ABSTRACT
Sexual and gender stigma is a known contributor to population health inequities; however, its impact on healthcare access among sexual and gender minorities (SGM) in Thailand is understudied. Therefore, we sought to examine the level of SGM stigma and its impact on self-reported difficulty accessing primary and mental healthcare services among a nationally recruited sample of lesbian, gay, bisexual, transgender, queer, intersex, and other gender and sexually diverse (LGBTQI+) people in Thailand. A previously validated sexual stigma scale was adapted to ascertain perceived and enacted SGM stigma. Between January and March 2018, 1,350 LGBTQI+ participants completed the online survey, and the median age was 27 (Quartile 1, 3: 23, 33) years. In total, 169 (12.5%) and 269 (19.9%) reported difficulty accessing primary and mental healthcare and 365 (27.0%) reported actively concealing their gender expression to access care. In multivariable logistic regression analyses, experiences of enacted stigma were independently associated with difficulty accessing primary healthcare (adjusted odds ratio [AOR] = 1.35; 95% Confidence Interval [CI]: 1.11 – 1.63) and mental healthcare (AOR = 1.26; 95% CI: 1.07 – 1.48), while experiences of perceived stigma were independently associated with difficulty accessing mental healthcare only (AOR = 1.20; 95% CI: 1.07 – 1.34). Our findings call for multi-level interventions to decrease SGM stigma and improve healthcare access among SGM in Thailand.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
INTRODUCTION
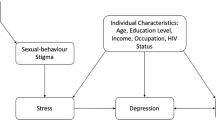
Sexual and gender stigma is a global issue that endangers the health and well-being of sexual and gender minorities (SGM) (Ayhan et al., 2019; DiPlacido & Fallahi, 2020; Hatzenbuehler et al., 2013; Herek, 2007; King et al., 2008; United Nations Development Programme, 2019; United Nations Development Programme & USAID, 2014; White Hughto et al., 2015; Zeeman & Aranda, 2020), including lesbian, gay, bisexual, transgender, queer, intersex, and other gender and sexually diverse (LGBTQI+) communities. SGM stigma refers to the collective negative view, unequal treatment, and devalued status of non-heterosexual identities, beliefs and behaviours (sexual stigma), as well as stigma directed at non-normative gender identities and expressions (gender stigma). SGM stigma is multi-dimensional and includes: perceived stigma, which refers to one’s knowledge of the stigma associated with their identity and the chronic stress that results from expectations of harm; and enacted stigma, which refers to the overt expressions of stigma, such as differential treatment, discrimination, and violence (Herek, 2007, 2016). International research has consistently linked stigma to higher levels of depression, anxiety, and suicide among SGM (Bockting et al., 2013; DiPlacido & Fallahi, 2020; King et al., 2008; Kittiteerasack et al., 2019; Krueger et al., 2020; McNeil et al., 2017; Sutter & Perrin, 2016; White Hughto et al., 2015; Zeeman & Aranda, 2020); underscoring healthcare as a priority for these populations.
However, owing to pervasive stigma in healthcare settings worldwide (Alencar Albuquerque et al., 2016; Ayhan et al., 2019; Ojanen et al., 2016; Snow et al., 2019; Zeeman & Aranda, 2020), SGM’s right to health is often not realized (World Health Organization & United Nations Human Rights Office Of The High Commissioner, 2008). SGM contend with numerous barriers to healthcare that are not experienced by their heterosexual counterparts. In particular, international research has identified: institutional-level barriers (e.g., heteronormative healthcare practices, binary medical wards); provider-level barriers (e.g., discrimination, lack of education and training among providers for culturally competent care, breaches of confidentiality); and patient-level barriers (i.e., disclosure of SGM status). All of these are complicated by broader oppressive and marginalizing forces (e.g., stigma or criminalization in other contexts) (Alencar Albuquerque et al., 2016; Ayhan et al., 2019). As a result of this reality, SGM face social exclusion and precarious encounters in healthcare settings, which can lead to avoidance or fear of healthcare settings and may explain the heavy reliance on pharmacies and self-care practices documented within this population (Alencar Albuquerque et al., 2016; Ayhan et al., 2019).
To begin to address the impact of stigma on SGM, research is required to understand the burden of SGM stigma and its effects on SGM’s access to healthcare. There currently exists a dearth of knowledge in this area among countries in Southeast Asia, where high levels of negative social attitudes towards lesbian and gay people have been documented (Manalastas et al., 2017). In particular, Thailand is known to be a country tolerant of SGM, where SGM are not criminalized, but continue to face wide-spread stigma in society, including in healthcare, education, employment and public settings (e.g., media) (Fongkaew et al., 2019; Newman et al., 2021; Ojanen et al., 2016; Suriyasarn, 2014; United Nations Development Programme, 2019, 2020; United Nations Development Programme & USAID, 2014). In addition, the laws in Thailand do not currently allow for same-sex unions and do not recognize change of legal gender (Ojanen et al., 2016; United Nations Development Programme & USAID, 2014). Research is needed to understand the impact of SGM stigma on healthcare access in Thailand.
According to the minority stress framework (Brooks, 1981; Meyer, 2003), health disparities arise from being a stigmatized minority and experiencing minority-specific stressors (i.e., stigma in society and healthcare) that have deleterious effects on health. A previous study among community-recruited Thai-LGBT (n=411) found that 40.3% met the criteria for clinical depression and that minority-specific stressors (such as experiences of enacted stigma and identity concealment) were correlates of depression (Kittiteerasack et al., 2020). A review study also demonstrated links between minority-specific stressors and major health problems among Thai SGM, including stress, depression, substance use, suicidality, and communicable disease (Ojanen et al., 2016). These findings highlight the need for public health efforts to prioritize SGM’s accessibility to healthcare services to realize SGM’s right to health.
