Measures
Dependent Variable: Anxiety Attack
The outcome variable was derived from the self-reported anxiety component of the Patient Health Questionnaire (PHQ) (Spitzer et al., 1999), namely the response to the first question, “In the last four weeks, have you had an anxiety attack—suddenly feeling fear or panic?”. Responses to four further questions providing details around the panic attack experience were also gathered.
Independent Variables
The choice of independent variables was based on existing literature (Darke et al., 2008; Duncan et al., 2022; McKetin et al., 2019). Variables were grouped into the following domains: demographics, social circumstances, substance use and mental health.
The demographic variables were gender (male, female), age group (18–29 years, 30–39 years and 40 + years), Aboriginal and/or Torres Strait Islander status (yes or no), sexual orientation (heterosexual, yes or no) and rurality (metropolitan or non-metropolitan). Rurality was classified by categorising participants’ residential postcodes according to the Modified Monash Model (MMM), a tool to categorise geographic locations by rurality in Australia (Australian Government Department of Health, 2019).
Social circumstances variables included homelessness in the last 12 months (yes or no), experience of interpersonal assault in the past 6 months (yes or no), currently employed (yes or no) and social support (low or moderate to high). The ENRICHED Social Support Instrument (ESSI 19-plus) was employed to measure social support (Gottlieb & Bergen, 2010).
Methamphetamine use was assessed by type (powder or base, or crystal), route of administration (RoA) (smoked; snorted, swallowed or shafted; or injected) and dependence. Dependence was measured using the Severity of Dependence Scale (SDS)—a 5-item tool which has been found to be suitable for use in a number of different settings (Gossop et al., 1995). Participants were categorised as dependent if they scored 4 or more.
Mental health variables considered were the 7-item General Anxiety Disorder (GAD-7) Measure (Rutter & Brown, 2017) and the 9-item Patient Health Questionnaire (PHQ-9) (Beard et al., 2016) which screens for major depressive disorders. Both scales were categorised nil to mild (scores of < 10) or moderate to severe (scores of 10 and above). We also considered including measures of alcohol and cannabis use. However, the vast majority of participants use alcohol (96%) and cannabis (97%) in addition to methamphetamine, and so these measures were not included in the analysis.
Statistical Analysis
Descriptive statistical analysis was used to measure the prevalence of recent panic attacks across the independent-variable characteristics described above. For those who reported a recent panic attack, we also calculated the proportion who had experienced previous attacks; whether the attacks were unexpected; whether the respondent was bothered by the attacks or worried about having another; and whether typical symptoms were associated with the last bad attack.
Bivariable logistic regression was used to examine associations between the outcome and each independent variable. This was followed by sequential logistic regression for variables grouped according to demographic factors (model A), plus social circumstances (model B), plus methamphetamine use (model C). Odds ratios (ORs), adjusted odds ratios (aORs), 95% confidence intervals (CIs) and p-values are reported. The significance level was p < 0.05.
A complete case approach was used, whereby cases with missing data were excluded from the analysis. Analyses were conducted using SPSS software (version 27.0.0; IBM Corporation, 2020).
Results
Sample Characteristics
For the baseline survey, 744 participants were recruited between June 2016 and June 2018. Thirty-three of these respondents were excluded due to missing data, leaving 711 for analysis. Overall, 36% of participants self-reported a panic attack during the 4 weeks prior to the interview. Of these, 94% had experienced an attack before, 76% reported that attacks were unexpected at the time and 66% that they were bothered a lot or worried by these attacks. Ninety-five per cent responded that during their last bad attack, they had specific panic-related symptoms (Table 1).
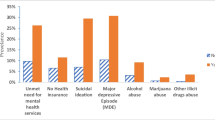
Table 2 sets out the distribution of respondent characteristics. Female participants made up 39% of the sample. Thirty-nine per cent were aged 18–29 years, 35% 30–39 years and 26% 40–67 years. Thirteen per cent identified as being of Aboriginal and/or Torres Strait Islander background. The majority identified as heterosexual (86%) and 65% lived in a non-metropolitan setting. A significant proportion had experienced recent homelessness (37%) and almost a third (30%) had experienced assault in the past 6 months. Just 22% were employed and social support was rated as low for 32% of the cohort (Table 2).
