Abstract
This study aimed to evaluate substance use and comorbid mental disorders in delinquent adolescents presenting to a child and adolescent psychiatry outpatient clinic. This study included 47 adolescents aged 15–18 years and had a history of delinquency. Data were collected using the Addiction Profile Index Adolescent Form (API-A) and an information form. Results indicated that the adolescents’ mean age is 16.11 ± 1.05 years, 78.7% had committed crimes against property and 34.0% against the person, and 34.0% were also victims of crime. Mean API-A total scores indicated that their level of substance use was low. In addition, mean API-A total scores showed significant differences according to the adolescents’ migration status, age, economic status, school attendance, mental disorder diagnosis, duration of mental disorder, and type of offense (p < 0.05). The benefit provided by timely and appropriate psychosocial interventions may have a key role in solving this problem for adolescents and improving their future as adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Children are immature beings that are developing physically and mentally, are learning their social roles, and require care from adults (Bülbül & Doǧan, 2016). Although they may be classified in various ways based on their developmental, cognitive, and psychological characteristics, according to the Universal Declaration of the Rights of the Child, every individual is considered a child until the age of 18 years. Experiencing a healthy childhood is important in terms of functioning and adapting to society as an adult. Therefore, variables such as socioeconomic conditions and exposure to traumatic life events may lead children to behave inappropriately for their age and developmental stage and develop certain mental disorders (Baysan Arabacı & Taş, 2017). In fact, the most common reasons for presenting to child and adolescent psychiatry outpatient clinics include complaints such as irritability, hyperactivity, disobedience, low academic performance, unhappiness, pessimism, self-harm, anxiety, stuttering, and attention deficit (Aras et al., 2007; Yöntem-Fidan, 2011). Ersoz Alan (Ersöz-Alan, 2019) retrospectively evaluated outpatient admissions and determined that 75.3% of the 1079 children and adolescents who presented were diagnosed as having at least one mental disorder. In another study in which Çeri et al., (2018) evaluated children and adolescents who presented to a pediatric and adolescent psychiatry outpatient clinic, 47% of the patients in the study were found to have at least two concurrent mental disorders.
Children and adolescents are in the process of exploring their world, and as they continue their biological and mental development, they may show a tendency toward illegal acts such as substance use due to the influence of their social environment. According to the 2020 Turkish Drug Report, 11.7% of people presenting for substance use treatment were in the 15 to 19 age range and 0.4% were under 15 years of age; of those who started treatment, 11.5% were under 15 years of age and 37.4% were 15 to 19 years of age (Türkiye Uyuşturucu ve Uyuşturucu Bağımlılığı İzleme Merkezi (TUBİM, 2013). Most of the children and adolescents who present for treatment are reported to be mixed (multiple) substance users (Yüncü et al., 2006). In a study examining 92 children and adolescents who received inpatient treatment in a regional psychiatric hospital in Turkey between 2014 and 2017, the mean age of adolescents was 15.4 years, the age at first substance use was 13.1 years, and 81.3% of the adolescents used multiple substances (Bilaç et al., 2019). In a national study conducted in US population, prevalence of crime was found 18.4% in young population and crime rates were higher in adolescent with a diagnosis of mental illness of conduct disorders, alcohol use disorders, and drug use disorders than in those who do not (Coker et al., 2014). The rate of substance use among children and adolescents is known to be considerable and steadily increasing (TUBİM, 2020), resulting in risky behaviors that can lead to accidents, neurological disorders, and even death (Bilaç et al., 2019).
Due to their immaturity, children and adolescents are unable to foresee the consequences of their actions and may become involved in crime (KARATAŞ, 2020). When children engage in criminal behavior for any reason, which is referred to as juvenile delinquency (Baysan Arabacı & Taş, 2017; World Youth Report, 2003), they are referred as forensic cases to child and adolescent psychiatry outpatient clinics for expert consultation (Ayaz et al., 2012). Sertdemir et al., (2020) evaluated child and adolescent forensic cases over a 5-year period (n = 523) and determined that their alleged offenses included theft (29.4%), battery (25%), sexual offenses (25%), drug possession (6.7%), threat/intimidation (5.6%), and property damage (4.4%). In addition, it is stated that mental health plays a major role in juvenile delinquency (Basto-Pereira & Maia, 2018) and delinquent children frequently have at least one mental disorder diagnosis (Köse et al., 2011). Kang et al. (2018) found that 17.1% of the juvenile delinquents meet the criteria for mood disorders, anxiety disorders, and psychotic disorders, and 24.9% for alcohol-substance use disorders (Kang et al., 2018). In another study conducted in Turkey, 85% (n = 122) of delinquent children and adolescents retrospectively examined had a chronic mental disorder, the most common of which were conduct disorder, substance abuse disorder, and adjustment disorder (Beşer et al., 2016).