In 2017, the World Health Organization (WHO) reported 14.36 mental health workers per 100,000 population in Thailand, including 0.99 psychiatrists and 0.75 psychologists per 100,000 population (World Health Organization, 2017). In 2018, the healthcare worker (doctors/nurses/midwives) density was an estimated 382 per 100, 000 population (World Health Organization, 2018). All citizens in Thailand receive healthcare coverage under three health insurance schemes, including the Universal Coverage Scheme (UCS), Civil Servant Medical Benefit Scheme (CSMBS), and Social Security Scheme (SSS). An estimated 75% of the population receives care under UCS and among the healthcare schemes, UCS is less flexible than CSMBS as UCS beneficiaries are restricted to access care at designated healthcare facilities, whereby unauthorized access to a facility outside of the designated facility requires the citizen to pay 100% of the out-of-pocket cost for care (Limwattananon et al., 2007; Paek et al., 2016), unless the individual first initiates a facility transfer. CSMBS beneficiaries (government employees, retirees, and their families) are free to access any healthcare facility in the country without costs, while SSS beneficiaries (formal employment coverage) must first register for and use services through a contractor network (Paek et al., 2016). Facility transfers under SSS can only occur once per year during the first three months of the year. Considering the potential effects of these different health insurance schemes when assessing healthcare access in Thailand is important.
In addition, other general constraints to the public healthcare system are important to consider, including cost-related barriers (e.g., some pharmaceutical drugs, transportation, and specialized care), provider-level (e.g., long wait times, lack of capacity) and structural-level barriers (e.g., geographic and transportation barriers) (Chongthawonsatid, 2021). In particular, healthcare resources are concentrated within urban centres and access to care is marked by inequitable differences across rural-urban divides and between regions of Thailand, especially for mental healthcare (Chongthawonsatid, 2021). Mental healthcare has been said to fall short in Thailand for several reasons, including the limited availability of therapeutic counselling, a small number of public practicing psychiatrists and psychologists, and deficits in provider training on cultural competency and the healthcare needs of SGM (Ojanen et al., 2016). In addition, in 2018, a national survey on burnout among 882 Thai psychiatrists and psychiatric residents found that about half the sample reported high-level emotional exhaustion (emotionally overextended or exhausted by work) and about a quarter experienced depersonalization (unsympathetic and impersonal responses to patients) (Nimmawitt et al., 2020).
In 2018, the United Nations Development Programme (UNDP) conducted one of the largest national online surveys to date among LGBTQI+ people in Thailand (United Nations Development Programme, 2019). Utilizing this survey data, our study objectives were to estimate the prevalence of multiple dimensions of SGM stigma (i.e., perceived and enacted stigma) and self-reported difficulty accessing primary and mental healthcare services and assess the relationships between them. We hypothesize that both experiences of perceived and enacted stigma will be associated with higher levels of difficulty accessing both primary and mental healthcare services.
METHODS
Study design and recruitment of participants
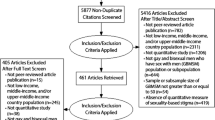
The UNDP’s national online survey was administered between January and March 2018. Several local, regional, and national LGBT community organizations from four regions of Thailand, including North (Chiang Mai and Phitsanulok), Northeast (Ubon Ratchathani), Central (Bangkok), and South (Pattani) provinces, collaborated to recruit study participants through a chain-referral sampling method (United Nations Development Programme, 2019). Over 24 LGBT-related community organizations were sent survey promotional images to share online and within their social media networks. These organizations acted as initial seeds to recruit the participants. To be eligible to participate in the anonymous survey, individuals must have provided informed consent. The online survey started with a consent form that included: the purpose of the study, study procedures, anonymity, voluntary participation, risks, potential benefits, incentives, investigator contact information and rights of the research participant. After reviewing the consent form, participants must have responded “Yes” to the question “Do you agree to participate in this study?” to be included, as well as acknowledge that they have read and understood the consent form, are at least 18 years old, currently reside in Thailand, self-identify as a SGM and have the ability to read and speak the Thai language (United Nations Development Programme, 2019). Detailed descriptions of the survey have been published online by UNDP (United Nations Development Programme, 2019). Participants could enter a lucky draw upon completion of the survey to win a redeemable gift card. In total, 10 survey respondents were randomly selected to win a gift card prize in the amount of ฿1,000 to ฿5,000 (Thai Baht; US$30 to $150).
We used Cochran’s formula to estimate the sample size needed to assess the proportions of our outcome variables at 50% prevalence at the 95% Confidence level with a 5% margin of error (Cochran, 1953). The adequate sample size needed was found to be n=377, which we surpassed by having n=1350 participants who provided consent and completed the survey. All LGBTQI+ participants who completed the online, structured questionnaire with close-ended questions were included in the present analysis. The survey was approved by the Asian Institute of Technology Research Ethics Review Committee.
Study measures
We used two binary outcome variables for the present analyses: difficulty accessing primary healthcare (difficult vs. moderate/easy) and mental healthcare (difficult vs. moderate/easy). Participants were asked one question: “How easy is it for you to obtain the following medical and health services if you need it? 1) primary health services 2) mental health services”. Responses included a scale ranging from 0 to 7 (0 = ‘don’t need it’, 1 = ‘very easy’ and 7 = ‘very difficult’). After inspecting the frequency of responses in both outcome variables, all participants provided a response between 1 to 7. We categorized scores 1 to 4 as ‘moderate/easy’ and 5 to 7 as ‘difficult’
The main explanatory variables of interest included two interval measures of SGM stigma: perceived and enacted stigma. A previously validated 12-item sexual stigma scale was adapted and used (Logie & Earnshaw, 2015), which included a 5-item measure in the perceived stigma sub-scale and a 7-item measure in the enacted stigma sub-scale. Items were scored on a Likert-scale ranging from 1 (‘never’) to 7 (‘always’). The sexual stigma scale was adapted to include gender stigma through collaborations between UNDP and LGBT civil society organizations (United Nations Development Programme, 2019). The questions are shown in Table 1. The term “LGBT” was translated as “people of diverse gender” in Thai. In Thai language, biological sex, gender, and sexuality are widely conflated; thus, the term “people of diverse gender” in Thai can refer to all SGM. This differs from the Western context, where distinctions are made between biological sex, gender, and sexuality (United Nations Development Programme, 2019). The perceived and enacted stigma sub-scales showed acceptable internal consistency (Cronbach’s α = .70 and α = .73, respectively).
