Abstract
Purpose
An inter-method variation experiment to evaluate visible spectrophotometric methods for determining carboxyhemoglobin (CO-Hb) in blood was performed in 17 different forensic science laboratories.
Methods
Three reference samples were prepared and the actual percentages of CO-Hb (%CO-Hb) in reference samples were determined with gas chromatography. The %CO-Hb values in reference samples were measured via four procedures: (1) the “Standard method of chemical analysis in poisoning 2017” (edited by the Pharmaceutical Society of Japan), (2) the isosbestic point method (developed by the Department of Forensic Medicine, Kagawa University), (3) the alkaline condition method, and (4) ISO 27368 with a slight modification.
Results
Procedures (1) and (2) gave results approximately the same as the actual values in low-%CO-Hb samples, but both methods underestimated %CO-Hb levels in blood samples with high %CO-Hb. Using a formula reported by Katsumata et al., procedure (3) overestimated %CO-Hb levels in blood samples with low %CO-Hb, while using the modified formula, gave underestimates in all samples. Procedure (4) gave %CO-Hb values relatively close to the actual values. Thus, an accuracy evaluation test was performed for this procedure and the values obtained were close to the actual CO-Hb content levels.
Conclusions
Procedure (4) was considered sufficiently accurate and thus recommendable for use in forensic science laboratories.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Many poisoning accidents caused by carbon monoxide (CO) have occurred in Japan, and a total of 2008 accidents were reported to the National Research Institute of Police Science (NRIPS) in 2016 [1]. Charcoal burning was frequently used as a means of suicide in the 2000s [2], and the highest number of CO poisoning cases since the first annual report (in 1957) reached 4963 in 2005 [3]. Although CO poisoning accidents have decreased recently, the relative number of CO poisoning cases is still much higher than those of other toxic compounds. Thus, it is very important to examine CO poisoning cases in forensic science laboratories.
CO poisoning is caused by an abrupt increase in blood carboxyhemoglobin (CO-Hb) produced by CO bound to hemoglobin. The degree of CO poisoning is related to the CO-Hb concentration in blood [4, 5]. Hence, the relative concentration of CO-Hb to whole hemoglobin (CO-Hb saturation; %CO-Hb) is measured to estimate the degree of CO toxicosis. Many spectrophotometric methods have been reported for measuring %CO-Hb, including measurements of absorption at the Soret band [6, 7], measurements of absorption at the α and β bands in the presence of a reducing agent [8,9,10,11,12], and the use of commercially available oximeters [13, 14]. Currently, methods based on measuring the difference in the visible spectrum (α and β band) between Hb and CO-Hb in the presence of a reducing agent are mainly used in forensic science laboratories in Japan.
Several different procedures for this visible spectrophotometric method based on α and β bands have been reported to date. These procedures differ in parameters such as wavelength, composition of the reaction mixture, and calculation formula. We have reported the results of a comparison of several procedures previously reported in Japan [15]. These experiments were performed as inter-laboratory proficiency tests in consideration of proposing an universal procedure independent of laboratory skill level. As a result, these procedures gave different values for %CO-Hb, but we could not estimate their accuracy, because we could not determine in advance the exact %CO-Hb values of the test blood samples used in the study. Thus, we considered that an evaluation of the procedures with reference to the %CO-Hb values obtained from a gas chromatography (GC) method [16] was required. An inter-method variation experiment to evaluate the four procedures was performed to assess their accuracy in 16 forensic science laboratories using three blood samples with different %CO-Hb values determined by GC. An accuracy evaluation test was then performed in 17 forensic science laboratories against the most suitable procedure selected through the inter-method variation experiment.
Materials and methods
Materials
Intravenous blood samples were drawn from 10 healthy volunteers (9 men and 1 woman, including 1 smoker and 9 nonsmokers) at the NRIPS into tubes containing ethylenediaminetetraacetic acid as an anticoagulant. The volunteers were in their 50s (n = 3), 40s (n = 2), 30s (n = 3), and 20s (n = 2).
