Abstract
Purpose
To demonstrate the usefulness of hair testing to determine exposure pattern to fentanyls.
Methods
A 43-year-old male was found unconscious with respiratory depression 15 min after snorting 3 mg of a powder labeled as butyrylfentanyl. He was discharged from hospital within 2 days without blood or urine testing. Two locks of hair were sampled 1 month (M1 A: 0–2 cm (overdose time frame); B: 2–4 cm; C: 4–6 cm) and 1 year (Y1: A: 0–2 cm; B: 2–4 cm) later to monitor his exposure to drugs of abuse by liquid chromatography–tandem mass spectrometry after liquid-liquid extraction.
Results
Hair analysis at M1 showed a repetitive exposure to 3-fluorofentanyl (A/B/C: 150/80/60 pg/mg) with higher concentration in segment A reflecting the overdose period. The non-detection of butyrylfentanyl was consistent with the analysis of the recovered powder identified as 3-fluorofentanyl. Furanylfentanyl (40/20/15 pg/mg) and fentanyl (37/25/3 pg/mg) were also detected in hair. The second hair analysis at Y1 showed the use of three new fentanyls, with probably repetitive exposures to methoxyacetylfentanyl (A/B: 500/600 pg/mg), and single or few exposures to carfentanil (2.5/3 pg/mg) and acetyl fentanyl (1/1 pg/mg). A decreasing exposure to 3-fluorofentanyl (25/80 pg/mg), and increasing consumption of furanylfentanyl (310/500 pg/mg) and fentanyl (620/760 pg/mg) were also observed despite methadone treatment initiation. The patient claimed not consuming three out of the six detected fentanyls.
Conclusions
We report single or repetitive exposure to several fentanyls using hair testing. To our knowledge, this is the first demonstration of 3-fluorofentanyl and methoxyacetylfentanyl in hair samples collected from an authentic abuser.
Similar content being viewed by others
Introduction
Over the last few years, new synthetic opioids (NSOs), primarily fentanyl derivatives are increasingly implicated in overdose deaths, and have caused a global health concern. Among the 70,237 drug-related deaths estimated in 2017 in the US, the sharpest increase occurred among those related to fentanyl analogs with more than 28,400 overdose deaths which represents 45.2% increase from 2016 to 2017 [1, 2]. In Europe, their use appears to be geographically localized, but the number of synthetic opioids has grown rapidly since the first substance was reported in 2009. In fact, around 50 NSOs have been reported to the EU Early Warning System with 11 being reported for the first time in 2018 [3]. From 2015 to early 2018, the European Monitoring Center for Drugs and Drug Addiction (EMCDDA) has conducted eight joint investigations with Europol on fentanyls that have caused serious concern at European level. The two agencies investigated acetylfentanyl, acryloylfentanyl and furanylfentanyl, 4-fluoroisobutyrylfentanyl (4F-iBF), tetrahydrofuranylfentanyl (THF-F), carfentanil, methoxyacetylfentanyl and cyclopropylfentanyl. These substances have been involved in more than 250 deaths, many of which were attributed directly to these substances [4]. Reported overdose cases include people who unknowingly buy adulterated heroin, other illicit drugs or pain relievers [3, 5].
The risk of life-threatening poisoning or deaths by NSOs is being enhanced by the following reasons: most NSOs are particularly potent on µ-opioid receptors (10 up to 10,000 more potent than morphine) and can be toxic at very low dose due to severe respiratory depression [6]; high bioavailability using routes of administration that allow substances to rapidly reach the central nervous system such as injecting, snorting, and inhalation; ease of synthesis, purchase at low cost, and their adulteration especially with heroin facilitate the poisonings; they, in many cases, are undetectable by the standard screening methods [4]. A recent EMCDDA study has shown that not all laboratories have the capacity to detect the more uncommon substances [3]. Thus, the prevalence of these substances in opioid-related poisonings and deaths is most likely underreported.
In the actual context of opioids crisis, more reliable and sensitive methods dedicated to the identification and quantification of NSOs in biological and non-biological matrices are needed. Recently, these analytical methods often based on chromatography (liquid or gas) coupled with mass spectrometry (MS) detection were extensively reviewed [7, 8]. Even if targeted screening is highly sensitive and specific, they remain limited by the unavailability of reference standards [7, 9,10,11,12]. A new approach based on untargeted screening by liquid chromatography–high-resolution mass spectrometry (LC–HRMS) using a shared MS spectral database and without a need for reference standards has emerged in recent years [13,14,15].
To study the prevalence of fentanyl derivatives among other drugs of abuse, the EMCDDA has proposed five strategies as targeted data sources: wastewater or syringe residue analysis, emergency department or drug checking service data, and web surveys [3, 16, 17]. Self-reported use of drugs often includes reporting biases related to users’ ignorance about the products for their consumption which often are different from the ones that they bought, especially in case of NSOs due to adulteration. Wastewater and syringe residue analysis strategies provide more informative data regarding drug use, but remain indirectly linked to the population of the consumers. Even if these approaches are not representative of the general population and present some limitations, they provide useful, timely and complementary data that offer valuable insights into drug use in Europe [5].