We assessed gender identity utilizing the “two-step” approach recommended as best practice by the Gender Identity in U.S. Surveillance and the Williams Institute at the University of California, Los Angeles School of Law (Gender Identity in U.S. Surveillance (GenIUSS), 2014). We asked participants: “What is your birth sex according to your ID card?” (response options included: “male or female”) and “What is your deeply felt sense of gender identity?”. Sexual attraction was assessed by a third question “Who are you attracted to?”. From these three questions, eight subgroups were created, which included: lesbian woman, defined as a cis (i.e., gender identity corresponds with biological sex) woman attracted to women or self-identified as lesbian in question #2 “What is your deeply felt sense of gender identity?”; gay man, defined as a cis man attracted to men or self-identified as gay in question #2; bisexual man, defined as a cis man attracted to both men and women; bisexual woman, defined as a cis woman attracted to both men and women; transgender man, defined as assigned female at birth and identified as male, tom or ponae (individuals who identify as tom or ponae are included into the transgender man category as the terms can refer to either trans man or masculine presenting lesbian) (United Nations Development Programme, 2019); transgender woman, defined as assigned male at birth and self-identified as female, sao praphet song or kathoey; genderqueer/non-binary, defined as assigned male or female at birth and self-identified as non-binary regardless of sexual attraction; and other, which includes respondents who did not fit in any of these categories. The categories of bisexual men (n=22) and women (n=98) were combined after observing low frequencies in the bisexual men category. A ninth subgroup was created by asking participants: “Were you born with a variation of sex characteristics (this is sometimes called intersex)?” Individuals who responded “Yes” were categorized as intersex, regardless of their reported gender identity or sexual attraction due to the low number of respondents self-identifying as intersex.
We included several socio-demographic variables to account for potential confounders in the analysis, including: age (continuous); education (≥Bachelor’s degree vs. ≤ Vocational certificate (Por Wor Sor or Por Wor Tor) or diploma); place of residence and birth (discordant vs. concordant), defined as whether the participant’s current place of residence is the same as their place of birth (under UCS, designated healthcare facilities are typically assigned to the health district of the individual’s place of birth, thus access could be impeded if an individual resides elsewhere in the country) (Paek et al., 2016); monthly income (≤฿30,000 vs. > ฿30,000 in Thai Baht; approximately US$930); and employment status (unemployed vs. employed or student). We also included a range of healthcare-related characteristics, including: type of health insurance scheme (CSMBS vs. SSS vs. UCS [reference]); ever received HIV testing (yes vs. no), included as HIV-related care in Thailand has been shown to improve service delivery and access, in part due to the prominent role of civil society organizations (U.S. President’s Emergency Plan for AIDS Relief, 2019; Vannakit et al., 2020); and gender concealment in healthcare settings (always/usually/sometimes vs. rarely/never), where participants were asked: “Do you hide your gender expression (expressing your gender with an outward display of the ways in which you dress, speak and behave) when you visit a hospital or a health provider?” We also controlled for sexual/gender identities that were associated with the outcome in bivariable analyses at the p<0.05 level.
Data analyses
We estimated the crude relationships between explanatory variables and both outcome measures (difficulty accessing primary and mental healthcare) using bivariable logistic regression. The adjusted relationships were estimated through the construction of two multivariable logistic regression models for each of the two outcomes. The models included all potential confounders listed above. In the sub-analysis, we examined the categories of SGM who reported gender concealment when accessing healthcare. All p-values were two-sided and all statistical analyses were conducted using R, version 3.6.0. (RStudio Team, 2017)
RESULTS
In total, the analytic sample included 1350 LGBTQI+ participants (Table 2), including 218 (16.1%) gay men, 234 (17.3%) lesbian women, 218 (16.1%) transgender men, 213 transgender women (15.8%), 176 (13.0%) genderqueer/non-binary persons, 120 (8.9%) bisexual men/women, 72 (5.3%) intersex persons and 99 (7.3%) other sexual/gender identity persons. The majority of the sample resided in the Greater Bangkok region (765, 56.7%) followed by Central Thailand (171, 12.7%), North Thailand (163, 12.1%), Northeast Thailand (159, 11.8%), and South Thailand (92, 6.3%) region (data not shown). The median age was 27 (1st and 3rd Quartile [Q]: 23, 33) years and the median scores of perceived and enacted stigma were 3.8 (1st and 3rd Q: 2.8, 4.8) and 1.6 (1st and 3rd Q: 1.1, 2.3) (all scores were out of 7.0), respectively. In addition, 365 (27.0%) participants reported actively hiding their gender expression to access healthcare. Participants also reported being the beneficiaries of the following health insurance schemes: UCS (623, 46.1%), SSS (561, 41.6%), and CSMBS (166, 12.3%). Among this sample, 169 (12.5%) participants reported difficulty accessing primary healthcare, while 269 (19.9%) participants reported difficulty accessing mental healthcare services.
The first multivariable model with the difficulty accessing primary healthcare outcome is shown in Table 3. As shown, after adjusting for a range of potential confounders, individuals who experienced higher levels of enacted stigma were significantly more likely to report difficulty accessing primary healthcare services (Adjusted Odds Ratio [AOR] = 1.34; 95% CI: 1.11 – 1.62). Also, unemployment and self-identifying as intersex had statistically significant associations with difficulties accessing primary healthcare.
The second multivariable model with the difficulty accessing mental healthcare outcome is shown in Table 4. As shown, both perceived and enacted stigma remained significantly and positively associated with difficultly accessing mental healthcare services (AOR: 1.20; 95% CI: 1.07 – 1.35; and AOR: 1.25; 95% CI: 1.07 – 1.48, respectively).
As shown in Figure 1, the sub-analysis results show that the three SGM groups that had the highest proportions of those reporting concealing their gender expression to access healthcare were gay men (43.1%), followed by bisexual men/women (39.8%) and genderqueer/non-binary persons (38.1%).
DISCUSSION
Among our sample of LGBTQI+ people from across Thailand, one in five individuals reported difficulty accessing mental healthcare services and about one in ten reported difficulty accessing primary healthcare. To our knowledge, we are the first to quantify the challenge with healthcare access among SGM in Thailand, which underscores the need and previous calls for government agencies to assess and improve healthcare access for SGM (United Nations Development Programme, 2019). Of concern, almost a third of our participants reported concealing their gender expression when accessing healthcare. In the multivariable analyses, participants who experienced higher levels of enacted stigma were more likely to report difficulty accessing both primary and mental healthcare services, while those who had higher levels of perceived stigma were more likely to report difficulty accessing mental healthcare services only.