The majority (65%) of participants were methamphetamine dependent. Over 90% of respondents used crystal methamphetamine as their main type of methamphetamine and 80% reported smoking as their main RoA. Forty-five per cent of respondents had moderate to severe anxiety, and 50% had moderate to severe depression (Table 2).
Independent Correlates for Anxiety Attacks
Bivariable analysis showed that the following characteristics were associated with an increased likelihood of panic attacks: being female [aOR 2.15, 95% CI 1.57, 2.94, p < 0.001], younger (aged 18–29 years) [aOR 1.82, 95% CI 1.23, 2.69, p < 0.001], non-heterosexual [aOR 2.36, 95% CI 1.53, 3.64, p < 0.001], not employed [stats] and with low social supports [aOR 1.60, 95% CI 1.16, 2.22, p < 0.004] (Table 2). Having experienced homelessness in the past 12 months [aOR 1.58, 95% CI 1.15, 2.16, p < 0.005] or interpersonal assault in the past 6 months [aOR 2.20, 95% CI 1.59, 3.07, p < 0.001] was also significantly associated with increased likelihood of experiencing an anxiety attack, as was being categorised as methamphetamine dependent [aOR 1.81, 95% CI 1.29, 2.53, p < 0.001] (Table 2).
In bivariable analysis, the outcome variable was strongly correlated with moderate to severe anxiety [aOR 5.49, 57% CI 3.93, 7.69, p < 0.001] and moderate to severe depression [aOR 3.98, 51.3% CI 2.86, 5.53, p < 0.001] (Table 2). The anxiety and depression variables were omitted from multivariable analyses due high correlation with the dependent variable and with each other.
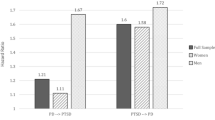
Table 3 sets out the results of the three multivariable models. In model A (demographics), being female [aOR 1.85, 95% CI 1.32, 2.60, p < 0.001], younger [aOR 1.82, 95% CI 1.16, 2.85, p 0.007] and non-heterosexual [aOR 2.19, 95% CI 1.37, 3.49, p < 0.001] were associated with significantly higher odds of reporting experiencing a panic attack. This pattern was largely unchanged by the inclusion of the social-circumstance variables in model B, but experiencing assault was also associated with increased odds of experiencing a panic attack [aOR 1.71, 95% CI 1.19, 2.45]. Inclusion of the substance use variables in model C showed a similar pattern but the association with age was no longer significant, while being methamphetamine dependent was associated with significantly higher odds of reporting a panic attack [aOR 1.78, 95% CI 1.22, 2.59, p < 0.001].
Discussion
We explored the prevalence, characteristics and correlates of panic attack amongst people who primarily smoked methamphetamine. Findings provide new insight into the variables associated with experience of panic attack, for a cohort recruited from community settings.
More than one-third of participants reported a panic attack in the previous 4 weeks. The Australian population estimates are 3.7% in a 12-month period. While there are differences in definitions (panic attack vs disorder) and measurement timeframe, it is likely that the prevalence of panic attack in this study population is significantly higher than that seen in the general population. Further research would be required to identify whether panic attacks experienced by people who smoke methamphetamine are isolated incidents or indicative of panic disorder. We found gender, violence, sexual orientation and methamphetamine dependence to be pertinent factors related to the experience of panic attacks. Our findings are consistent with studies of people who inject drugs which show females are more likely to report recent experiences of assault, and to experience higher levels of distress as a result of assaults than male participants (Scott et al., 2016). King and colleagues concluded that “… being female, being stressed at home, and having little support from family may be causal antecedents to panic attacks” (1993, p.181). The high levels of interpersonal violence as victims found within this cohort are also consistent with previous research (Sommers & Baskin, 2006).
Women and gay men are populations at significantly increased risk of experiencing intimate partner violence (IPV) compared to heterosexual men (Callan et al., 2021), and the profound mental health implications of IPV are well documented. Further investigation is required to understand the relationship between experience of discrimination and its violent manifestations (particularly in relation to sexism, racism and homophobia), panic attacks and the ways in which methamphetamine is used by those who have such life experiences.