On the other hand, the analysis of biological specimens of drug users could be the most accurate and directly linked to their drug consumption. While blood and urine testing can provide useful information of recent exposure to drugs (few hours up to days after consumption), hair testing allows an extensive exposure pattern of past use, as it offers a wide detection window, up to months prior to sampling and is easy to collect. Given that hair is also a rot-proof material that does not decompose, it can be kept for a long period with no special storage conditions (ambient temperature) and retrospectively analyzed, as most substances are stable in the hair matrix. Lastly, unlike conventional matrices like urine, hair sample cannot be adulterated by dilution, for example, to produce negative results [18].
Recently, hair testing has gained an interesting role in harm reduction, which is often used as a therapeutic strategy to disclose how individuals who use drugs learning about exposure may affect their drug taking and their adherence to treatment [10].
However, hair analysis can be tricky, and some common pitfalls should be known to avoid wrong results and interpretation. The sample collection is the first step that should be considered, especially in case of segmental analysis. Given that hair growth differs in each region of the body, the collection of head hair, for example, has to be done in the vertex area behind the head where the growth rate is steady (~ 1 cm/month). Hair strand should also be oriented to distinguish between the proximal (recent) and distal side which can affect the interpretation of consumption trend (increase or decrease) [18]. From the analytical point of view, the analysis of hair samples may be more difficult than conventional matrices like urine, because it requires more preparation steps like decontamination or digestion where losses or degradation of drugs may affect the detection and increase variability of quantitative results. The choices of the right solvent, the extraction time and the analytical instrument are some of the important factors to consider for achieving unambiguous identification and accurate quantification [19].
The most serious pitfalls of hair analysis are in the interpretation of the results. While the incorporation of drugs in hair is dose related, it is well known that there is no good correlation between the dose of a drug taken and hair concentration because of interindividual variation. This can be due to differences in metabolism, frequency of use, purity of drugs, hair color, or the use of cosmetic products (dying, bleaching, etc.) among many factors that affect the incorporation of drugs into the hair matrix. It is, therefore, difficult to speculate on how much or how often an individual used drug. However, intraindividual correlation when analyzing multiple hair segments or different time frame could be used to monitor drug use pattern and detect changes in the frequency (decrease or increase) of use in the same subject [20].
Finally, while a positive result from the analysis of hair suggests that a person has used or been exposed to a drug (including external contamination), a negative hair result, however, does not categorically mean that the person did not use drugs if they have been exposed to a drug infrequently or in low doses. Consequently, it is important that the limitations of the test should be highlighted when reporting the results [18].
Even if this approach remains scarce and requires some particular skills, it deserves to be considered as a direct and long-term indicator of drug exposure. Some prevalence and analytical data regarding new psychoactive substance (NPS) study by hair testing in high-risk populations are now available [21,22,23,24,25,26,27].
In this article, we report a case of a 43-year-old male hospitalized in intensive care unit (ICU) for 3-fluorofentanyl unintentional overdose from a mislabeled product and demonstrate the usefulness of hair to determine his exposure profile to other fentanyl analogs over 1 year.
Materials and methods
Chemicals and reagents
The reference standards of alfentanil, carfentanil, furanylfentanyl, furanylnorfentanyl, butyrylnorfentanyl, acetylnorfentanyl, norcarfetanil, norfentanyl, methylfentanyl, furanylnorfentanyl, methoxyacetylfentanyl, fentanyl-D5, acetylfentanyl-D5 and norfentanyl-D5 were purchased from LGC Standards (Molsheim, France); sufentanyl, fentanyl, and butyrylfentanyl from Lipomed AG (Arlesheim, Switzerland); 3(meta)-fluorofentanyl, ocfentanil and acetylfentanyl from Cayman Chemical Company (Ann Arbor, MI, USA); U-47700 from Chiron AS (Trondheim, Norway); acetonitrile, dichloromethane, hexane, ethyl acetate, formic acid and methanol from Sigma-Aldrich (Paris, France) in MS or high-performance liquid chromatography (HPLC) grade; sodium carbonate and hydrogen carbonate from Prolabo (Paris, France). Ultra-pure water (18 MΩ) was obtained by ultrafiltration with a Q-Pod (Millipore Corp., Molsheim, France). Formate buffer containing 2 mM ammonium formate in 0.1% formic acid was prepared in ultra-pure water and stored after each analysis at +4°C away from light for a maximum of 1 week.
Calibration standards and quality controls
Eight calibration standards containing a mixture of screened fentanyls at 1, 2.5, 5, 10, 50, 100, 500, and 1000 pg/mg of hair were prepared by spiking stock solutions of reference standards with appropriate volume into a 20-mg drug-free hair powder. Quality controls (QCs) were prepared at concentrations of 5, 250 and 750 pg/mg by the same way. Drug-free human hair was obtained from healthy subjects who are not medically treated.