We found a higher proportion of LGBTQI+ participants reported difficulty accessing mental healthcare compared to primary healthcare services. This finding could be related to the double stigma associated with mental illness and SGM stigma or related to the constraints of the healthcare system in Thailand (Ojanen et al., 2016). Although psychiatric treatment at public hospitals is covered under the universal healthcare coverage for citizens in Thailand, there exists a shortage of providers who are equipped to address the health needs of SGM (Ojanen et al., 2016). In addition, as with many universal healthcare systems, treatment for mental healthcare is separated from mainstream primary healthcare services, which can create spatial and organizational barriers to care coordination among healthcare providers and access issues among patients (World Health Organization, 2008, 2015). In Thailand, to access secondary and tertiary care individuals must have a referral from a primary care or designated provider (Limwattananon et al., 2007; Paek et al., 2016); who often receive minimal training on providing care for SGM (Ojanen et al., 2016). This forces SGM to navigate and negotiate with potentially stigmatizing health systems to receive care and referrals to mental healthcare services (Ojanen et al., 2016). There have been international calls for healthcare systems to deliver care through an integrated model of care (Black et al., 2020; Centre for Addiction and Mental Health, 2016; Kates et al., 2011; Office of the Surgeon General (US), 2016; Salway et al., 2019a, b; World Health Organization, 2008, 2015), especially for marginalized populations who often experience underfunded and fragmented healthcare services (World Health Organization, 2015). An integrated model of care aims for care to be interdisciplinary, holistic, and people-centered through the unification of several healthcare providers at one geographic location, including social workers, nurses, psychologists and physicians (Centre for Addiction and Mental Health, 2016; World Health Organization, 2008, 2015). The World Health Organization has encouraged all healthcare systems worldwide to adopt people-centred and integrated health services to meet the growing demands for the treatment of noncommunicable diseases, mental health, and injuries (World Health Organization, 2008, 2015).
We also found perceived stigma had an independent and positive association with difficulty accessing mental healthcare services, but not with primary care services. These finding may be related to the specific barriers within mental healthcare settings for SGM, including the harmful effects of pathologizing non-heterosexual sexualities and gender identities (Ojanen et al., 2016; Snow et al., 2019; United Nations Human Rights Office Of The High Commissioner, 2020). In the Thai context, media has played a large role in portraying SGM negatively, including equating SGM status as a pathology (Burapha University, United Nations Development Programme, 2017; Winter et al., 2018). Although evidence of conversion therapy (i.e., the pseudoscientific practice and belief that sexual orientation can and should be changed) has been documented in the Thai context (Ojanen et al., 2016; United Nations Human Rights Office Of The High Commissioner, 2020), it has been noted by some scholars that these attempts are generally rare (Ojanen et al., 2016). However, in previous qualitative research, some SGM in Thailand reported that anticipating mental healthcare providers as not accepting of one’s gender identity contributed to their avoidance of mental healthcare services (Ojanen et al., 2016). This is also in line with a systematic review that examined barriers to mental healthcare for transgender and gender-nonconforming adults, where fears of being pathologized were found to be a major barrier to healthcare access (Snow et al., 2019).
It is important to note that our perceived and enacted stigma measurements assess stigma experienced across one’s life-course, and thus requires multi-level interventions to reduce the overall stigma experienced by SGM in Thai society. A recent scoping review on SGM inclusion and human rights in Thailand found a broad consensus among the literature, including among leading intergovernmental and non-governmental organizations, for the need for interventions across legal, education, health, family, and economic settings to improve the social exclusion faced by SGM in these settings (Newman et al., 2021). The strongest priorities identified in the review included general LGBT+ antidiscrimination legislation and legal recognition of same-sex marriage and ability to change one’s gender (Newman et al., 2021). Pre-post studies in the US has demonstrated the consequential effects of the social and legal climate (i.e., anti-discrimination and same-sex marriage laws) for the health of LGB, including healthcare utilization (Hatzenbuehler et al., 2011; Solazzo et al., 2018). Another US study found that state-level protective policies for LGB were significantly protective of psychiatric disorders (i.e., generalized anxiety disorder, post-traumatic stress disorder, and dysthymia) compared to states without these policies (Hatzenbuehler et al., 2009). Taken together with our findings, considerations to improve the social and legal climate influences for SGM in Thailand are needed to reduce the experiences of stigma observed across Thai SGM’s life-course.
We also found that individuals who experienced elevated levels of enacted stigma were significantly more likely to report difficulty accessing both primary and mental healthcare services. The powerful detrimental impacts of enacted stigma on healthcare access are consistent with the international literature (Alencar Albuquerque et al., 2016; Ayhan et al., 2019; Snow et al., 2019; White Hughto et al., 2015; Zeeman et al., 2019). Given these findings, it is important to ensure culturally safe care particularly for those SGM who experienced explicit forms of sexual and gender stigma. However, available data suggests Thailand needs significant investment in this area (Ojanen et al., 2016; Suriyasarn, 2014; United Nations Development Programme, 2019, 2020; United Nations Development Programme & USAID, 2014). For instance, previous qualitative studies have showed reports of SGM being forced to be admitted to healthcare wards based on their assigned biological sex (United Nations Development Programme, 2019; United Nations Development Programme & USAID, 2014), which contributes to SGM’s avoidance of healthcare settings (United Nations Development Programme & USAID, 2014). Taken together with our findings, there is a need to implement national training for SGM-specific culturally competent care to all existing and future healthcare professionals (McClain et al., 2016; Sekoni et al., 2017). In addition, there is a need for improving guidelines and official policies at the health system level to include SGM-specific needs (i.e., in-patient accommodation based on SGM identity). A recent study has sought to define cultural competencies for SGM among mental health practitioners in the Thai context (Ojanen et al., 2021), where acceptance of sexual and gender diversity, feminist counseling techniques, and respect of self-determination, among other competencies, were identified as being crucial components (Ojanen et al., 2021). Further, a systematic review has demonstrated the benefits of SGM-specific educational curricula for healthcare professionals (Sekoni et al., 2017).