Standard CO gas and oxygen gas (both 99.9% purity) were purchased from GL Sciences (Tokyo, Japan). Sodium dithionite (practical grade), purchased from Wako Pure Chemical Industries, Ltd. (Osaka, Japan), was subdivided into small tubes and tightly stoppered until use. This reagent was sent to each laboratory for use in the tests. Potassium hexacyanoferrate (III), potassium dihydrogenphosphate, potassium cyanide, sodium carbonate anhydrate, and sodium hydroxide (all guaranteed reagents) were purchased from Wako Pure Chemical Industries, Ltd. Saponin (1st grade) was purchased from Kanto Chemical (Tokyo, Japan).
Preparation of test samples
In the inter-method variation experiment, test samples for evaluating the procedures were prepared as follows. The blood samples from donors were pooled and 10 mL of CO gas was gently bubbled into 25 mL of the pooled sample 9 times. This blood sample and the residual pooled blood sample were mixed at the following ratios: sample A, 4:25; sample B, 11:17; and sample C, 1:0. The %CO-Hb values of these three samples were determined using GC as described in the section “Determination of %CO-Hb by GC” below. Because the blood samples from nonsmoking donors were regarded as containing almost 0% CO-Hb, the blood from only nonsmokers was pooled to prepare “sample O” as described in the section “Spectrophotometric procedure for the determination of %CO-Hb in a blood sample” below. These four samples were immediately frozen at −30 °C after preparation and sent to each laboratory under refrigeration.
The test samples for the accuracy evaluation test were prepared as follows. CO gas (40 mL) was introduced into 7 mL of the pooled blood. This blood sample and the blank pooled blood sample were mixed at the following ratios: sample L (low), 1:11; sample M (medium), 1:2; sample H (high), 4:1.
The test samples were prepared at the NRIPS.
Determination of %CO-Hb by GC
CO analysis was performed by GC with barrier discharge ionization detection [16]. Determination of CO in the blood samples was performed using the method of Seto et al. [17] with slight modification. Blood samples (0.1 mL) were added into screw-cap septum vials (9.0 mL, GL Sciences) with the same volume of 20% (w/v) potassium hexacyanoferrate (III) containing 5% (w/v) saponin, and 0.8 mL of distilled water to adjust the total volume to 1.0 mL. Vials were immediately sealed, capped tightly, and incubated for 90 min at 30 °C. Next, 0.1 mL of gas from the headspace in the vial was injected by using a gas-tight syringe into a gas chromatograph (Shimadzu Tracera; Shimadzu Corporation, Kyoto, Japan) with a molecular sieve 5A mega-bore capillary column (30 m × 0.53 mm, film thickness 50 μm; Restek, Bellefonte, PA, USA). The carrier gas was helium (flow rate: 4.4 mL/min). The injector temperature was 250 °C, and the samples were injected in the split injection mode (split ratio 1:7). The column oven temperature was held at 100 °C and the detector temperature was 280 °C.
The %CO-Hb was calculated from the CO concentration in the headspace (8.0 mL) and the concentration of heme in the blood samples [16]. Heme in the blood sample was determined via the cyanmethemoglobin method [12, 18]. Potassium hexacyanoferrate (III) (25 mg), potassium dihydrogenphosphate (3.5 mg), and potassium cyanide (1.25 mg) were added to diluting reagent (25.0 mL), and 0.1 mL of a blood sample was added. After 15 min, A540 was measured and the heme concentration was calculated based on ε540 (11.0 mM−1 cm−1) [19]. All measurements were performed in triplicate.
Spectrophotometric procedure for the determination of %CO-Hb in a blood sample
We evaluated four procedures for the determination of %CO-Hb as described below. Because two different formulae were proposed for procedure (3), the analysts used both formulae and submitted both sets of results.
-
1.
Procedure described in the “Standard Method of Chemical Analysis in Poisoning 2017” (edited by the Pharmaceutical Society of Japan) [12]
-
(i)
Sample O was diluted 200-fold with 0.1% (w/v) Na2CO3.