Although our study did not find a statistically significant association between social support and panic attack, the finding on recent experience of assault may indicate compromised safety; further qualitative investigation would be required to confirm this interpretation. Leach et al. (2022) found, amongst a cohort of people who use methamphetamine, higher levels of social support were associated with female gender and employment, while homelessness was associated with low social support. Altamura et al. (2005) found evidence that those who have experienced a duration of panic disorder longer than 12 months have increased risk of concurrent depression, and within the current study, a high correlation of both depression and anxiety with the recent experience of panic attack was found.
The high correlation of anxiety and depression amongst those participants who experienced a recent panic attack may not be surprising (Duncan et al., 2022) but illuminates the compounding psychiatric stressors that impact this cohort. The combination of depression, anxiety and methamphetamine use and the significant compromised physical and mental health outcomes that result underscore the necessity of proactive, sensitive and responsive care. Practitioners need to be aware of the high risk of panic attack amongst people who experience depression and use methamphetamine as the discomfort and fear associated with panic attacks may contribute to increased depressive symptoms.
Stigma, shame, discrimination and socioeconomic circumstances (such as a lack of transport) create barriers to health service access (Cumming et al., 2016). This suggests that those who experience panic attacks and use methamphetamine may have longer durations of untreated panic symptoms due to facing multiple healthcare access issues. While this may have significant negative impacts on physical and mental well-being and quality of life, there is some evidence that pharmacotherapy for mental health treatment can still be effective after periods of untreated illness (Altamura et al., 2005). Therefore, it is important that help seeking for this cohort be promoted.
Our findings have implications for the provision of psychosocial support and mental health assessment and treatment. The high number of study participants who had experienced assault in the past 12 months and panic attack is congruent with Remes et al. (2016) findings that trauma and vulnerability to discrimination and stigma exacerbate anxiety. This underscores the importance of trauma-informed approaches to service delivery. Trauma informed care (TIC) includes sensitive use of language that reinforces a person-centred approach and provides hope for recovery (Volkow et al., 2021). For people who use methamphetamine and experience panic attacks, TIC may include sensory modulation such as providing relatively quiet and unstimulating spaces that foster a sense of safety, validation of experiences, and providing choice where possible. EDs and mental health crisis services are both important sites for implementing TIC and EDs could be an entry point to a range of treatment and support services. Presentations to EDs provide an opportunity for psycho-education, harm reduction, referral to drug and alcohol and psychiatric treatment services and early intervention. Healthcare professionals and drug treatment specialists need to be alert to the high likelihood of panic attacks for young women who use methamphetamine and they need to ensure their services are accessible and inclusive for people with diverse sexual and gender identities. When people present with symptoms of panic attack, non-judgemental substance use assessment processes may enhance engagement and promote help seeking for the substance use and also for psychosocial issues such as homelessness. Sensitive questioning about personal safety and experience of assault may also lead to opportunities for counselling and/or other forms of mental health support.
Integrated models of care whereby methamphetamine use and mental health challenges can be addressed simultaneously in ways that matches the individual’s priorities and preferences have been advocated by Duncan and colleagues (2022). Previous studies have demonstrated that integrated care enables health practitioners to more effectively recognise and address individuals’ social needs and disadvantage (Yu et al., 2018), around their identified priorities (Duncan et al., 2022). Some of the barriers to effective treatment such as lack of engagement and low adherence to medications may be addressed through assessment of the individual’s social needs and resources, and working from a person-centred framework to prioritise needs and goals. This may enhance connectedness which is also beneficial for mental health and wellbeing.
Research Considerations
Strengths of this study include the size and diversity of the community sample and the inclusion of rural participants, a cohort that is under-represented in both mental health and substance use research (BLINDED et al., 2021). The recruitment methods also enabled inclusion of participants who are not necessarily seeking treatment or support, whose experiences are rarely captured. A complete case approach to analysis aided statistical precision and meant that the risk of bias was reduced. Limitations of the study include potential sample bias. Due to the recruitment methods, those who were connected to a service or a community were more likely to come across the study information. The validity of the data may also be affected by participant recall and social desirability bias given that they were gathered via face-to-face interviews, and biochemical confirmation of reported use was not undertaken. It is extremely difficult to obtain biochemical confirmation of self-report. However, self-report is commonly used in similar studies and has been shown to be reliable and valid (Darke, 1998). In this study, we measured panic attack experienced in the last 4 weeks while national prevalence statistics for panic measure panic disorder in a 12-month period. This makes comparisons between the cohort of our study and the general population unreliable. Further studies with people who smoke methamphetamine and have a diagnosed panic disorder would clarify this picture.