To foster an environment where SGM feel safe to disclose their needs, the inclusion of trained SGM lay providers may be an effective strategy (Vannakit et al., 2020; Yang et al., 2020). Specifically, in Thailand, the Key Population-led Health Services (KPLHS) model was developed by and for SGM and other priority populations (e.g., sex worker populations) to task shift HIV and healthcare services (Vannakit et al., 2020; Yang et al., 2020). In this context, affirming care and sexual health services are provided (Sekoni et al., 2017), which has shown to be effective in service delivery to SGM (Vannakit et al., 2020). Additionally, a systematic review has shown that involving SGM in the training, design, or facilitation of culturally-competent care enhanced the effects of training (Sekoni et al., 2017). Therefore, healthcare systems should consider incorporating key populations into delivery and training of general and mental healthcare (beyond HIV care) as a means to provide a supportive environment for SGM.
We also observed that almost a third of the sample reported hiding their gender expression to access care. Our finding is consistent with the international literature that has also documented identity concealment as a barrier to care among SGM (Alencar Albuquerque et al., 2016; Ayhan et al., 2019). The need to conceal gender or sexual identity is a barrier to healthcare that can endanger SGM’s health as a result of poor quality of care (e.g., concealing can lead to missed opportunities for preventive and SGM-specific care and inadequate/inappropriate medical history taking) (Alencar Albuquerque et al., 2016; Ayhan et al., 2019). In general, we observed that sexual minority groups had a higher proportion of those hiding their gender expression in healthcare settings compared to transgender groups. Although an individual’s gender expression can vary vastly between and within SGM, our finding may be reflective of an individual’s ability to conceal their identity to avoid SGM stigma. Within the Thai context, it has been noted that the level of stigma experienced by SGM largely depends on whether individuals conform to the social demands to hide their gender identity (Ojanen et al., 2016; Suriyasarn, 2014; United Nations Development Programme, 2019). Some scholars in Thailand have noted that bisexual people may be able to evade stigma based on their ability to remain ‘invisible’ (Ojanen et al., 2016). In addition, change of gender is not legally recognized in Thailand, which contributes to ongoing difficulties in receiving gender-affirming care in healthcare settings among SGM (e.g., transgender women being denied in-patient accommodation in the women’s ward of the hospital) (United Nations Development Programme, 2019). This is consistent with our hypothesis that transgender respondents may be less able to conceal their gender expression as it is more difficult to do so. Thus, interventions must consider the differences among SGM to support the diverse needs of SGM in Thailand.
Although our primary study aims were to examine the relationship between multiple dimensions of stigma and difficulties in accessing primary and mental healthcare, we observed notable associations between SGM who reported being unemployed and difficulties accessing primary healthcare, which warrants further research. Similarly, we observed a significant link between intersex people and difficulty in accessing primary healthcare. Given the pre-existing inequities experienced by this community (as shown in international contexts) (Zeeman & Aranda, 2020), the dearth of research among intersex people internationally and in the Thai context (Ojanen et al., 2016), research is needed to investigate barriers to care and other determinants of health among this population.
Our study has several limitations. Although our measurement of stigma was adapted from a previously validated scale on sexual stigma among men who have sex with men (MSM) populations in the US and queer women in Canada (Díaz et al., 2001; Logie & Earnshaw, 2015), it has not been validated in the Thai language. Due to a scarcity of validated measurements of stigma in the Thai context, the previously validated sexual stigma scale was adapted to the Thai context through collaborations between UNDP and several LGBT-organizations. Both the enacted- and perceive-stigma sub-scales demonstrated adequate internal consistency (Cronbach’s alpha ≥0.70). Similarly, the question used to assess perceived difficulty in accessing primary and mental healthcare services was not validated, but was created by UNDP through consultation with national and regional survey reference groups (United Nations Development Programme, 2019). Further, all of our variables were measured using participant self-report, which may introduce some response bias. As with most large-scale online surveys, no suitable sampling frame exists as the survey is limited to those with internet access. In addition, we also did not randomly recruit participants, which reduces our ability to generalize our findings to all LGBTQI+ populations in Thailand, and may mischaracterize SGM across several sociodemographic, employment and health-related factors (Salway et al., 2019a, b). Namely, our sample had high levels of employment/students and educational attainment, which may indicate a selection bias in favour of more stable and/or well-resourced individuals. Also, the overall distribution of enrolment in UCS, SSS, and CSMBS was different from that reported at the national level where about 75% of the population are UCS beneficiaries (Paek et al., 2016). In addition, the majority of our sample resided in the Greater Bangkok area, the largest metropolitan city in Thailand, thus our ability to discern rural/urban dynamics to difficulty accessing healthcare is limited. Although we did extensively adjust for potential confounding variables, the observational research study design is limited by potential unmeasured confounding variables. Our assessment of SGM stigma is also limited as it does not include measures related to internalized stigma (another intraindividual dimension of stigma) (Herek, 2007). In addition, the cross-sectional nature of this study does not allow us to determine the temporal sequences of associations found in our study, specifically between SGM stigma and difficultly accessing healthcare services.
CONCLUSION
In our sample of LGBTQI+ people in Thailand, we found that one in five participants had difficulty accessing mental healthcare, while one in ten had difficulty accessing primary healthcare services. About a third of the sample actively hid their gender expression to access care. Further, enacted stigma was independently associated with difficulty accessing both primary and mental healthcare services, while perceived stigma was independently associated with difficulty accessing mental healthcare services only. Our findings suggest that addressing the issue of access to care requires multi-level and multidisciplinary interventions that address SGM stigma within and outside of healthcare settings, including training for providers in culturally competent care for SGM. Further, providing integrated care for SGM may be an effective strategy to reduce barriers in care coordination between primary and mental healthcare services.