-
(ii)
Sodium dithionite (5 mg) was added to 5 mL of the diluted sample O solution.
-
(iii)
After 15 min, absorbances at 538 nm (A538) and 555 nm (A555) were measured and the A538/A555 value (A0) was calculated.
-
(iv)
CO gas (5 mL) was introduced into this solution.
-
(v)
A538 and A555 were measured and the A538/A555 value (A100) was calculated.
-
(vi)
Samples A, B, and C were diluted 200-fold with 0.1% (w/v) Na2CO3.
-
(vii)
Sodium dithionite (5 mg) was added to 5 mL of each diluted solution.
-
(viii)
A538 and A555 were measured and the A538/A555 value (Ax) was calculated.
-
(ix)
%CO-Hb was obtained by the formula described below.
$$ \% {\text{CO-Hb}} = \left( {A_{x} - A_{0} } \right)/\left( {A_{100} - A_{0} } \right) \times 100 $$(1)
-
(i)
-
2.
Procedure measuring isosbestic point [15]
-
(i)
Samples A, B, and C were diluted 200-fold with 0.1% (w/v) Na2CO3.
-
(ii)
Sodium dithionite (25 mg) was added to 10 mL of each diluted solution.
-
(iii)
A539 and A579 were measured and the A539/A579 value (Ax) was calculated.
-
(iv)
%CO-Hb was obtained by the formula described below.
$$ \% {\text{CO-Hb}} = 208.5A_{x} - 232.2 $$(2)
-
(i)
-
3.
Procedure under alkaline conditions reported by Katsumata et al. [8]
-
(i)
Sodium dithionite (2 mg) was added to 2.5 mL of 0.1% (w/v) Na2CO3.
-
(ii)
Samples A, B, or C (each 10 μL) and 0.2 mL of 5 M NaOH were added to this solution.
-
(iii)
After 5 min, A532 and A558 were measured and the A558/A532 value (Ax) was calculated.
-
(iv)
%CO-Hb was obtained by the formulae described below.
Katsumata’s formula [8]:
$$ \% {\text{CO-Hb}} = \left( {2.44 - A_{x} } \right) \times 67 $$(3-1)Modified Katsumata’s formula [15]:
$$ \% {\text{CO-Hb}} = \left( {2.30 - A_{x} } \right) \times 75.6 $$(3-2)
-
(i)
-
4.
ISO 27368 procedure [9] with a slight modification
-
(i)
Sample O (15 μL) was diluted with 3 mL of 0.1% (w/v) Na2CO3 and 10 mL of oxygen gas was introduced into this solution by bubbling for 5 min with occasional shaking.
-
(ii)
To this solution, 30 mg of sodium dithionite was added. Immediately, A540 and A579 were measured and the A540/A579 value (A0) was calculated.
-
(iii)
Sample O (15 μL) was diluted with 3 mL of 0.1% (w/v) Na2CO3, and 5 mL of CO gas was introduced into this solution for 1 min.
-
(iv)
To this solution, 30 mg of sodium dithionite was added. A540 and A579 were immediately measured and the A540/A579 value (A100) was calculated.
-
(v)
Samples A, B, and C (each 15 μL) were diluted with 3 mL of 0.1% (w/v) Na2CO3.
-
(vi)
Sodium dithionite (30 mg) was added to this solution.
-
(vii)
A540 and A579 were immediately measured and the A540/A579 value (Ax) was calculated.