As the data were cross-sectional, causality cannot be determined. The high prevalence of panic attacks we found among people who use methamphetamine could be explained by one of three mechanisms: methamphetamine use leading to panic attacks; panic symptoms leading to self-medication with methamphetamine; or shared vulnerability factors for both (e.g. trauma or homelessness). Future studies may explore whether a reduction in methamphetamine use reduces panic symptoms irrespective of any other interventions. Other Australian cohort data (McKetin et al., 2013) suggests this may be the case for psychosis. Longitudinal studies that can elucidate the causal pathways between methamphetamine use and panic while accounting for moderators such as gender and sexual orientation and other exposures such as violence victimisation are needed to build on this evidence. Gathering data around the phase of methamphetamine use (e.g. intoxication, withdrawal, abstinence) that is associated with the experience of panic attacks may also provide important information for treatment and support.
While this study has illuminated some factors associated with experience of panic attacks amongst people who use methamphetamine, in-depth qualitative exploration of the experience of panic attacks amongst people who use methamphetamine is warranted. This might include gathering data on the experience of poly substance use, particularly alcohol and cannabis, the relationship of psychosis and panic attacks and the stage of substance use (e.g. intoxication, withdrawal) when panic attacks are experienced, along with investigating mental health needs and help-seeking behaviours, which may assist in pinpointing intervention opportunities.
Panic attacks are unpleasant, frightening and, if untreated, can lead to other compounding mental health conditions. Services need to develop programs that can provide sensitive and responsive care to women, people who identify as non-heterosexual and/or gender diverse and those who may have experienced recent assault. This study reinforces the need for specialised mental health and substance use services to be available and accessible and for non-judgemental, trauma informed engagement with people who use methamphetamine regarding their mental health experiences and needs.
Data Availability
Access to the dataset can be requested by contacting the first author Dr Rochelle Hine, rochelle.hine1@monash.edu.
References
Altamura, A., Santini, A., Salvadori, D., & Mundo, E. (2005). Duration of untreated illness in panic disorder: A poor outcome risk factor? Neuropsychiatric Disease and Treatment, 1(4): 345–347. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2424121/
Australian Bureau of Statistics. (2022). National Survey of Mental Health and Wellbeing: Summary of Results, 2020–21. Australian Bureau of Statistics. https://www.abs.gov.au/statistics/health/mental-health/national-study-mental-health-and-wellbeing/latest-release#data-download. Accessed 19 Dec 2022
Australian Government Department of Health. (2019). Modified Monash Model Fact Sheet. https://www.health.gov.au/sites/default/files/documents/2020/07/modified-monash-model---fact-sheet.pdf.. Accessed 26 Aug 2022
Australian Institute of Health and Welfare. (2015). The health and welfare of Australia’s Aboriginal and Torres Strait Islander peoples: 2015. https://www.aihw.gov.au/reports/indigenous-health-welfare/indigenous-health-welfare-2015/contents/determinants-of-health-key-points
Australian Institute of Health and Welfare. (2020). Alcohol, tobacco and other drugs in Australia. https://www.aihw.gov.au/reports/alcohol/alcohol-tobacco-other-drugs-australia/contents/drug-types/meth/amphetamine-and-other-stimulants. Accessed 26 Aug 2022
Australian Institute of Health and Wellbeing. (2022). Alcohol, tobacco & other drugs in Australia. https://www.aihw.gov.au/reports/alcohol/alcohol-tobaccoother-drugs-australia/contents/priority-populations/aboriginal-and-orres-strait-islander-people
Beard, C., Hsu, J., Rifkin, L., Busch, A., & Bjőrgvinsson, T. (2016). Validation of the PHQ-9 in a psychiatric sample. Journal of Affective Disorders, 193: 267–273. https://pubmed.ncbi.nlm.nih.gov/26774513/
Brecht, M., O'Brien, A., von Mayrhauser, C. &, Anglin, M. (2004). Methamphetamine use behaviors and gender differences. Addictive Behaviours, 29(1):89–106. https://pubmed.ncbi.nlm.nih.gov/14667423/
Callan, A., Corbally, M., & McElvaney, R. (2021). A scoping review of intimate partner violence as it relates to the experiences of gay and bisexual men. Trauma, Violence, & Abuse, 22(2), 233–248. https://doi.org/10.1177/1524838020970898
Cohen, J., Dickow, A., Horner, K., Zweben, J., Balabis, J., Vandersloot, D. et al. (2003). Abuse and violence history of men and women in treatment for methamphetamine dependence. American Journal on Addictions, 12(5): 377–385. https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.523.8099&rep=rep1&type=pdf
Cook, C. E., Jeffcoat, A. R., Hill, J. M., et al. (1993). Pharmacokinetics of methamphetamine self-administered to human subjects by smoking S-(+)-metham-phetamine hydrochloride. Drug Metabolism and Disposition, 21, 717–723.