Change history
17 March 2022
A Correction to this paper has been published: https://doi.org/10.1007/s11469-022-00776-3
REFERENCES
Alencar Albuquerque, G., de Lima Garcia, C., da Silva Quirino, G., Alves, M. J. H., Belém, J. M., dos Santos Figueiredo, F. W., da Silva Paiva, L., Do Nascimento, V. B., da Silva Maciel, É., Valenti, V. E., de Abreu, L. C., & Adami, F. (2016). Access to health services by lesbian, gay, bisexual, and transgender persons: systematic literature review. BMC International Health and Human Rights, 16, 2. https://doi.org/10.1186/s12914-015-0072-9
Ayhan, C. H. B., Bilgin, H., Uluman, O. T., Sukut, O., Yilmaz, S., & Buzlu, S. (2019). A Systematic Review of the Discrimination Against Sexual and Gender Minority in Health Care Settings. International Journal of Health Services, 50(1), 44–61. https://doi.org/10.1177/0020731419885093
Black, S., Salway, T., Dove, N., Shoveller, J., & Gilbert, M. (2020). From silos to buckets: a qualitative study of how sexual health clinics address their clients’ mental health needs. Canadian Journal of Public Health, 111(2), 220–228. https://doi.org/10.17269/s41997-019-00273-6
Bockting, W. O., Miner, M. H., Swinburne Romine, R. E., Hamilton, A., & Coleman, E. (2013). Stigma, Mental Health, and Resilience in an Online Sample of the US Transgender Population. American Journal of Public Health, 103(5), 943–951. https://doi.org/10.2105/AJPH.2013.301241
Brooks, V. (1981). Minority stress and lesbian women. Lexington Books.
Burapha University, United Nations Development Programme. (2017). A tool for change: Working with the media on issues relating to sexual orientation, dender identity, expression and sex characteristics in thailand. https://www.th.undp.org/content/dam/thailand/docs/publications/LGBTI/UNDP_Thailand_A-tool-for-change.pdf. Accessed Dec 2020.
Centre for Addiction and Mental Health. (2016). Mental Health and Primary Care Policy Framework. https://www.camh.ca/-/media/files/pdfs---public-policy-submissions/primarycarepolicyframework_march2016-pdf. Accessed Dec 2020.
Chongthawonsatid, S. (2021). Identification of Unmet Healthcare Needs: A National Survey in Thailand. Journal of Preventive Medicine and Public Health = Yebang Uihakhoe Chi, 54(2), 129–136. https://doi.org/10.3961/jpmph.20.318
Cochran, W. (1953). Sampling Techniques. John Wiley & Sons, Ltd.
Díaz, R. M., Ayala, G., Bein, E., Henne, J., & Marin, B. V. (2001). The impact of homophobia, poverty, and racism on the mental health of gay and bisexual Latino men: findings from 3 US cities. American Journal of Public Health, 91(6), 927–932. https://doi.org/10.2105/ajph.91.6.927
DiPlacido, J., & Fallahi, C. R. (2020). Stigma and Sexual and Gender Minority Mental Health. In E. D. Rothblum (Ed.), The Oxford Handbook of Sexual and Gender Minority Mental Health (pp. 419–425). Oxford University Press.
Fongkaew, K., Khruataeng, A., Unsathit, S., Khamphiirathasana, M., Jongwisan, N., Arlunaek, O., & Byrne, J. (2019). “Gay Guys are Shit-Lovers” and “Lesbians are Obsessed With Fingers”: The (Mis)Representation of LGBTIQ People in Thai News Media. Journal of Homosexuality, 66(2), 260–273. https://doi.org/10.1080/00918369.2017.1398026
Gender Identity in U.S. Surveillance (GenIUSS). (2014). Best Practices for Asking Questions to Identify Transgender and Othe r Gender Minority Re spondents on Population-Based Surveys. https://williamsinstitute.law.ucla.edu/publications/geniuss-trans-pop-based-survey/. Accessed Dec 2020.
Hatzenbuehler, M. L., Keyes, K. M., & Hasin, D. S. (2009). State-Level Policies and Psychiatric Morbidity In Lesbian, Gay, and Bisexual Populations. American Journal of Public Health, 99(12), 2275–2281. https://doi.org/10.2105/AJPH.2008.153510
Hatzenbuehler, M. L., O’Cleirigh, C., Grasso, C., Mayer, K., Safren, S., & Bradford, J. (2011). Effect of Same-Sex Marriage Laws on Health Care Use and Expenditures in Sexual Minority Men: A Quasi-Natural Experiment. American Journal of Public Health, 102(2), 285–291. https://doi.org/10.2105/AJPH.2011.300382
Hatzenbuehler, M. L., Phelan, J. C., & Link, B. G. (2013). Stigma as a fundamental cause of population health inequalities. American Journal of Public Health, 103(5), 813–821. https://doi.org/10.2105/AJPH.2012.301069
Herek, G. M. (2007). Confronting Sexual Stigma and Prejudice: Theory and Practice. Journal of Social Issues, 63(4), 905–925. https://doi.org/10.1111/j.1540-4560.2007.00544.x
Herek, G. M. (2016). A Nuanced View of Stigma for Understanding and Addressing Sexual and Gender Minority Health Disparities. LGBT Health, 3(6), 397–399. https://doi.org/10.1089/lgbt.2016.0154
Kates, N., Mazowita, G., Lemire, F., Jayabarathan, A., Bland, R., Selby, P., Isomura, T., Craven, M., Gervais, M., & Audet, D. (2011). The Evolution of Collaborative Mental Health Care in Canada: A Shared Vision for the Future. Canadian Journal of Psychiatry, 56(5), 1–10.