-
(viii)
%CO-Hb was obtained by the formula described below.
$$ \% {\text{CO-Hb}} = \left( {A_{x} - A_{0} } \right)/\left( {A_{100} - A_{0} } \right) \times 100 $$(4)
-
(i)
Oxygen gas volume required to provide 0% CO-Hb from control blood
When oxygen gas was introduced into the blood to prepare the 0% CO-Hb sample, the required volume of oxygen gas should depend on the initial CO-Hb percentage of the blood. Thus, we examined the oxygen gas volume required to provide 0% CO-Hb using various blood samples. The respective blood samples (15 μL) were diluted by 3 mL of 0.1% (w/v) Na2CO3. Three blood samples, namely, the smoker’s blood (%CO-Hb ~ 3%), samples M, and sample H, were used in this examination. Various volumes of oxygen gas were bubbled through each diluted blood solution at 2 mL/min. The concentrations of CO-Hb in the oxygen-introduced blood solutions were measured by procedure (4). All assays were performed in triplicate.
Inter-method variation experiment
The inter-method variation experiment for evaluation of the procedures was performed at 16 forensic science laboratories in Japan (Hokkaido Hakodate area Police Headquarter (H.Q.), Aomori, Miyagi, Ibaraki, Gunma, Chiba, Yamanashi, Shizuoka, Toyama, Fukui, Okayama, Yamaguchi, Kagawa, Nagasaki and Kagoshima Prefectural Police H.Q., and the NRIPS). The analysts at each laboratory determined the %CO-Hb of samples A, B, and C using the four procedures described above. All assays were performed in triplicate. The analysts were not informed of the actual %CO-Hb of the test samples.
The spectrophotometers used at each laboratory was as follows: a V-660 UV–visible spectrophotometer (JASCO Corporation, Tokyo, Japan) was used at the NRIPS, a UV-1800 UV–visible spectrophotometer (Shimadzu Corporation, Kyoto, Japan) was used at Miyagi Prefectural Police Headquarters, and V-630 UV–visible spectrophotometers (JASCO Corporation) were used at the other laboratories.
Accuracy evaluation test
The accuracy evaluation test was performed only for procedure (4); it was performed by 17 forensic science laboratories in Japan (16 forensic science laboratories described in “Inter-method variation experiment”, plus Saitama Prefectural Police H.Q.). The analysts of each laboratory also determined the %CO-Hb of samples at the L, M, and H concentrations by procedure (4) described above. All assays were performed in triplicate.
The spectrophotometers used at each laboratory were the same as those described in “Inter-method variation experiment”.
Results
%CO-Hb levels in the test samples determined by GC
The actual %CO-Hb levels of the samples used in this study were measured by GC. The concentrations of CO liberated from 0.1-mL samples were determined. The %CO-Hb levels were calculated from CO concentrations and the concentrations of heme in the blood samples. The %CO-Hb levels of samples O (nonsmokers), A, B, and C were 1.4 ± 0.0, 7.5 ± 0.2, 26.6 ± 1.7, and 77.6 ± 4.1%, respectively. The %CO-Hb levels of samples L, M, and H for the accuracy evaluation tests were 14.4 ± 0.3%, 36.5 ± 3.0%, and 67.3 ± 5.3%, respectively.
Results of the inter-method variation experiment
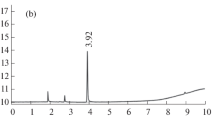
The results of the inter-method variation experiment are shown in Fig. 1. All data reported from the laboratories were plotted in this figure, and crosses indicate mean values. The %CO-Hb levels determined by GC were used as reference values.
Results of carboxyhemoglobin (CO-Hb) measurements of the test samples. All results from 16 laboratories were plotted. Crosses indicate mean values and the dotted line indicates the reference value [obtained by gas chromatography (GC)]. a Sample A; b sample B; c sample C. Details of procedures (1)–(4) and GC were described in the text
Procedures (1) and (2) gave values close to the reference values for samples A and B, but both methods clearly underestimated %CO-Hb for sample C.
Procedure (3-1) (Katsumata’s formula) gave an overestimate for sample A, which had a low concentration of CO-Hb. However, the procedure gave values that were close to the reference values for sample B and underestimates for sample C. The values obtained by procedure (3-2) (modified Katsumata’s formula) were underestimated in all samples.