Hair sample preparation
Hair locks were obtained from the posterior vertex. Hair was washed once with warm water and decontaminated twice using dichloromethane (immersion for 2 min in each step). It was then ground into a fine and homogeneous powder using a ball mill (MM200; Fisher Scientific, Illkrich, France). Each 20 mg was incubated in 1 mL of phosphate buffer at pH 5.0 at 95 °C for 10 min, in the presence of an appropriate amount of deuterated internal standards (ISs: fentanyl-D5, acetylfentanyl-D5 and norfentanyl-D5). After spiking the corresponding volume of calibration standard or QC working solution when necessary, liquid-liquid extraction was performed by 4 mL of a mixture of hexane/ethyl acetate (v/v, 1:1). After agitation and centrifugation for 20 min, the organic phase was recovered and evaporated to dryness. The residue was reconstituted in 80 µL of mobile phase and 10 µL was injected into the chromatographic system.
Liquid chromatography–tandem mass spectrometry system and conditions
A liquid chromatography–tandem mass spectrometry (LC–MS/MS) system derived from a previously published method [22] and enriched by the addition of 17 NSOs was employed in the present study. Chromatography was performed on a Dionex Ultimate 3000 pump (ThermoFisher, Les Ulis, France) using a Hypersyl Gold PFP column (100 × 2.1 mm i.d., particle size 1.9 µm) preheated at 30 °C. The mobile phase was a gradient of acetonitrile (A) and 2 mM sodium formate buffer aqueous solution with 0.1% formic acid (B) starting from 20% (A) to 90% (A) in 10 min at a flow rate of 300 μL/min. The total run time was 12 min. Compounds were detected by a TSQ Endura triple-quadrupole mass spectrometer (ThermoFisher) equipped with an electrospray ionization source set in a positive mode with ion spray potential at + 3.5kV. Capillary temperature was set at 350°C. Nitrogen (Nitrox UHPLCMS 18, nitrogen generator; Domnick Hunter, Villefranche sur Saône, France) was employed as sheath gas at 35 arbitrary pressure unit. The argon gas collision-induced dissociation was used with a pressure of 1.5 mTorr. Data were collected in selected reaction monitoring (SRM) mode, with two m/z transitions per analyte. Data acquisition was performed using Xcalibur and LC-Quan softwares (both ThermoFisher).
Retention times, SRM transitions with corresponding collision energies for the 17 screened NSOs and their ISs are shown in Table 1.
Method validation procedure
Selectivity and carry-over
Drug-free blank hair was analyzed to determine whether endogenous hair constituents interfere or not at the retention times and on the ion channels of NSOs. A replicate of blank sample was also analyzed immediately after the highest calibration standard to determine the carry-over.
Linearity
Six calibration curves were prepared with eight calibration standards ranging from 1 to 1000 pg/mg. Quantification was achieved by plotting the peak area ratios of NSOs to their respective ISs. Back-calculated concentrations of the calibration standards had to be within 85–115% of the nominal concentrations.
Limits of detection and quantification
The limit of detection (LOD) is the lowest concentration for each NSO that can be detected with a signal-to-noise ratio greater than 3. The limit of quantification (LOQ) was the lowest concentration of each NSO achievable with an accuracy of ± 20%.
Accuracy and precision
The accuracy (bias) and precision (coefficient of variation: CV) of the assay were determined at three QC levels (low 5; mid 250; high 750 pg/mg). For the intraday assay, six replicates of each QC were processed on the same day. For the interday assay, six replicates of each QC level were processed at three different days. The concentrations obtained were analyzed using analysis of variance (ANOVA), which separated the intraday and interday standard deviation and the corresponding CVs. An accuracy within the range 85–115% of the nominal values and a precision with a CV of ± 15% were required.
Matrix effect and overall method recovery
Matrix effect was defined as the ratio of the mean peak area obtained by analyzing six different blank hair matrices spiked after extraction with ISs and NSOs at two concentrations (100 and 500 pg/mg) to the mean peak area obtained in an aqueous solution at the same concentrations. Overall method recovery was defined as the ratio of the mean peak area obtained by analyzing six different blank matrices spiked before extraction with ISs and NSOs to the mean peak area obtained in an aqueous solution at the same concentrations. The determination of method recovery remains optional for mass spectrometry techniques.