Juvenile delinquency is associated with biological, psychosocial, and environmental factors; established biological risk factors include male sex, diagnosis of attention deficit hyperactivity disorder (ADHD), thrill-seeking and risky behaviors, and alcohol and substance use (Havaçeliği Atlam & Şaşman Kaylı, 2019). Substance use can lead to crime by increasing the intensity of emotions, causing hormonal and physiological changes in the body, promoting irrational behavior, and impairing self-regulatory mechanisms (Altuner et al., 2009; Farrington et al., 2001). Moreover, adolescents may resort to theft, robbery, prostitution, or assault/battery to obtain money with which to buy a substance, or commit violent crimes associated with producing, trafficking, and selling the substance (Bennett et al., 2008). Especially drugs, alcohol and marihuana use had a major effect on delinquent behaviors like robbery, fraud, and larceny (Leal & Mier, 2017). It is also stated that substance use is widespread in crime-related environments and therefore, crime causes substance abuse. Especially after initial delinquency, becoming acquainted with criminal subcultures and being in these environments are considered risk factors for alcohol/substance use, while on the other hand, antisocial behaviors in children and adolescents due to genetic or psychosocial factors may result in more substance use and crime (Altuner et al., 2009). Regardless of these two different views, it is important to address these two behavioral disorders together instead of focusing on the causal relationship between substance use and crime. Therefore, detailed mental health examinations of children and adolescents to identify possible substance use and comorbid mental disorders are important for effective treatment and care. Identifying mental problems in children and adolescents, determining their variability and prevalence according to sociodemographic characteristics, and developing preventive measures and characterizing care needs will provide a basis for effective interventions. From this point of view, the present study was conducted to evaluate the presence of substance use and comorbid mental diagnoses in adolescents with a history of delinquency who presented to a child and adolescent psychiatry outpatient clinic.
Methods
This was a descriptive, cross-sectional study carried out with delinquent adolescents who presented to the outpatient clinic of a regional mental health and psychiatric hospital between September 2018 and February 2020.
Participants
The study included adolescents between the ages of 15 and 18 years who had a history of delinquency, presented to the child and adolescent psychiatry outpatient clinic, and were followed up on an outpatient basis. This age group was selected because the Addiction Profile Index Adolescent Form (API-A) was among the data collection tools used in the study and this tool is applicable in adolescents aged 15 to 18 years. No sampling was performed; all adolescents meeting the inclusion criteria were included in the data collection. Data were collected from 52 adolescents, but 5 were excluded due to missing data. Therefore, 47 adolescents were included in the statistical analyses.
Data Collection Tools
Data were collected using the API-A and a participant information form created by the researchers based on a review of the literature. Data are obtained from adolescents who participate in the study, using self-report forms of scales.
Participant Information Form
Created by the researchers after evaluating the relevant literature (Bilginer et al., 2012; Brown & Shillington, 2017; Güngör, 2013; Marotta & Voisin, 2017), this form consisted of 20 questions about the participant’s sociodemographic characteristics, mental disorder diagnoses, traumatic life events, and history of substance use and delinquency. This form is a self-report form and consists some questions for mental illness diagnoses “If you know your mental illness diagnosis, what is it?”, “How many years have you had a mental illness?”, “Did you ever hospitalized for mental illness?”, “How many times have you been hospitalized for mental illness?”; for traumatic life events “Have you been exposed to a traumatic event in your life/in the last year? Emotional: constant criticism, embarrassment, disregard, humiliation in front of others. Physically: slapping, kicking, dragging, beating etc.”; and for history of substance use and delinquency “Have you ever involved a crime?”, “Have you ever use any kind of substance?”, etc. After the children filled out the questions in this form, they were interviewed by the doctor who also took part in the study.
Addiction Profile Index Adolescent Form (API-A)
The API-A is a tool developed to evaluate the different dimensions of addiction and to measure addition severity in adolescents aged 15 to 18 years. API (Addiction Profile Index) is a self-report questionnaire for adults and consists of 37 questions (Ögel et al., 2012a). API-A is an adolescent form that was developed based on the original API form. Original API form consists of 37 questions, although the Turkish version consists of 25 items (adolescent form). In API-A, 12 items with an item-total correlation low of 0.4 were excluded by the authors who did the Turkish validity and reliability (Ögel, Evren, et al., 2012; Ögel, Karadayı, et al., 2012). API-A form has 5 subscales: substance use characteristics, diagnosis, effect on life, cravings, and motivation. The total score is calculated as substance use characteristics subscale score/2 + diagnostic subscale score/5 + effects on life subscale score/6 + craving subscale score/4 + motivation subscale score/3. The API-A has two forms, a self-report and a practitioner form, both including the same questions. The self-report form was used in this study. The Cronbach’s alpha coefficient of the total scale was 0.87 (Ögel et al., 2012a; Ögel, Karadayı, et al., 2012). In this sample, the Cronbach’s alpha coefficient of the scale was 0.96.
Analysis
The data were analyzed using SPSS 22.0. The data were evaluated using frequency, percentage, mean, and standard deviation. As the data were normally distributed, Pearson correlation analysis, independent samples t test, and analysis of variance (ANOVA) were used. The level of statistical significance was p < 0.05 for all analyses.
Ethical Considerations
Approval to conduct this study was obtained from the ethics committee of a university education and research hospital (decision number 63, dated 21.02.2018). In addition, written permission was obtained from the Provincial Health Directorate and institutional approval was obtained from the regional psychiatric hospital in which the study was conducted. All adolescents who participated in the study and their families provided written and verbal consent.