Cumming, C., Troeung, L., Young, J., Kelty, E. & Preen, D. (2016). Barriers to accessing methamphetamine treatment: A systematic review and meta-analysis. Drug and Alcohol Dependence. 168: 263–273. https://pubmed.ncbi.nlm.nih.gov/27736680/
Darke, S. (1998). Self-report among injecting drug users: A review. Drug and Alcohol Dependence, 51(3). https://doi.org/10.1016/S0376-8716(98)00028-3.
Darke, S., Kaye, S., McKetin, R. & Duflou, J. (2008). Major physical and psychological harms of methamphetamine use. Drug and Alcohol Review, 27: 253–262. https://pubmed.ncbi.nlm.nih.gov/18368606/
Derrick, K., Green, T., & Wand, T. (2019). Assessing and responding to anxiety and panic in the Emergency Department. Australasian Emergency Care, 22(4), 216–220. https://doi.org/10.1016/j.auec.2019.08.002
Duncan, Z., Kippen, R., Sutton, K., Ward, B., Agius, P. A., Quinn, B., & Dietze, P. (2022). Correlates of anxiety and depression in a community cohort of people who smoke methamphetamine. Australian & New Zealand Journal of Psychiatry 56(8), 964–973. https://doi.org/10.1177/00048674211048152
Eaton, W., Kessler, R., Wittchen. H. & Magee, W. (1994). Panic and panic disorder in the United States. American Journal of Psychiatry, 151: 413–420. https://pubmed.ncbi.nlm.nih.gov/8109651/
Farnia, V., Alikhani, M., Jalali, A., Golshani, S., Salemi, S., Hookari, S., et al. (2018). The role of attachment styles and perceived social support in prediction of methamphetamine abuse. Journal of Substance Use, 23(4), 377–383. https://doi.org/10.1080/14659891.2018.1436598
Gadalla, T. M. (2009). Determinants, correlates and mediators of psychological distress: A longitudinal study. Social Science & Medicine, 68(12), 2199–2205. https://doi.org/10.1016/j.socscimed.2009.03.040
Glasner-Edwards, S., Mooney, L.J., Marinelli-Casey, P., Hillhouse, M., Ang, A., Rawson, R. & Methamphetamine Treatment Project. (2008). Identifying methamphetamine users at risk for major depressive disorder: Findings from the methamphetamine treatment project at three-year follow-up. American Journal of Addiction, 17, 99–102. https://pubmed.ncbi.nlm.nih.gov/18393051/
Glasner-Edwards, S., Mooney, L., Marinelli-Casey, P., Hillhouse, M., Ang, A., Rawson, R., et al. (2010). Anxiety disorders among methamphetamine dependent adults: Association with post-treatment functioning. The American Journal on Addictions, 19: 385–390. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3159418/
Goodwin, R. & Hamilton, S. (2001). Panic attack as a marker of core psychopathological processes. Psychopathology, 34: 278–288. https://pubmed.ncbi.nlm.nih.gov/11847487/
Gossop, M., Darke, S., Griffiths, P., Hando, J., Powis, B., Hall, W. et al. (1995). The Severity of Dependence Scale (SDS): Psychometric properties of the SDS in English and Australian samples of heroin, cocaine and amphetamine users. Addiction, 90: 607–614. https://pubmed.ncbi.nlm.nih.gov/7795497/
Gottlieb, B. & Bergen, A. (2010). Social support concepts and measures. Journal of Psychosomatic Research, 69(5): 511–520. https://pubmed.ncbi.nlm.nih.gov/20955871/
Harris, P., Taylor, R., Thielke, R., Payne, J., Gonzalez, N. & Conde, J. (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Information, 42: 377–381. https://pubmed.ncbi.nlm.nih.gov/18929686/
Harris, M., Baxter, A., Reavley, N., Diminic, S., Pirkis, J., & Whiteford, H. (2016). Gender-related patterns and determinants of recent help-seeking for past-year affective, anxiety and substance use disorders: Findings from a national epidemiological survey. Epidemiology and Psychiatric Sciences, 25(6): 548–561. https://pubmed.ncbi.nlm.nih.gov/26428069/
Harvard Medical School. (2007). Data Table 1: Lifetime prevalence DSM-IV/WMH-CIDI disorders by sex and cohort. National Comorbidity Survey (NCS). https://www.hcp.med.harvard.edu/ncs/index.php.