King, M., Semlyen, J., Tai, S. S., Killaspy, H., Osborn, D., Popelyuk, D., & Nazareth, I. (2008). A systematic review of mental disorder, suicide, and deliberate self harm in lesbian, gay and bisexual people. BMC Psychiatry, 8(1), 70. https://doi.org/10.1186/1471-244X-8-70
Kittiteerasack, P., Matthews, A. K., Steffen, A., Corte, C., McCreary, L. L., Bostwick, W., Park, C., & Johnson, T. P. (2020). The influence of minority stress on indicators of suicidality among lesbian, gay, bisexual and transgender adults in Thailand. Journal of Psychiatric and Mental Health Nursing, n/a(n/a). https://doi.org/10.1111/jpm.12713
Kittiteerasack, P., Steffen, A., & Matthews, A. (2019). The Influence of Minority Stress on Level of Depression among Thai LGBT Adults. Jurnal Keperawatan Indonesia. https://doi.org/10.7454/jki.v0i0.1073
Krueger, E. A., Holloway, I. W., Lightfoot, M., Lin, A., Hammack, P. L., & Meyer, I. H. (2020). Psychological Distress, Felt Stigma, and HIV Prevention in a National Probability Sample of Sexual Minority Men. LGBT Health, 7(4), 190–197. https://doi.org/10.1089/lgbt.2019.0280
Limwattananon, S., Tangcharoensathien, V., & Prakongsai, P. (2007). Catastrophic and poverty impacts of health payments: results from national household surveys in Thailand. Bulletin of the World Health Organization, 85(8), 600–606. https://doi.org/10.2471/blt.06.033720
Logie, C. H., & Earnshaw, V. (2015). Adapting and Validating a Scale to Measure Sexual Stigma among Lesbian, Bisexual and Queer Women. PLoS ONE, 10(2), e0116198. https://doi.org/10.1371/journal.pone.0116198
Manalastas, E. J., Ojanen, T., Torre, B., Ratanashevorn, R., Choong, C., Kumaresan, V., & Veeramuthu, V. (2017). Homonegativity in Southeast Asia: Attitudes Toward Lesbians and Gay Men in Indonesia, Malaysia, the Philippines, Singapore, Thailand, and Vietnam. Asia-Pacific Social Science Review, 17, 25–33.
McClain, Z., Hawkins, L. A., & Yehia, B. R. (2016). Creating Welcoming Spaces for Lesbian, Gay, Bisexual, and Transgender (LGBT) Patients: An Evaluation of the Health Care Environment. Journal of Homosexuality, 63(3), 387–393. https://doi.org/10.1080/00918369.2016.1124694
McNeil, J., Ellis, S. J., & Eccles, F. J. R. (2017). Suicide in trans populations: A systematic review of prevalence and correlates. In Psychology of Sexual Orientation and Gender Diversity (Vol. 4, Issue 3, pp. 341–353). Educational Publishing Foundation. https://doi.org/10.1037/sgd0000235
Meyer, I. H. (2003). Prejudice, social stress, and mental health in lesbian, gay, and bisexual populations: Conceptual issues and research evidence. In Psychological Bulletin (Vol. 129, Issue 5, pp. 674–697). American Psychological Association. https://doi.org/10.1037/0033-2909.129.5.674
Newman, P. A., Reid, L., Tepjan, S., & Akkakanjanasupar, P. (2021). LGBT+ inclusion and human rights in Thailand: a scoping review of the literature. BMC Public Health, 21(1), 1816. https://doi.org/10.1186/s12889-021-11798-2
Nimmawitt, N., Wannarit, K., & Pariwatcharakul, P. (2020). Thai psychiatrists and burnout: A national survey. PLoS ONE, 15(4), e0230204. https://doi.org/10.1371/journal.pone.0230204
Office of the Surgeon General (US). (2016). Facing Addiction in America: The Surgeon General’s Report on Alcohol, Drugs, and Health. https://addiction.surgeongeneral.gov/sites/default/files/surgeon-generals-report.pdf. Accessed Dec 2020.
Ojanen, T., Ratanashevorn, R., & Boonkerd, S. (2016). Gaps in responses to LGBT issues in Thailand: Mental health research, services, and policies. Psychology of Sexualities Review, 7, 41–59.
Ojanen, T. T., Phukao, D., Pimpawun, B., & Rungreangkulkij, S. (2021). Defining Mental Health Practitioners’ LGBTIQ Cultural Competence in Thailand. Journal of Population and Social Studies, 29, 158–176. https://doi.org/10.25133/JPSSv292021.010
Paek, S. C., Meemon, N., & Wan, T. T. H. (2016). Thailand’s universal coverage scheme and its impact on health-seeking behavior. SpringerPlus, 5(1), 1952. https://doi.org/10.1186/s40064-016-3665-4
RStudio Team. (2017). RStudio: Integrated Development for R. (3.4.2). RStudio, Inc.
Salway, T., Ferlatte, O., Shoveller, J., Purdie, A., Grennan, T., Tan, D. H. S., Consolacion, T., Rich, A. J., Dove, N., Samji, H., Scott, K., Blackwell, E., Mirau, D., Holgerson, N., Wong, J., & Gilbert, M. (2019). The Need and Desire for Mental Health and Substance Use–Related Services Among Clients of Publicly Funded Sexually Transmitted Infection Clinics in Vancouver, Canada. Journal of Public Health Management and Practice, 25(3). https://journals.lww.com/jphmp/Fulltext/2019/05000/The_Need_and_Desire_for_Mental_Health_and.17.aspx. Accessed Dec 2020.
Salway, T. J., Morgan, J., Ferlatte, O., Hawkins, B., Lachowsky, N. J., & Gilbert, M. (2019). A Systematic Review of Characteristics of Nonprobability Community Venue Samples of Sexual Minority Individuals and Associated Methods for Assessing Selection Bias. LGBT Health, 6(5), 205–215. https://doi.org/10.1089/lgbt.2018.0241
Sekoni, A. O., Gale, N. K., Manga-Atangana, B., Bhadhuri, A., & Jolly, K. (2017). The effects of educational curricula and training on LGBT-specific health issues for healthcare students and professionals: a mixed-method systematic review. Journal of the International AIDS Society, 20(1), 21624. https://doi.org/10.7448/IAS.20.1.21624
Snow, A., Cerel, J., Loeffler, D. N., & Flaherty, C. (2019). Barriers to Mental Health Care for Transgender and Gender-Nonconforming Adults: A Systematic Literature Review. Health & Social Work, 44(3), 149–155. https://doi.org/10.1093/hsw/hlz016
Solazzo, A., Brown, T. N., & Gorman, B. K. (2018). State-level climate, anti-discrimination law, and sexual minority health status: An ecological study. Social Science & Medicine, 196, 158–165. https://doi.org/10.1016/j.socscimed.2017.11.033
Suriyasarn, B. (2014). Gender identity and sexual orientation in Thailand. https://www.ilo.org/wcmsp5/groups/public/---asia/---ro-bangkok/---sro-bangkok/documents/publication/wcms_356950.pdf. Accessed Dec 2020.