Results
The mean age of the adolescents participating in the study was 16.11 ± 1.05 years, 66% were male, 34% reported living in urban areas, and 68.1% had no history of internal or external migration at any time in their lives. In addition, 57.4% of the adolescents lived with their nuclear family, 40.4% described their socioeconomic status as middle, and 53.2% had social insurance. It was determined that 40.4% of the adolescents were attending school, and most of the attendees were in high school. The other 59.6% of the adolescents were not attending school and most commonly reported dropping out in middle school. Of the adolescents, 78.7% stated that they did not have a job and 51.1% described their relationship with family as good (Table 1).
There was a highly significant, moderate positive correlation between the adolescents’ age and their mean total API-A scores. There were no differences in mean API-A total scores according to their gender, place of residence, household structure, presence of social insurance, employment status, or perception of their family relationship. Mean API-A total scores were significantly higher among adolescents with a history of external migration compared to those with no migration history, among adolescents who perceived their economic status as low compared to those who described it as high, and among adolescents who did not attend school compared to those who were still attending school (Table 1).
In terms of clinical history, 14.9% of the adolescents reported having a chronic physical disease, 42.5% were diagnosed as having a mental disorder, and 23.4% had multiple mental disorder diagnoses. Thirty-four percent stated that they had no diagnosed mental disorder, but had only presented to the child and adolescent psychiatry outpatient clinic to receive psychosocial support. Of the adolescents with diagnosed mental disorders, the mean disease duration was 1.62 ± 2.10 years and 70.2% had never been hospitalized. Of those who had a history of hospital admission, the mean length of their last hospital stay was 5 ± 9.49 days. Overall, 40.4% of the adolescents reported a history of attempted suicide (Table 2).
There was no significant difference in mean API-A total scores according to the presence of physical illness, number of hospitalizations, or history of suicide attempt, and mean API-A total score was not correlated with length of last hospital stay. Mean API-A total scores differed significantly based on the presence of a mental disorder diagnosis and was weakly positively correlated with the duration of the mental disorder (Table 2).
The adolescents’ history of trauma, crime victimization, and delinquency is shown in Table 3. It was reported that 68.1% of the adolescents experienced a traumatic event in the year before the study was conducted; these traumas were reported as emotional (44.7%), verbal (38.3%), physical (21.3%), and sexual (4.3%) in nature. All of the adolescents had a history of delinquency, with property crimes reported by 78.7% (theft: 74.5%, property damage: 2.1%, both theft and property damage: 2.1%) and crimes toward the person reported by 34.0% (fighting: 19.1%, battery: 12.8%, robbery: 2.1%). In addition, 34% of the adolescents reported being the victim of a crime (assault/battery, robbery: 17.0%, verbal assault/insult/slander: 14.9%, harassment and attempted murder: 4.3%).
The adolescents’ mean API-A total scores did not differ significantly according to the history of traumatic event, delinquency, or crime victimization in the last year. However, there was a significant difference among the subgroups of property crime (Table 3). Due to the small sample number, further analysis could not be performed to determine which group was significantly different.
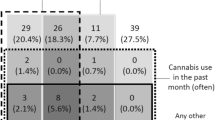
When the mean API-A total and subscale scores of the adolescents were examined, their mean total score (4.98 ± 5.19) indicated a low level of addiction overall. The mean score in the substance use characteristics subscale (1.33 ± 1.59) showed that the frequency of substance use, number of substances used, and problems related to substance use were at low levels. Their mean score in the diagnosis subscale (5.28 ± 6.01) indicated that the adolescents met the diagnostic criteria for addiction. The mean score in the effects on life subscale (6.40 ± 7.25) showed that substance use had some negative effects on the psychosocial functioning and daily lives of the delinquent adolescents. The mean scores for the cravings subscale (0.96 ± 1.25) revealed that the adolescents’ desire to use was low, while their motivation subscale score (1.23 ± 1.45) showed that the adolescents in this study did not experience much difficulty with substance addiction and had high motivation to quit the substance (Table 4).
Discussion
In this study evaluating the substance use and comorbid mental disorder diagnoses of 47 adolescents with a history of juvenile delinquency who presented to the child and adolescent psychiatry outpatient clinic, the mean age was 16.11 ± 1.05 years and approximately two-thirds of the adolescents in the study were male. The majority of the adolescents had no history of internal or external migration, resided in urban areas, lived with their nuclear family, considered themselves to have middle socioeconomic status, and had social insurance. According to the 2019 data from the Turkish Statistical Institute (TurkStat), 236,000 of the 511,247 children admitted to secure wards in our country were victims of crime and 168,000 were juvenile delinquents (TUİK, 2020). Analysis of changes between the years 2015 and 2019 revealed substantial increases in the numbers of children with both criminal victimization and criminal offenses (TUİK, 2020). In 2019, 65.4% of the children were male and 34.6% were female. It has been reported in the literature that juvenile delinquency is more common among boys (Bilaç et al., 2019; Bilginer et al., 2012, 2020; Karataş, 2020; Yüksel, 2019).