Hurst, T. (2019). World drug report. The Encyclopedia of Women and Crime, 1–2. https://doi.org/10.1002/9781118929803.ewac0543
IBM Corporation. (2020). IBM SPSS Statistics for Windows, Version 27.0 [Computer software]. IBM Corporation
Kay-Lambkin, F., Baker, A., & Lewin, T. (2004). The ‘co-morbidity roundabout’: A framework to guide assessment and intervention strategies and engineer change among people with co-morbid problems. Drug and Alcohol Review, 23(4), 407–423. https://doi.org/10.1080/09595230412331324536
Kay-Lambkin, F. J., Baker, A. L., Lee, N. M., Jenner, L., & Lewin, T. J. (2011). The influence of depression on treatment for methamphetamine use. Medical Journal of Australia, 195, S38–S43. https://doi.org/10.5694/j.1326-5377.2011.tb03264.x
Koszycki, D., Bilodeau, C., Zwanzger, P., Schneider, B., Flament, M. & Bradwejn, J. (2013). Parental bonds in children at high and low familial risk for panic disorder. Child Psychiatry of Human Development. 44: 278–289. https://pubmed.ncbi.nlm.nih.gov/22837072/
Leach, M. J., Ward, B., Kippen, R., Quinn, B., Agius, P. A., Sutton, K., & Dietze, P. M. (2022). Level and correlates of social support in a community‐based sample of Australians who primarily smoke methamphetamine. Health & Social Care in the Community, 30(6), e4950–e4960. https://doi.org/10.1111/hsc.13907
Marshall, B.D., Wood, E., Shoveller, J.A., Buxton, J.A., Montaner, J.S., & Kerr, T. (2011). Individual, social, and environmental factors associated with initiating methamphetamine injection: Implications for drug use and HIV prevention strategies. Prevention Science, 12(2), 173–180. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3107866/
Math, S. & Seshadri, S. (2013). The invisible ones: sexual minorities. Indian Journal of Medical Research, 137(1): 4–6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3657897/
McKetin, R., Lubman, D. I., Lee, N. M., Ross, J. E., & Slade, T. N. (2011). Major depression among methamphetamine users entering drug treatment programs. Medical Journal of Australia, 195, S51–S55. https://doi.org/10.5694/j.1326-5377.2011.tb03266.x
McKetin, R., Lubman, D.I., Baker, A.L., Dawe, S., & Ali, R.L. (2013). Dose-related psychotic symptoms in chronic methamphetamine users: Evidence from a prospective longitudinal study. JAMA psychiatry, 70(3), 319–324. https://jamanetwork.com/journals/jamapsychiatry/article-abstract/1555603
McKetin, R., Degenhardt, L., Shanahan, M., Baker, A.L., Lee, N.K., & Lubman, D.I. (2018). Health service utilisation attributable to methamphetamine use in Australia: Patterns, predictors and national impact. Drug and Alcohol Review, 37(2), 196–204. https://pubmed.ncbi.nlm.nih.gov/28294443/
McKetin, R., Leung, J., Stockings, E., Huo, Y., Foulds, J., Lappin, J., et al. (2019). Mental health outcomes associated with of the use of amphetamines: A systematic review and meta-analysis. E-Journal of Clinical Medicine, 17(16): 81–97. https://pubmed.ncbi.nlm.nih.gov/31832623/
McKetin, R., Ross, J., Kelly, E., Baker, A., Lee, N., Lubman, D,I,, Mattick, R. (2021). Characteristics and harms associated with injecting versus smoking methamphetamine among methamphetamine treatment entrants. Drug Alcohol Review, 27(3):277–85. https://pubmed.ncbi.nlm.nih.gov/18368609/
McLean, C., Asnaani, A., Litz, B. & Hofmann, S. (2011). Gender differences in anxiety disorders: Prevalence, course of illness, comorbidity and burden of illness. Journal of Psychiatric Research, 45:1027–1035. https://pubmed.ncbi.nlm.nih.gov/21439576/