Application: case report
A 43-year-old man was hospitalized in the emergency department for opioid overdose. Over the week preceding the poisoning, he snorted 70 mg/day of a so-called “China White” powder. After 48 h without any reported consumption, he snorted 3 mg of another powder labeled as “butyrylfentanyl”. Fifteen minutes later, he was found inanimate by his wife who alerted the emergency service. The first examination revealed unconscious state (Glasgow score: 3) and a respiratory depression. The patient also had a bilateral non-reactive tight miosis, cyanosis and bradypnea. He received injection of naloxone before arriving at the emergency department which allowed his recovery. He was discharged from the ICU within 2 days without any toxicological testing and was directed to the addiction clinic to follow a harm reduction program. This patient was a heroin addict and had already experienced different types of drugs, including NPS. Methadone substitution treatment was, therefore, initiated. The powder consumed just before the overdose was subjected to analysis. Two locks of hair were sampled 1 month (M1) (length: 6 cm) and 1 year (Y1) (4 cm) later to monitor his exposure to heroin, NSOs, and other drugs of abuse. Hair samples were cut into 2-cm segments: M1: A 0–2 cm, B 2–4 cm, C 4–6 cm; Y1: A 0–2 cm, B 2–4 cm. The segment A was the closest to the root (proximal) and reflects M1, the overdose time-frame. Each segment reflects a 2-month exposure period based on average hair growth rate of 1 cm/month [18]. Both hair samples were analyzed by the present LC─MS/MS method and by a previously published LC─HRMS method which used the mzCloud shared database containing 81 fentanyl analogs and several non-fentanyl NSOs (e.g., U-47700, U-49900, MT-45, etc.) by 27th June 2019 [15].
Results and discussion
Validation results for the analytical method
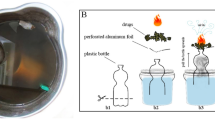
The SRM chromatograms for NSOs obtained in patient’s hair are shown in Fig. 1. The method exhibited a good linearity (determination coefficient, r2 > 0.995) with no interference from endogenous substances for detection of the analytes and ISs. The validation settings of the 6 detected NSOs are summarized in Table 2. Contamination by carry-over from a 1000 pg/mg QC to blank sample was not observed. The LODs and LOQs were 0.3 and 1 pg/mg for fentanyl, acetylfentanyl, and methoxyacetylfentanyl, and 0.8 and 2.5 pg/mg for 3-fluorofentanyl, carfentanil and furanylfentanyl, respectively. The CVs at the LOQs were ≤ 14.7% for all compounds. Intra- and interday accuracy and precision were ≤ 8 and ≤ 14.7%, respectively. Recoveries ranged from 74 to 116% and matrix effect from 20 to 69%.
Analytical results for hair segment 5 months before and up to 1 month after the overdose
The analysis of the first lock of hair showed no exposure to butyrylfentanyl nor the presence of its main metabolite butyryl norfentanyl (LOD= 0.3 and 5 pg/mg, respectively, details not shown) during the last 6 months prior to sampling. This finding was consistent with the analysis of the recovered powder that contained 3-fluorofentanyl (purity 86%) rather than butyrylfentanyl. Segmental analysis demonstrated a repetitive exposure to 3-fluorofentanyl, confirming long-term use of this fentanyl analog by the patient (Table 3). In addition, slightly higher concentration of 3-fluorofentanyl in segment A with respect to segments B and C could be compatible with increased consumption before the overdose, or a consumption of high-purity product leading to patient’s poisoning. These findings clearly demonstrated discrepancy that might exist between the product purchased as “butyrylfentanyl” on the Internet and the one actually delivered to the user. As the toxicity of delivered fentanyl analog might be much higher than the ordered ones, the consumption of the same dose can increase the risk of life-threatening overdose. This phenomenon is recurring and causing mass poisonings and even deaths [28,29,30,31]. Moreover, fentanyl analogs are sold as heroin or are adulterating heroin, other illicit opioids, or even pain relievers. Occasionally, they have also been used to make fake medicines and, less commonly, sold as cocaine [4].
Basic toxicological data regarding 3(meta)-fluorofentanyl are missing from the literature. Comparatively, 4 (para)-fluorofentanyl, one of the isomers has been scheduled as narcotic since 1989 under the United Nation’s single convention on narcotic drugs of 1961 due to its toxicity and abuse potential. According to the Expert Committee on Drug Dependence (ECDD) of the World Health Organisation (WHO) who assessed multiple fentanyl derivatives in 1989, the potency of 4-fluorofentanyl is on a par with fentanyl [32]. Since 2016, 2 (ortho)-fluorofentanyl, another isomer of 3-fluorofentanyl was directly implicated in 16 fatalities in the US and two in Europe (Sweden and Norway). Consequently, it has been scheduled as narcotic (schedule I) in 2017 in the US and by the end of 2018 in Europe [33, 34]. Given the structural similarity among 3-fluorofentanyl, its two isomers and fentanyl itself, it is expected that 3-fluorofentanyl has high potency, dependence and abuse liability similar to that of fentanyl. Thus, the switch from butyrylfentanyl to 3-fluorofentanyl in our patient seemed to significantly contribute to his poisoning as the few available preclinical studies suggested that butyrylfentanyl was about 30 times less potent than fentanyl itself [35]. The analysis of the second strand of hair 1 year later still showed an exposure to 3-fluorofentanyl in this patient but with about sixfold decrease with regard to the concentration initially observed (from 150 to 25 pg/mg). This finding might reflect a decrease in consumption due to its involvement in the precedent overdose or a consumption of a low-purity product.