In this study, we determined that the adolescents’ age was positively correlated with substance use, and that substance use was more frequent in adolescents who were external migrants compared to non-immigrant adolescents, in those with low perceived economic status compared to those with high economic status, and in those who were not attending school compared to those who attended school. The mean age at time of offense has been reported as 14 to 15 years, with most adolescents’ first offense occurring before the age of 17 (Bilginer et al., 2012, 2020; Güngör, 2013). It has also been stated that psychosocial factors such as adjustment problems, unemployment, and poverty encountered by adolescents and their family due to external migration can also contribute to the risk of juvenile delinquency (Güngör, 2013). The fact that most adolescents in the present study lived in urban areas and many did not work or attend school suggests that they may have experiences associated with risk of criminal involvement, such as spending idle time on the street and forming/joining gangs. Peer delinquency, poor family relationships, sensation-seeking, and gun carrying are other risk factors (Pardini et al., 2021; Parks et al., 2020). This result may also be supported by urban factors such as higher rates of juvenile delinquency, absence of the village social structure, easy access to substances, a more stressful lifestyle, and lack of intense social control in cities (Bilginer et al., 2012; Karataş, 2020). Adolescents who drop out of school due to substance use, mental disorders, or juvenile delinquency are more likely to exhibit violent behavior, offend more frequently, or become adult offenders (Bilginer et al., 2012). Multiple risk factors are affecting persistent delinquent behavior; the largest effect was during the childhood (Assink et al., 2015). This findings are notable, as it shows that family and teacher support is needed by adolescents both for their educational achievement and to encourage them to remain in the education system. To this end, the Ministries of Justice, Health, and National Education should work in cooperation to protect and improve the physical and mental health of adolescents. In addition, periodic screening and follow-up of at-risk children and adolescents with poor academic performance and a history of migration may be recommended. The findings of the present study are consistent with the literature in terms of the impact of age, migration, and school nonattendance.
Of the adolescents in this study, 14.9% had a chronic physical disease, 42.5% had a single mental disorder, and 23.4% had multiple mental disorders. A third of the adolescents presented to the child and adolescent psychiatry outpatient clinic to receive counseling services. Those with mental diagnoses had a mean disease duration of 1.62 ± 2.10 years and most had never been hospitalized. Among those with a history of hospitalization, the mean length of their most recent hospital stay was 5 ± 9.49 days. In addition, we observed that the mean API-A total scores differed among the mental disorder subgroups, and substance use increased with longer duration of the mental disorder. It is reported that juvenile delinquents frequently have one or more mental disorder diagnoses. Bilginer et al. (Bilginer et al., 2020) found in their retrospective study that 62.3% of juvenile delinquents were diagnosed with a mental disorder, most commonly attention deficit hyperactivity disorder (ADHD), cognitive impairment, or conduct disorder. Yüksel (Yüksel, 2019) also found that diagnoses of substance use disorder, ADHD, and conduct disorder were more frequent in children and adolescents with a history of juvenile delinquency. Poor impulse control in adolescents with ADHD and conduct disorder can be said to contribute to substance use, risky behavior (Erdoğan & Delibaş, 2019), and juvenile delinquency. Analysis of the diagnoses of the adolescents in this study revealed that, unlike in the literature, one-third of them had no mental disorder diagnosis and had only presented in order to receive counseling. Another part of our sample group had multiple mental diagnoses, while the remaining part had a mental disorder diagnosed in childhood. We believe this difference is related to the sample group, as this study was conducted with adolescent outpatients. However, despite detecting a significant difference in terms of substance use among the mental disorder subgroups, further analysis was not possible due to the limited sample size. Therefore, further studies with larger samples are recommended to examine the relationship between mental diagnoses and comorbidities, substance use, and criminal history in child and adolescent offenders.
Suicide is an emerging situation. According to the WHO reports, suicide is the fourth leading cause of death in 15–19 years (WHO, 2021). In the present study, 40.4% of the adolescents reported previously attempting suicide. It is known that having a mental illness, alcohol or substance use, and having been forced into sexual relationship increase the risk for suicide in adolescent (Dávila-Cervantes & Luna-Contreras, 2019). Also in a meta-analysis, exposure to interpersonal violence and substance use is found to be most common risk factors for both sex (Miranda-Mendizabal et al., 2019). It is obvious that juvenile delinquents have risk factors for suicidal thoughts and attempts. In another study from Sweden, showed that bullying victimization was uniquely associated with suicide attempt and childhood psychopathology (O’Reilly et al., 2021). It is important to determine the risks and protective factors and implement effective interventions. Pereira et al. (2018) stated that higher scores of self-esteems, self-efficacy, social skills, and family relationship are important protective factors for preventing suicidal ideations and attempts. Interventions in this group should focus on improving self-esteem and efficacy and organizing effective social and family support.