Moreno-Peral, P., Conejo-Cerón, S., Motrico, E., Rodríguez-Morejón, A., Fernández, A., García-Campayo, J., et al. (2014). Risk factors for the onset of panic and generalised anxiety disorders in the general adult population: A systematic review of cohort studies. Journal of Affective Disorders, 168: 337–348. https://pubmed.ncbi.nlm.nih.gov/25089514/
Morley, K.C., Cornish, J.L., Faingold, A., Wood, K., & Haber, P.S. (2017). Pharmacotherapeutic agents in the treatment of methamphetamine dependence. Expert opinion on investigational drugs, 26(5), 563–578. https://pubmed.ncbi.nlm.nih.gov/28351169/
Ozbay, F., Johnson, D., Dimoulas, E., Morgan, C., Charney, D., & Southwick, S. (2007). Social support and resilience to stress: From neurobiology to clinical practice. Psychiatry (Edgmont), 4(5): 35–40. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2921311/
Parker, R., & Milroy, H. (2014). Aboriginal and Torres Strait Islander mental health: an overview. Working together: Aboriginal and Torres Strait Islander mental health and wellbeing principles and practice, 2: 25–38. Commonwealth of Australia
Polcin, D., Buscemi, R., Nayak, M., Korcha, R., & Galloway, G. (2012). Gender differences in psychiatric symptoms among methamphetamine dependent residents in sober living houses. Addictive disorders & their treatment, 11(2): 53–63. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3614000/
Quinn, B., Ward, B., Agius, P. A., Jenkinson, R., Hickman, M., Sutton, K., & Dietze, P. M. (2021). A prospective cohort of people who use methamphetamine in Melbourne and non‐metropolitan Victoria, Australia: Baseline characteristics and correlates of methamphetamine dependence. Drug and Alcohol Review, 40(7), 1239–1248. https://doi.org/10.1111/dar.13194
Raskin, M., Peeke, H., Dickman, W. & Pinsker, H. (1982). Panic and generalized anxiety disorders. Archives of General Psychiatry, 39: 687–689. https://psycnet.apa.org/record/1982-28323-001
Read, J., & Bentall, R. (2012). Negative childhood experiences and mental health: Theoretical, clinical and primary prevention implications. British Journal of Psychiatry, 200(2): 89–91. https://pubmed.ncbi.nlm.nih.gov/22297585/
Remes, O., Brayne, C., van der Linde, R., & Lafortune, L. (2016). A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain and behaviour, 6(7): e00497. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4951626/
Robinson, J., Sareen, J., Cox, B. & Bolton, J. (2009). Self-medication of anxiety disorders with alcohol and drugs: Results from a nationally representative sample. Journal of Anxiety Disorders, 23(1): 38–45. https://pubmed.ncbi.nlm.nih.gov/18571370/
Roxburgh, A., Lea, T., de Wit, J., & Degenhardt, L. (2016). Sexual identity and prevalence of alcohol and other drug use among Australians in the general population. International Journal of Drug Policy, 28: 76–82. https://doi.org/10.1016/j.drugpo.2015.11.005
Rutter, L. & Brown, T. (2017). Psychometric properties of the Generalized Anxiety Disorder Scale-7 (GAD-7) in outpatients with anxiety and mood disorders. Journal of Psychopathology and Behavioral Assessment, 39(1): 140–146. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5333929/
Scott, N., Carrotte, E. R., Higgs, P., Cogger, S., Stoové, M. A., Aitken, C. K., & Dietze, P. M. (2016). Longitudinal changes in psychological distress in a cohort of people who inject drugs in Melbourne, Australia. Drug and alcohol dependence 168: 140–146. https://doi.org/10.1016/j.drugalcdep.2016.08.638