Sutter, M., & Perrin, P. B. (2016). Discrimination, mental health, and suicidal ideation among LGBTQ people of color. In Journal of Counseling Psychology (Vol. 63, Issue 1, pp. 98–105). American Psychological Association. https://doi.org/10.1037/cou0000126
United Nations Development Programme. (2019). A national survey on experiences of discrimination and social attitudes towards LGBT people in Thailand. https://www.undp.org/content/undp/en/home/librarypage/democratic-governance/tolerance-but-not-inclusion.html. Accessed Dec 2020.
United Nations Development Programme. (2020). Stories of Stigma: Exploring stigma and discrimination against Thai transgender people while accessing health care and in other settings. https://www.undp.org/content/dam/thailand/docs/UNDP-THStoriesOfStigma_Eng.pdf .
United Nations Development Programme, & USAID. (2014). Being LGBT in Asia Country Reports - Thailand. https://www.refworld.org/pdfid/54ed82784.pdf. Accessed Dec 2020.
United Nations Human Rights Office Of The High Commissioner. (2020). Report on conversion therapy. https://www.ohchr.org/EN/Issues/SexualOrientationGender/Pages/ReportOnConversiontherapy.aspx. Accessed Dec 2020.
U.S. President’s Emergency Plan for AIDS Relief. (2019). Asia Region Operational Plan, ROP 2019 Strategic Direction Summary. https://www.state.gov/wp-content/uploads/2019/09/Asia-Regional_COP19-Strategic-Directional-Summary_public.pdf. Accessed Dec 2020.
Vannakit, R., Janyam, S., Linjongrat, D., Chanlearn, P., Sittikarn, S., Pengnonyang, S., Janamnuaysook, R., Termvanich, K., Ramautarsing, R., Phanuphak, N., & Phanuphak, P. (2020). Give the community the tools and they will help finish the job: key population-led health services for ending AIDS in Thailand. Journal of the International AIDS Society, 23(6), e25535. https://doi.org/10.1002/jia2.25535
White Hughto, J. M., Reisner, S. L., & Pachankis, J. E. (2015). Transgender stigma and health: A critical review of stigma determinants, mechanisms, and interventions. Social Science & Medicine, 147, 222–231. https://doi.org/10.1016/j.socscimed.2015.11.010
Winter, S., Davis-McCabe, C., Russell, C., Wilde, D., Thanh Ha, C., Peeranee Suparak, A., & Wong, J. (2018). Denied Work – An audit of employment discrimination on the basis of gender identity in South-East Asia. https://www.asia-pacific.undp.org/content/rbap/en/home/library/democratic_governance/hiv_aids/denied-work.html. Accessed Dec 2020.
World Health Organization. (2008). Integrating Mental Health Into Primary Care: A Global Perspective. World Health Organization.
World Health Organization. (2015). WHO global strategy on people-centred and integrated health services Interim Report on people-centred and Interim report. https://apps.who.int/iris/bitstream/handle/10665/155002/WHO_HIS_SDS_2015.6_eng.pdf;jsessionid=535F5B04B09B46FB8CD1AABA8AF8CB34?sequence=1. Accessed Dec 2020.
World Health Organization. (2017). Mental Health ATLAS 2017 Member State Profile. https://www.who.int/mental_health/evidence/atlas/profiles-2017/THA.pdf. Accessed Dec 2020.
World Health Organization. (2018). Decade for health workforce strengthening in the South-East Asia Region 2015–2024; Second review of progress. https://apps.who.int/iris/bitstream/handle/10665/274310/9789290226574-eng.pdf?sequence=1&isAllowed=y. Accessed Dec 2020.
World Health Organization, & United Nations Human Rights Office Of The High Commissioner. (2008). The Right to Health. https://www.who.int/gender-equity-rights/knowledge/right-to-health-factsheet31.pdf?ua=1. Accessed Dec 2020.
Yang, F., Janamnuaysook, R., Boyd, M. A., Phanuphak, N., & Tucker, J. D. (2020). Key populations and power: people-centred social innovation in Asian HIV services. The Lancet. HIV, 7(1), e69–e74. https://doi.org/10.1016/S2352-3018(19)30347-9
Zeeman, L., & Aranda, K. (2020). A Systematic Review of the Health and Healthcare Inequalities for People with Intersex Variance. International Journal of Environmental Research and Public Health, 17(18). https://doi.org/10.3390/ijerph17186533
Zeeman, L., Sherriff, N., Browne, K., McGlynn, N., Mirandola, M., Gios, L., Davis, R., Sanchez-Lambert, J., Aujean, S., Pinto, N., Farinella, F., Donisi, V., Niedźwiedzka-Stadnik, M., Rosińska, M., Pierson, A., Amaddeo, F., Network, =Health4LGBTI. (2019). A review of lesbian, gay, bisexual, trans and intersex (LGBTI) health and healthcare inequalities. European Journal of Public Health, 29(5), 974–980. https://doi.org/10.1093/eurpub/cky226
Acknowledgment
The authors thank the study participants and Love Frankie, Asian Institute of Technology and Prince of Songkhla University for their contribution to the research.
Funding
The survey was funded by UNDP’s Being LGBTI in Asia and the Pacific programme, with generous financial support by the Embassy of Sweden in Bangkok and USAID.
KH holds the St. Paul’s Hospital Chair in Substance Use Research and is supported in part by a Michael Smith Foundation for Health Research (MSFHR) Scholar Award, and the St. Paul’s Foundation.
The data and code used in this study are available upon request and approval from UNDP.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Soroush Moallef conducted the statistical analyses and wrote the first draft of the manuscript, with guidance and assistance from Kanna Hayashi. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Disclosure Statement
No conflicts of interest declared, including no financial or non-financial interests to declare.
Ethics approval/Ethical standards
This survey research project was approved by the Asian Institute of Technology Research Ethics Review Committee. The manuscript does not contain clinical studies or patient data.
Consent to participate
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Moallef, S., Salway, T., Phanuphak, N. et al. The relationship between sexual and gender stigma and difficulty accessing primary and mental healthcare services among LGBTQI+ populations in Thailand: Findings from a national survey. Int J Ment Health Addiction 20, 3244–3261 (2022). https://doi.org/10.1007/s11469-021-00740-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11469-021-00740-7