Most of the adolescents in the present study said they had experienced a traumatic event in the last year, reported in order of descending frequency as emotional, verbal, physical, and sexual traumas. However, mean API-A total scores did not differ significantly based on history of trauma in the last year. Studies in the literature examining the relationship between trauma, juvenile delinquency, and substance use have yielded different results. Traumatic events have been reported as precipitating factors in risky behavior, committing or being a victim of violent crime, and substance use (Baglivio et al., 2015; Brown & Shillington, 2017). Adolescents with negative life experiences may use substances to self-medicate, i.e., as a way to cope with their difficult situation. However, this coping mechanism in response to a traumatic event can lead to legal problems and delinquent behavior (Brown & Shillington, 2017). In a study of 1054 adolescents aged 11 to 17 years conducted in the USA by Brown and Shillington (Brown & Shillington, 2017) as part of the National Survey of Child and Adolescent Well-Being, adolescents’ negative childhood experiences were associated with substance use but not with juvenile delinquency. Baglivio et al. (Baglivio et al., 2015) conducted a multiple regression analysis of 64,000 delinquent children and adolescents aged 7 to 17 years in the state of Florida and reported that those who offended before the age of 17 and had multiple negative life experiences exhibited early-onset or chronic criminal behavior. Adolescents are the adults of the future, and the traumas of adolescents with negative childhood experiences must be addressed and treated early in order to prevent possible mental disorders, especially substance use and criminal behavior. In this context, psychiatric nurses in cooperation with families can be involved in early diagnosis, intervention, and protection interventions for adolescents to be academically successful, have a productive work life, and establish healthy relationships as adults. The social and psychological reasons for juvenile delinquency should be considered, and adolescents living in chaotic environments or areas with high crime rates and substance use should be closely monitored. In a study examining the relationship between delinquency and substance use among low-income African American adolescents in the USA, it was determined that adolescents’ negative peer relationships were strongly associated with delinquency, that peer pressure was an important factor in substance use, and that adequate follow-up and future-oriented guidance from parents reduced substance use and criminal behaviors (Marotta & Voisin, 2017). Although we did not evaluate the peer relationships of the adolescents in this study, this finding shows that peer relationships should not be ignored when planning preventive and therapeutic psychosocial intervention programs for adolescents with a history of substance use and delinquency.
In the present study, property crimes were the most common type of offense, and nearly all of these adolescents had committed theft. Previous studies have also shown that adolescents with substance use were frequently involved in crime (Marotta & Voisin, 2017). According to 2019 TurkStat data, 31.7% of juvenile delinquents were brought to secure wards due to battery and 25.6% due to theft (TUİK, 2020). In the literature, theft is the most common crime among child and adolescent offenders (Bilaç et al., 2014; Eyüboğlu & Eyüboğlu, 2018; Leal & Mier, 2017). In a retrospective study, it was reported that theft was the most common crime among 270 children and adolescents referred for forensic psychological assessment (Bilginer et al., 2012); in another study, the most common type of crime committed by juvenile offenders was sexual assault, followed by property damage (Bilginer et al., 2020). We also observed in this study that 38.3% of the adolescents perceived their economic status as low, and these adolescents had higher mean API-A total score than those who considered themselves to have a high economic status. This suggests that the adolescents may have committed theft due to poverty or to enable them to buy the substance they use. In addition, adolescents may commit offenses such as assault, battery, robbery, and fighting due to the inability to control their anger as a result of the effect of substance use on their judgment and perceptions of reality. On the other hand, 34% of the adolescents participating in this study reported being the victim of crime, most frequently physical, verbal, and sexual offenses. Crime victimization may be an etiology of mental disorders in children and adolescents, as well as lead to delinquency, which in turn can result in crime victimization. In order to interrupt this vicious cycle and take protective measures against neglect and abuse, it is necessary to plan interventions encompassing family and school and raise awareness of this subject among children and adolescents (Karataş, 2020).
In this study, the mean API-A total and subscale scores showed that children and adolescents with a history of delinquency met the diagnostic criteria for addiction, albeit at a low level, and their substance use had an effect on their lives. However, it was an encouraging finding that the adolescents reported a low urge to use and a high motivation to quit using, and that they had not yet developed a complex substance use profile (they did not have a history of multiple or frequent substance use). In another study conducted among inpatients at the Child and Adolescent Substance Addiction Treatment and Training Center in our country, the mean API-A score was higher than that of the adolescents in our study (Yildiz et al., 2020). This difference may be due to the fact that our study included adolescent outpatients rather than inpatients. This result also suggests that these adolescents are still in the early stages of addiction, the problem has not become chronic, and there is hope that the problem can be solved. In addition, we determined that a considerable proportion of the cases included in this study had presented to the outpatient clinic for counseling purposes and had no previous criminal history; it was their first experience with delinquency. On this point, therapeutic interventions for adolescents and psychosocial rehabilitation programs provided by health professionals would be beneficial. In fact, the adolescents’ low desire to use the substance and their high motivation to quit suggest that they will easily adapt to such assistance and move rapidly toward recovery.
Limitations
The COVID-19 pandemic has affected the collection of research data worldwide. Changes in the patterns of presentation to hospital outpatient services have adversely affected the number of patients recruited for studies and markedly limited research data obtained over the last year. Also, the adolescents filled out the forms themselves (self-report), and they stated their diagnosis of mental illness as “diagnosed in childhood.” Another limitation of the study is the lack of evaluation of the peer relationships of the adolescents in the study.