The consumption of the so-called “China White” powder over a week prior to the poisoning could also have contributed to the opioid adverse effects, as the term “China White” was originally used to describe a highly refined and light-colored form of Southeast Asian heroin, but has also been used in contradictory ways to fentanyls (especially furanylfentanyl) sold as heroin since the 1980s of the last century [5]. This powder could correspond to heroin, furanylfentanyl, fentanyl or a mixture of these compounds as they were all found in patient’s hair, with higher concentrations in segment A of M1 reflecting the overdose time-frame. The presence of and/or interaction with all these analogs may account for some of the reported effects.
Analytical results for hair segments reflecting 9–12 months after the overdose
Furanylfentanyl and fentanyl were also found in the patient’s hair, in much higher concentrations in the second strand (Y1), confirming long-term and polydrug abuse status of this patient, especially for fentanyls. In a recent study from a high-risk population of nightclub and festival attendees from the US, Salomone et al. [26] reported two positive hair samples for fentanyl at 2 and 6 pg/mg, and one for furanylfentanyl at 44 pg/mg out of 34 tested samples. Low rate of incorporation into the keratin matrix or the exposure to low quantities of the drug was suggested by the author. From the present case study, it seems that Salamone’s findings would probably reflect occasional exposure to fentanyl and furanylfentanyl rather than low rate of incorporation into the keratin matrix because the concentrations in the second hair analysis clearly demonstrated high rate of incorporation of the two compounds into the hair. Moreover, Busardò et al. [27] have also reported high concentrations of fentanyl in hair (mean 2670 ± 184 pg/mg, n=2), confirming our findings.
The second hair analysis clearly revealed changes in fentanyl consumption by the patient over the year following his overdose because methoxyacetylfentanyl, carfentanil and acetylfentanyl appeared in the two segments of hair (Y1). The high concentrations of methoxyacetylfentanyl seemed to reflect repetitive exposure. Methoxyacetylfentanyl was first notified in late 2016 and then risk assessed by the EMCDDA and Europol by the end of 2017 due to relevant evidence of serious intoxications or fatalities. Two acute intoxications including one fatal outcome with confirmed exposure to methoxyacetylfentanyl were reported from users who bought products on the Internet supposed to be carfentanil or ketamine, respectively. Overall, at least 28 deaths were reported across Europe and the United States during 2017, largely in a home environment, which showed that in at least some of these cases the poisoning was so severe that the poisoned persons were unable to call for help [36]. Methoxyacetyl norfentanyl, a metabolite of methoxyacetylfentanyl was not screened in our method, but as reported by Busardò et al. [27], this metabolite is not a suitable biomarker of methoxyacetylfentanyl consumption, and was not detected when methoxyacetylfentanyl was taken, whether in blood or urine.
Acetylfentanyl and carfentanil were also found in patient’s hair at very low concentrations. These concentrations probably reflect a single or few exposures, but because hair testing gives evidence of the cumulated incorporation of substances over time, it is difficult to speculate if these fentanyl analogs were taken alone or simultaneously, and if these analogs were present as an impurity of methoxyacetylfentanyl, furanylfentanyl or fentanyl [37]. As expected, respective metabolites of acetylfentanyl (acetyl norfentanyl) and carfentanil (norcarfentanil) were not detected (LOD = 1.5 pg/mg for norcarfentanil and 3 pg/mg for acetyl norfentanyl; detailed data not shown) as the concentrations of parent drugs were very low in our case. In a previous study investigating exposure to fentanyl analogs through hair testing in 40 individuals in inpatient detoxification, Palamar et al. [37] have reported acetylfentanyl hair concentrations ranging from 2.1 to 3200 pg/mg (median: 26 pg/mg) showing that this fentanyl analog integrates well into the hair matrix. In a case of carfentanil related fatality, hair concentrations found in victim’s hair ranged from 54 to 166 pg/mg, which probably reflected a repeated exposure to this fentanyl analog over the studied period of 9 months [38], but could also be due to contamination by sebum and postmortem fluids [39].
In the present case, the patient had probably unknowingly been exposed to methoxyacetylfentanyl, acetylfentanyl and carfentanil, because he claimed in different harm reduction sessions not consuming these analogs. This could come from mislabeling or adulterating with other fentanyl analog(s) that the patient used to order. In Palamar’s previous study [37], 39 out of 40 individuals (98%) tested positive for fentanyl and 85% of participants tested positive for one or more fentanyl analogs, suggesting that exposure to more than one analog is common; 71.8% of the patients denied known use of these compounds [37].
Metabolites of fentanyls
Furanyl norfentanyl and norfentanyl, the respective metabolites of furanylfentanyl and fentanyl were not detected by the method described in Table 1 in the two analyzed samples (LODs = 1.5 and 15 pg/mg, respectively). Even if the LOD for norfentanyl was quite high in our method, our findings were consistent with previously published data. The mean parent- to- metabolite ratio for fentanyl/norfentanyl in Busardò’s study was 32.5. Given that fentanyl concentrations in our case were low in M1, it is not surprising that norfentanyl was not detected. Moreover, previous studies showed that furanyl norfentanyl concentrations were much lower than that of furanylfentanyl, which does not make it a suitable biomarker of furanylfentanyl consumption [40]. Overall, as most metabolites are more hydrophilic than the parent drug, they are less likely to be integrated into the hair matrix.