Sheikh, J., Leskin, G. & Klein, D. (2002). Gender differences in panic disorder: Findings from the National Comorbidity Survey. The American Journal of Psychiatry, 159: 55–58. https://pubmed.ncbi.nlm.nih.gov/11772690/
Sommers, I., & Baskin, D. (2006). Methamphetamine use and violence. Journal of Drug Issues, 36(1), 77–96. https://psycnet.apa.org/record/2006-04801-004
Spitzer, R., Kroenke, K., Williams, J. & the Patient Health Questionnaire Primary Care Study Group (1999). Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. JAMA, 282(18): 1737–1744. https://pubmed.ncbi.nlm.nih.gov/10568646/
Vik, P. (2007). Methamphetamine use by incarcerated women: Comorbid mood and anxiety problems. Womens Health Issues, 17(4): 256–63. https://pubmed.ncbi.nlm.nih.gov/17544297/
Volkow, N., Gordon, J. & Koob, G. (2021). Choosing appropriate language to reduce the stigma around mental illness and substance use disorders. Neuropsychopharmacol, 46: 2230–2232. https://pubmed.ncbi.nlm.nih.gov/34276051/
Williams, A., Jones, C., Arcelus, J., Townsend, E., Lazaridou, A., & Michail, M. (2021). A systematic review and meta-analysis of victimisation and mental health prevalence among LGBTQ+ young people with experiences of self-harm and suicide. PloS One, 16(1), e0245268. https://doi.org/10.1371/journal.pone.0245268
Yu, S., van Gool, K., Edwards, K., Kirkby, S., Gardner, K., Robinson, L. et al. (2018). The business of integrated care: Implementing new models of care in a fee-for-service setting. Journal of Integrated Care, 26: 16–28. http://hdl.handle.net/10453/130457
Zweben, J., Cohen, J., Christian, D., Galloway, G., Salinardi, M., Parent, D., et al. (2004). Psychiatric symptoms in methamphetamine users. The American Journal on Addictions, 13, 181–190. https://doi.org/10.1080/10550490490436055
Acknowledgements
The authors thank the participants of this study and also acknowledge the contributions of Rebecca Jenkinson, Paul Agius and Matthew Hickman as Chief Investigators on the VMAX project team.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions The VMAX study was established with a grant from the Colonial Foundation and is now funded by the National Health and Medical Research Council (NHMRC, 1148170). PD is supported by an NHMRC Senior Research Fellowship (1136908). BQ was supported by a Postdoctoral Fulbright Scholarship during the 2016/17 financial year. PD has received investigator-driven funding from Gilead Sciences and Indivior for work unrelated to this study.
Author information
Authors and Affiliations
Contributions
Rochelle Hine: study concept and design, data analysis, leading manuscript writing.
Bernadette Ward: study concept and design, data analysis, writing manuscript.
Rebecca Kippen: study concept and design, data analysis, writing manuscript.
Zoe Duncan: data collection, data analysis, writing manuscript.
Keith Sutton: study concept and design, writing manuscript.
Brendan Quinn: study concept and design, obtaining funding, writing manuscript.
Aimee Powell: data collection, writing manuscript.
Paul Dietze: project management, ethics, study concept and design, obtaining funding, writing manuscript.
Corresponding author
Ethics declarations
Ethics Approval and Consent to Participate
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all patients for being included in the study.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hine, R., Ward, B., Kippen, R. et al. Prevalence and Correlates of Panic Attacks Among People Who Primarily Smoke Methamphetamine. Int J Ment Health Addiction (2023). https://doi.org/10.1007/s11469-023-01042-w
Accepted:
Published:
DOI: https://doi.org/10.1007/s11469-023-01042-w