Conclusion
In this study examining substance use and comorbid mental diagnoses in a group of delinquent adolescents, the majority of the participants had a history of migration, lived in urban areas, did not attend school, had experienced a traumatic life event in the last year, and had committed theft. It was determined that the adolescents met the criteria for substance addiction (albeit at low severity), that substance use had a limited effect on their lives, and that they had low desire to use and high motivation to quit the substance. External migration experience, socioeconomic status perception, and school attendance were significant factors influencing substance use. The adolescents’ ages and duration of mental illness were also positively correlated with substance abuse. Furthermore, substance use varied according to the type of property crime and mental disorder diagnosis. In conclusion, we recommend protecting the mental health of at-risk adolescents to prevent substance use and delinquency and organizing programs for adolescents with family and school cooperation to ensure continued school attendance, improve their academic performance, and encourage them to enter an occupation.
Implications for Practice
Community mental health nurses should plan and implement community-based interventions to protect and promote adolescents’ mental health in order to improve their future prospects as adults. Adolescents in chaotic environments where crime and substance use are widespread and those who experience traumatic life events comprise risk groups that should be screened periodically to enable early diagnosis and rehabilitation through appropriate interventions. Community mental health nurses can work in cooperation with school nurses to ensure that students with these risk factors continue to attend school and are followed regularly. Nurses can help adolescents from disadvantaged groups, such as those with low socioeconomic status, migrants and refugees, and those with a mental disorder diagnosis or mental symptoms, to avoid legal problems by advising against delinquency and crime victimization and enabling them to benefit from follow-up programs.
References
Altuner, D., Engin, N., Gürer, C., Akyay, İ, & Akgül, A. (2009). Substance use and crime: The results of a survey research. The Journal of Medical Investigations, 7(2), 87–94.
Aras, Ş, Ünlü, G., & Varol-Taş, F. (2007). Symptoms, diagnoses and diagnostic procedures of patients who presented to the child and adolescent psychiatry outpatient clinic. Journal of Clinical Psychiatry, 10, 28–37.
Assink, M., van der Put, C. E., Hoeve, M., de Vries, S. L. A., Stams, G. J. J. M., & Oort, F. J. (2015). Risk factors for persistent delinquent behavior among juveniles: A meta-analytic review. Clinical Psychology Review, 42, 47–61. https://doi.org/10.1016/j.cpr.2015.08.002
Ayaz, M., Ayaz, A. B., & Soylu, N. (2012). Psychiatric evaluation of child and adolescent forensic cases. Journal of Clinical Psychiatry, 15(1), 33–40.
Baglivio, M. T., Wolff, K. T., Piquero, A. R., & Epps, N. (2015). The relationship between adverse childhood experiences (ACE) and juvenile offending trajectories in a juvenile offender sample. Journal of Criminal Justice, 43(3), 229–241. https://doi.org/10.1016/j.jcrimjus.2015.04.012
Basto-Pereira, M., & Maia, Â. (2018). Persistence in crime in young adults with a history of juvenile delinquency: The role of mental health and psychosocial problems. International Journal of Mental Health and Addiction, 16(2), 496–506. https://doi.org/10.1007/s11469-017-9847-7
Baysan Arabacı, L., & Taş, G. (2017). Dragging factors in juvenile delinquency, mental health problems and nursing care. Journal of Psychiatric Nursing 8(2):110–117. https://doi.org/10.14744/phd.2017.88597
Bennett, T., Holloway, K., & Farrington, D. (2008). The statistical association between drug misuse and crime: A meta-analysis. Aggression and Violent Behavior, 13(2), 107–118. https://doi.org/10.1016/j.avb.2008.02.001
Beşer, N. G., Arabacı, L. B., & Uzunoğlu, G. (2016). Türkiye ’ de bir bölge psikiyatri hastanesinde tedavi olan suça itilmiş çocuk profilleri. Anadolu Psikiyatri Dergisi, 17(4), 317–324.
Bilaç, Ö., Pilan, B. . Şentürk, Orhon, Z., & Bayrak, A. (2014). Suça Sürüklenen çocukların suç ve tanı dağılımlarının inclenmesi: kesitsel bir araştırma. Çocuk ve Gençlik Ruh Sağlığı Dergisi, 21(2), 115–122.
Bilaç, Ö., Kavurma, C., Önder, A., Doğan, Y., Uzunoğlu, G., & Ozan, E. (2019). A clinical and sociodemographic evaluation of youths with substance use disorders in a child and adolescent inpatient unit of mental health hospital. Journal of Clinical Psychiatry, 22, 463–471. https://doi.org/10.5505/kpd.2019.30075
Bilginer, Ç., Tural Hesapçıoğlu, S., & Kandil, S. (2012). Bir Üniversite Hastanesine Adli Psikiyatrik Muayene Amacıyla Gönderilen Çocuk Ve Ergenlerin Değerlendirilmesi. Turkiye Klinikleri Journal of Forensic Medicine and Forensic Sciences, 9(1), 20–27.