In addition, the untargeted screening by LC–HRMS allowed the detection of 4-ANPP (4-anilino-N-phenethyl-piperidine) in the two samples (detailed data not shown). 4-ANPP is both a precursor and a metabolite of several fentanyl analogs. It is a major metabolite of fentanyl [27], furanylfentanyl [41], methoxyacetylfentanyl [42] and a minor metabolite of acetylfentanyl [41]. However, in previous studies, reported 4-ANPP hair concentrations were lower than those of parent drugs, making it an inefficient and nonspecific marker of consumption [27]. Unfortunately, the quantification of this compound had not been performed in our study to confirm these findings, because the reference standard was not available in our laboratory.
Conclusions
As shown in a recent study in Canada, 75% of individuals reporting nonmedical opioid use and denying fentanyl use had their urine test positive for fentanyl [43]. Another study showed that, among patients denying known exposure to fentanyl and seeking opioid withdrawal management, two-thirds tested positive for fentanyl in urine [44]. Segmental hair analysis is especially useful for identification and monitoring the use of designer drugs, which often are different from ones that they bought; it enables to follow for months to nearly a year as we did. However, the number of cases for NSO identification and/or quantification using hair samples is still not many [45].
More data are needed to know to what extent the hair analysis can be effective in harm reduction. A large-scale adoption of this approach would allow a better understanding and response to NSO crisis at both health and regulatory levels. To our knowledge, this is the first report to describe the quantification of 3-fluorofentanyl and methoxyacetylfentanyl in hair samples collected from an authentic abuser.
References
National Institute on Drug Abuse (2019) Overdose death rates. https://www.drugabuse.gov/related-topics/trends-statistics/overdose-death-rates. Accessed 4 Jun 2019
Scholl L (2019) Drug and opioid-involved overdose deaths—United States, 2013–2017. MMWR Morb Mortal Wkly Rep. https://doi.org/10.15585/mmwr.mm6751521e1
EMCDDA (2019) European drug report 2019: trends and developments. https://www.emcdda.europa.eu/publications/edr/trends-developments/2019. Accessed 20 Jun 2019
Evans-Brown M, Gallegos A, Christie R (2018) Fentanyl analogs and synthetic cannabinoids: driving greater complexity into the drug situation; an update from the EU Early Warning System. Publ Off Eur Union Luxemb. https://doi.org/10.2810/603753
Ciccarone D, Ondocsin J, Mars SG (2017) Heroin uncertainties: exploring users’ perceptions of fentanyl-adulterated and -substituted ‘heroin’. Int J Drug Policy 46:146–155. https://doi.org/10.1016/j.drugpo.2017.06.004
Armenian P, Vo KT, Barr-Walker J, Lynch KL (2017) Fentanyl, fentanyl analogs and novel synthetic opioids: a comprehensive review. Neuropharmacology 134:121–132. https://doi.org/10.1016/j.neuropharm.2017.10.016
Roda G, Faggiani F, Bolchi C, Pallavicini M, Dei Cas M (2019) Ten years of fentanyl-like drugs: a technical-analytical review. Anal Sci 35:479–491. https://doi.org/10.2116/analsci.18R004
Marchei E, Pacifici R, Mannocchi G, Marinelli E, Busardò FP, Pichini S (2018) New synthetic opioids in biological and non-biological matrices: a review of current analytical methods. Trends Analyt Chem 102:1–15. https://doi.org/10.1016/j.trac.2018.01.007
Sofalvi S, Schueler HE, Lavins ES, Kaspar CK, Brooker IT, Mazzola CD, Dolinak D, Gilson TP, Perch S (2017) An LC-MS-MS method for the analysis of carfentanil, 3-methylfentanyl, 2-furanyl fentanyl, acetyl fentanyl, fentanyl and norfentanyl in postmortem and impaired-driving cases. J Anal Toxicol 41:473–483. https://doi.org/10.1093/jat/bkx052(open access article)
Fogarty MF, Papsun DM, Logan BK (2018) Analysis of fentanyl and 18 novel fentanyl analogs and metabolites by LC–MS–MS, and report of fatalities associated with methoxyacetylfentanyl and cyclopropylfentanyl. J Anal Toxicol 42:592–604. https://doi.org/10.1093/jat/bky035
Qin N, Xiang P, Shen B, Zhuo X, Shi Y, Song F (2019) Application of a validated UHPLC-MS/MS method for 28 fentanyl-analogue and novel synthetic opioids in whole blood in authentic forensic cases. J Chromatogr B 1124:82–99. https://doi.org/10.1016/j.jchromb.2019.05.025
Allibe N, Fouilhe Sam-Lai NF, Willeman T, Jourdil J-F, Bartoli M, Mallaret M, Nemoz B, Stanke-Labesque F, Eysseric-Guerin H (2019) Norcarfentanil: carfentanil misuse or remifentanil treatment? Forensic Toxicol 37:488–495. https://doi.org/10.1007/s11419-019-00481-2
Maurer HH, Meyer MR (2016) High-resolution mass spectrometry in toxicology: current status and future perspectives. Arch Toxicol 90:2161–2172. https://doi.org/10.1007/s00204-016-1764-1
Pleil JD, Isaacs KK (2016) High-resolution mass spectrometry: basic principles for using exact mass and mass defect for discovery analysis of organic molecules in blood, breath, urine and environmental media. J Breath Res 10:012001. https://doi.org/10.1088/1752-7155/10/1/012001(open access article)
Fabresse N, Larabi IA, Stratton T, Mistrik R, Pfau G, Lorin de la Grandmaison G, Etting I, Grassin Delyle S, Alvarez J-C (2019) Development of a sensitive untargeted liquid chromatography–high resolution mass spectrometry screening devoted to hair analysis through a shared MS2 spectra database: a step towards early detection of new psychoactive substances. Drug Test Anal 11:697–708. https://doi.org/10.1002/dta.2535
Karolak S, Nefau T, Bailly E, Solgadi A, Levi Y (2010) Estimation of illicit drugs consumption by wastewater analysis in Paris area (France). Forensic Sci Int 200:153–160. https://doi.org/10.1016/j.forsciint.2010.04.007
Néfau T, Charpentier E, Elyasmino N, Duplessy-Garson C, Levi Y, Karolak S (2015) Drug analysis of residual content of used syringes: a new approach for improving knowledge of injected drugs and drug user practices. Int J Drug Policy 26:412–419. https://doi.org/10.1016/j.drugpo.2014.09.010
Kintz P (2015) Hair analysis in clinical and forensic toxicology, 1st edn. Elsevier, Boston
Kintz P (2017) Hair analysis in forensic toxicology: an updated review with a special focus on pitfalls. Curr Pharm Des 23:5480–5486. https://doi.org/10.2174/1381612823666170929155628
Tsanaclis L, Wicks JF (2007) Patterns in drug use in the United Kingdom as revealed through analysis of hair in a large population sample. Forensic Sci Int 170:121–128. https://doi.org/10.1016/j.forsciint.2007.03.033
Rust KY, Baumgartner MR, Dally AM, Kraemer T (2012) Prevalence of new psychoactive substances: a retrospective study in hair. Drug Test Anal 4:402–408. https://doi.org/10.1002/dta.1338
Tang MHY, Ching CK, Tse ML, Ng C, Lee C, Chong YK, Wong W, Mak TWL (2015) Surveillance of emerging drugs of abuse in Hong Kong: validation of an analytical tool. Hong Kong Med J 21:114–123. https://doi.org/10.12809/hkmj144398(open access article)
Adamowicz P, Gieroń J, Gil D, Lechowicz W, Skulska A, Tokarczyk B (2016) The prevalence of new psychoactive substances in biological material—a three-year review of casework in Poland. Drug Test Anal 8:63–70. https://doi.org/10.1002/dta.1924
Larabi IA, Fabresse N, Etting I, Nadour L, Pfau G, Raphalen JH, Philippe P, Edel Y, Alvarez JC (2019) Prevalence of new psychoactive substances (NPS) and conventional drugs of abuse (DOA) in high risk populations from Paris (France) and its suburbs. A cross sectional study by hair testing (2012–2017). Drug Alcohol Depend. https://doi.org/10.1016/j.drugalcdep.2019.06.011
Salomone A, Gazzilli G, Di Corcia D, Gerace E, Vincenti M (2016) Determination of cathinones and other stimulant, psychedelic, and dissociative designer drugs in real hair samples. Anal Bioanal Chem 408:2035–2042. https://doi.org/10.1007/s00216-015-9247-4
Salomone A, Palamar JJ, Bigiarini R, Gerace E, Di Corcia D, Vincenti M (2019) Detection of fentanyl analogs and synthetic opioids in real hair samples. J Anal Toxicol 43:259–265. https://doi.org/10.1093/jat/bky093
Busardò FP, Carlier J, Giorgetti R, Tagliabracci A, Pacifici R, Gottardi M, Pichini S (2019) Ultra-high-performance liquid chromatography-tandem mass spectrometry assay for quantifying fentanyl and 22 analogs and metabolites in whole blood, urine, and hair. Front Chem 7:184. https://doi.org/10.3389/fchem.2019.00184(open access article)
Arens AM, van Wijk XMR, Vo KT, Lynch KL, Wu AHB, Smollin CG (2016) Adverse effects from counterfeit alprazolam tablets. JAMA Intern Med 176:1554–1555. https://doi.org/10.1001/jamainternmed.2016.4306
Klar SA, Brodkin E, Gibson E, Padhi S, Predy C, Green C, Lee V (2016) Notes from the field: furanyl-fentanyl overdose events caused by smoking contaminated crack cocaine—British Columbia, Canada, July 15–18, 2016. MMWR Morb Mortal Wkly Rep 65:1015–1016. https://doi.org/10.15585/mmwr.mm6537a6