Bilginer, Ç., Karadeniz, S., Yilmaz, B. C., & Kandil, S. (2020). Forensic psychiatric evaluation and reports of juvenile pushed to crime: A two-year retrospective chart review. Journal of Clinical Psychiatry, 24(2), 217–227. https://doi.org/10.5505/kpd.2020.02360
Brown, S. M., & Shillington, A. M. (2017). Childhood adversity and the risk of substance use and delinquency: The role of protective adult relationships. Child Abuse and Neglect, 63(June 2018), 211–221. https://doi.org/10.1016/j.chiabu.2016.11.006
Bülbül, S., & Doǧan, S. (2016). Suça sürüklenen çocuklarin durumu ve çözüm önerileri. Cocuk Sagligi Ve Hastaliklari Dergisi, 59(1), 31–36.
Çeri, V., Özer, Ü., Layık, M. E., & İz, F. B. A. (2018). Evaluation of Psychiatric Disorders Among Children and Adolescents Who Applied To An Outpatient Service. Van Medical Journal, 25(4), 520–26. https://doi.org/10.5505/vtd.2018.80557
Coker, K. L., Smith, P. H., Westphal, A., Zonana, H. V., & McKee, S. A. (2014). Crime and psychiatric disorders among youth in the US population: An analysis of the national comorbidity survey–adolescent supplement. Journal of the American Academy of Child & Adolescent Psychiatry, 53(8), 888-898.e2. https://doi.org/10.1016/j.jaac.2014.05.007
Dávila-Cervantes, C. A., & Luna-Contreras, M. (2019). Suicide attempt in teenagers: Associated factors. Revista Chilena de Pediatria, 90(6), 606–616. https://doi.org/10.32641/rchped.v90i6.1012
Erdoğan, E., & Delibaş, D. H. (2019). Comparison of clinical features, comorbidity and functioning in substance dependents with and without adult adhd. Anatolian Journal of Psychiatry, 20(3), 296–304. https://doi.org/10.5455/apd.3881
Ersöz-Alan, B. (2019). Assessment of symptoms, diagnosis and comorbidity of patients referring to a child and adolescent psychiatry outpatient clinic. Turkish Journal of Clinics and Laboratory, 10:484–491. https://doi.org/10.18663/tjcl.511659
Eyüboğlu, M., & Eyüboğlu, D. (2018). Psychiatric disorders, sociodemographic features and risk factors in children driving to committing crime. Journal of Clinical Psychiatry, 21(1), 7–14. https://doi.org/10.5505/kpd.2018.02997
Farrington, D. P., Jollıffe, D., Loeber, R., Stouthamer-Loeber, M., & Kalb, L. M. (2001). The concentration of offenders in families, and family criminality in the prediction of boys ’ delinquency. Journal of Adolescence, 579–596.https://doi.org/10.1006/jado.2001.0424
Güngör, M. (2013). Risk Altındaki Çocukların Aile Yapıları ve Suça Yönelimleri (Mersin İli Örneği). Mersin Üniversitesi Eğitim Fakültesi Dergisi, 9(2), 421–434.
Havaçeliği Atlam, D., & Şaşman Kaylı, D. (2019). Bağımlılıkta Riskli Bir Durum : Suç Davranışı. In Türkiye Klinikleri (1. Baskı). Ankara.
Kang, T., Wood, J. M., Louden, J. E., & Ricks, E. P. (2018). Prevalence of internalizing, externalizing, and psychotic disorders among low-risk juvenile offenders. Psychological Services, 15(1), 78–86. https://doi.org/10.1037/ser0000152
Karataş, S. (2020). Suça Sürüklenen Çocuklar ve Suç Mağduru Çocuklara Yönelik Bir Değerlendirme. Psikiyatride Guncel Yaklasimlar - Current Approaches in Psychiatry, 12(4), 575–586. https://doi.org/10.18863/pgy.711319
Köse, S., Aslan, Z., Başgül, ŞS., Şahin, S., Yılmaz, Ş, Çitak, S., & Tezcan, A. E. (2011). Bir eğitim ve araştırma hastanesi çocuk psikiyatrisi polikliniğine yönlendirilen adli olgular. Anatolian Journal of Psychiatry, 12, 221–225.
Leal, W., & Mier, C. (2017). What’s age got to do with it? Comparing juveniles and adults on drugs and crime. Crime and Delinquency, 63(3), 334–352. https://doi.org/10.1177/0011128715616131
Marotta, P. L., & Voisin, D. R. (2017). Testing three pathways to substance use and delinquency among low-income African American adolescents. Children and Youth Services Review, 75, 7–17. https://doi.org/10.1016/j.childyouth.2017.02.009
Miranda-Mendizabal, A., Castellví, P., Parés-Badell, O., Alayo, I., Almenara, J., Alonso, I.,l., et al. (2019). Gender differences in suicidal behavior in adolescents and young adults: Systematic review and meta-analysis of longitudinal studies. International Journal of Public Health, 64(2), 265–283. https://doi.org/10.1007/s00038-018-1196-1
O’Reilly, L. M., Pettersson, E., Quinn, P. D., Klonsky, E. D., Baldwin, J. R., Lundström, S.,l., et al. (2021). A co-twin control study of the association between bullying victimization and self-harm and suicide attempt in adolescence. The Journal of Adolescent Health : Official Publication of the Society for Adolescent Medicine, 69(2), 272–279. https://doi.org/10.1016/j.jadohealth.2020.11.018
Ögel, K., Karadayı, G., Şenyuva, G., & Hatipoğlu, S. (2012b). Development of the Addiction Profile Index (API-A) adolescent form. Psychiatry and Clinical Psychopharmacology, 22(1), 109.