Sutter ME, Gerona RR, Davis MT, Roche BM, Colby DK, Chenoweth JA, Adams AJ, Owen KP, Ford JB, Black HB, Albertson TE (2017) Fatal fentanyl: one pill can kill. Acad Emerg Med 24:106–113. https://doi.org/10.1111/acem.13034
Tomassoni AJ, Hawk KF, Jubanyik K, Nogee DP, Durant T, Lynch KL, Patel R, Dinh D, Ulrich A, D'Onofrio G (2017) Multiple fentanyl overdoses—New Haven, Connecticut, June 23, 2016. MMWR Morb Mortal Wkly Rep 66:107–111. https://doi.org/10.15585/mm6604a4
WHO Expert Committee on Drug Dependence (1989) WHO Expert Committee on Drug Dependence: twenty-sixth report. World Health Organization, Geneva. https://apps.who.int/iris/handle/10665/41542
WHO Expert Committee on Drug Dependence (2018) Critical review report: orthofluorofentanyl. https://www.who.int/medicines/access/controlled-substances/Orthofluorofentanyl.pdf?ua=1. Accessed 2 Aug 2019
Helland A, Brede WR, Michelsen LS, Gundersen POM, Aarset H, Skjølås JE, Slørdal L (2017) Two hospitalizations and one death after exposure to ortho-fluorofentanyl. J Anal Toxicol 41:708–709. https://doi.org/10.1093/jat/bkx050
WHO Expert Committee on Drug Dependence (2016) Critical review report: butyrfentanyl. https://www.who.int/medicines/access/controlled-substances/4.2_Butyrfentanyl_CritReview.pdf. Accessed 2 Aug 2019
EMCDDA (2018) Methoxyacetylfentanyl: risk assessments. https://doi.org/10.2810/520464
Palamar JJ, Salomone A, Bigiarini R, Vincenti M, Acosta P, Tofighi B (2019) Testing hair for fentanyl exposure: a method to inform harm reduction behavior among individuals who use heroin. Am J Drug Alcohol Abuse 45:90–96. https://doi.org/10.1080/00952990.2018.1550652
Gaulier J-M, Richeval C, Phanithavong M, Brault S, Allorge D, Dumestre-Toulet V (2019) A case report of carfentanil-related fatality in France. Toxicol Anal Clin. https://doi.org/10.1016/j.toxac.2019.01.002
Kintz P (2018) Hair analysis in forensic toxicology. WIREs Forensic Sci 1:e1196. https://doi.org/10.1002/wfs2.1196(open access article)
Goggin MM, Nguyen A, Janis GC (2017) Identification of unique metabolites of the designer opioid furanyl fentanyl. J Anal Toxicol 41:367–375. https://doi.org/10.1093/jat/bkx022
Watanabe S, Vikingsson S, Roman M, Green H, Kronstrand R, Wohlfarth A (2017) In vitro and in vivo metabolite identification studies for the new synthetic opioids acetylfentanyl, acrylfentanyl, furanylfentanyl, and 4-fluoro-isobutyrylfentanyl. AAPS J 19:1102–1122. https://doi.org/10.1208/s12248-017-0070-z
Mardal M, Johansen SS, Davidsen AB, Telving R, Jornil JR, Dalsgaard PW, Hasselstrøm JB, Øiestad ÅM, Linnet K, Andreasen MF (2018) Postmortem analysis of three methoxyacetylfentanyl-related deaths in Denmark and in vitro metabolite profiling in pooled human hepatocytes. Forensic Sci Int 290:310–317. https://doi.org/10.1016/j.forsciint.2018.07.020
Jones AA, Jang K, Panenka WJ, Barr AM, MacEwan GW, Thornton AE, Honer WG (2018) Rapid change in fentanyl prevalence in a community-based, high-risk sample. JAMA Psychiatry 75:298–300. https://doi.org/10.1001/jamapsychiatry.2017.4432
Kenney SR, Anderson BJ, Conti MT, Bailey GL, Stein MD (2018) Expected and actual fentanyl exposure among persons seeking opioid withdrawal management. J Subst Abuse Treat 86:65–69. https://doi.org/10.1016/j.jsat.2018.01.005
Tabarra I, Soares S, Rosado T, Gonçalves J, Luís Â, Malaca S, Barroso M, Keller T, Restolho J, Gallardo E (2019) Novel synthetic opioids - toxicological aspects and analysis. Forensic Sci Res 4:111–140. https://doi.org/10.1080/20961790.2019.1588933(open access article)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There are no financial or other relations that could lead to a conflict of interest.
Ethical approval
The analyses of toxic substances were requested by judicial authorities. About several tens of strands of scalp hair (length: 6 and 4 cm) were noninvasively collected from the patient with his informed consent.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Larabi, I.A., Martin, M., Fabresse, N. et al. Hair testing for 3-fluorofentanyl, furanylfentanyl, methoxyacetylfentanyl, carfentanil, acetylfentanyl and fentanyl by LC–MS/MS after unintentional overdose. Forensic Toxicol 38, 277–286 (2020). https://doi.org/10.1007/s11419-019-00502-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11419-019-00502-0