Ögel, K., Evren, C., Karadağ, F., & Gürol, D. T. (2012a). The development, validity, and reliability of the Addiction Profile Index (API). Turk Psikiyatri Dergisi = Turkish Journal of Psychiatry, 23(4), 263–275. Retrieved from http://www.ncbi.nlm.nih.gov/pubmed/23225127
Pardini, D., Beardslee, J., Docherty, M., Schubert, C., & Mulvey, E. (2021). Risk and protective factors for gun violence in male juvenile offenders. Journal of Clinical Child & Adolescent Psychology, 50(3), 337–352. https://doi.org/10.1080/15374416.2020.1823848
Parks, M. J., Solomon, R. J., Solomon, S., Rowland, B. C., Hemphill, S. A., Patton, G. C., & Toumbourou, J. W. (2020). Delinquency, school context, and risk factors in India, Australia, and the United States: Implications for prevention. Journal of Research on Adolescence, 30(S1), 143–157. https://doi.org/10.1111/jora.12455
Pereira, A. S., Willhelm, A. R., Koller, S. H., & Almeida, R. M. M. D. (2018). Risk and protective factors for suicide attempt in emerging adulthood. Ciencia & saude coletiva, 23, 3767–3777. https://doi.org/10.1590/1413-812320182311.29112016
Sertdemir, M., Kut, B., Demirci, Ş, Akça, Ö. F., Erden, S., Uğuz, F.,l., et al. (2020). Retrospective analysis of sociodemographic and clinical characteristics of forensic cases evaluated in a child and adolescent psychiatry clinic in Konya. Turkish Journal of Child and Adolescent Mental Health, 27(1), 27–32. https://doi.org/10.4274/tjcamh.galenos.2020.54264
TUBİM. (2020). Madde Kullanıcıları Profil Çalışması. Ankara. Retrieved from http://www.narkotik.pol.tr/kurumlar/narkotik.pol.tr/TUBİM/Ulusal Yayınlar/ANALIZRAPORU2020.pdf
TUİK. (2020). Güvenlik Birimine Gelen veya Getirilen Çocuk İstatistikleri 2015–2019. Retrieved January 28, 2020, from https://data.tuik.gov.tr/Bulten/Index?p=Guvenlik-Birimine-Gelen-veya-Getirilen-Cocuk-Istatistikleri-2015-2019-33632
Türkiye Uyuşturucu ve Uyuşturucu Bağımlılığı İzleme Merkezi (TUBİM). (2013). EMCDDA 2013 ULUSAL RAPORU (2012 Verileri) Reitox Ulusal Temas Noktası.
WHO. (2021). Adolescent Mental Health. Retrieved from https://www.who.int/news-room/fact-sheets/detail/adolescent-mental-health
World Youth Report. (2003). Juvenile Delinguency (Vol. 501). https://doi.org/10.1007/978-1-60327-164-6
Yildiz, D., Ciftci, A., & Yalcin, O. (2020). Substance use patterns, psychosocial traumas, psychiatric comorbidities, and gender differences among adolescent inpatients at an addiction treatment center. Dusunen Adam J Psychiatr Neurol Sci, 33(2), 190–202. https://doi.org/10.14744/DAJPNS.2020.00078
Yöntem-Fidan, T. (2011). Bir Çocuk-Ergen Ruh Sağlığı ve Hastalıkları Polikliniğine Başvuran Çocuk ve Ergenlerin Ruhsal Belirtileri ve Risk Faktörlerinin Değerlendirilmesi. Konuralp Tıp Dergisi, 3(1), 1–8. Retrieved from www.konuralptipdergi.duzce.edu.tr
Yüksel, T. (2019). Bir Üniversite Hastanesi Çocuk Psikiyatrisi Polikliniğinde Değerlendirilen Suça Sürüklenen Çocuklar. Dicle Tıp Dergisi, 46, 559–565. https://doi.org/10.5798/dicletip.620603
Yüncü, Z., Aydın, C., Coşkunal, H., Altıntoprak, E., & Bayram, A. T. (2006). Çocuk ve Ergenlere Yönelik Bir Bağımlılık Merkezine İki Yıl Süresince Başvuran Olguların Sosyodemografik Değerlendirmesi. Bağımlılık Dergisi, 7(1), 31–37.
Author information
Authors and Affiliations
Contributions
All authors took part in the article process.
Corresponding author
Ethics declarations
Ethics Approval
We (all authors) confirm that the research presented in the paper has received permission from a stated Research Ethics Committee (REC) including adherence to the legal requirements of the study country.
Informed Consent
Informed consent was obtained from all participants.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Baysan Arabacı, L., Dikeç, G., Taş Soylu, G. et al. Analysis of Substance Use and Mental Disorder Diagnoses in Adolescents with a History of Delinquency: a Cross-sectional Study. Int J Ment Health Addiction 22, 146–161 (2024). https://doi.org/10.1007/s11469-022-00864-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11469-022-00864-4