Procedure (4) gave overestimates for sample A; however, the values derived for samples B and C were almost the same as and slightly lower than the reference values, respectively. Of the four procedures tested in this study, this procedure gave %CO-Hb values that were relatively similar to the actual values.
Taking note of data dispersion, the data points calculated by procedure (4) were most widely spread out. In contrast, the results calculated by procedure (1) showed the least dispersion (Fig. 1).
The %CO-Hb levels measured by spectrophotometric procedure and the reference values (GC) are plotted Fig. 2. If the measured values and reference values are identical, the plotted line should overlap the dotted line in the figures. Procedures (1) and (2) gave nearly correct values in low-CO-Hb samples, but the measured values tended to diverge from the reference values in high-CO-Hb samples. In procedure (3), Katsumata’s formula (3-1) gave overestimates in low-CO-Hb samples, but underestimates in high-CO-Hb samples. On the other hand, the values obtained by the modified Katsumata’s formula (3-2) were underestimated. Procedure (4) gave the values close to the actual values, except for the values of low-CO-Hb samples.
%CO-Hb measured by spectrophotometric procedure versus reference values obtained by GC. The results of procedures (1)–(4) are shown in each panel. In procedure (3), two results are indicated as obtained by Katsumata’s equation (opened circle) and modified Katsumata’s equation (filled circle). The averages of the results from 16 laboratories were plotted and the error bars indicate standard deviations. If a measured value and reference value are identical, the plotted line should overlap the dotted line
To evaluate these procedures, we calculated the square of the difference between the CO-Hb content measured spectrophotometrically and the CO-Hb content determined using GC (Table 1). The values obtained from procedure (4) were more accurate than those obtained by the other procedures.
Oxygen gas volume required to provide 0% CO-Hb in various blood samples
Figure 3 shows the relationship between the initial CO-Hb concentration and the necessary oxygen gas volumes needed to provide 0% CO-Hb. Oxygen gas (80 mL) reduced the CO-Hb concentration from 62 to 3%, but could not eliminate it completely. In the 38% CO-Hb sample, 45 mL of oxygen gas was not enough to eliminate CO-Hb completely. However, 3% CO-Hb was reduced to 0.1% by 10 mL of oxygen gas. This result showed that it is difficult to prepare nearly 0% CO-Hb from a high percentage CO-Hb blood sample. If the initial %CO-Hb of blood sample was lower than 3%, a nearly 0% CO-Hb sample could be obtained by introducing oxygen gas.
Results of accuracy evaluation test
Because the values obtained by procedure (4) were more accurate than those obtained by the other procedures, we attempted to perform the test again to confirm the accuracy. The results of the accuracy evaluation test are shown in Fig. 4 and Table 2. Values close to the actual CO-Hb content levels were obtained by procedure (4) in the second test (accuracy evaluation test). Compared with the result of the first test (inter-method variation experiment), the accuracy and deviation were improved in the second test. To evaluate this procedure, we calculated the square of the difference between the CO-Hb content measured spectrophotometrically and the CO-Hb content determined using GC.
Result of the accuracy evaluation test of procedure (4). Measured %CO-Hb values are plotted against actual %CO-Hb values obtained by GC. The averages of the results from 17 laboratories were plotted, and the error bars indicate standard deviation
Discussion
Procedures (1) and (4) calculated the %CO-Hb levels based on positive (100% CO-Hb) and negative (0% CO-Hb) control values. In procedure (1), blood taken from nonsmokers was used as a negative control. Because the blood of nonsmokers has been reported to contain 1.22% [20], 1.5% [21], 1.6% [15], and 2% [5] CO-Hb, the CO-Hb concentration of this negative control sample is not strictly 0%. On the other hand, in procedure (4), oxygen gas was introduced into the negative control sample in order to prepare a 0% CO-Hb sample (Fig. 3). Therefore, we thought that procedure (4) may give more accurate values than procedure (1). In the original procedure of ISO 27368 [9], the test sample was diluted, and the diluted solution was divided to three tubes. Oxygen gas was introduced into one of the three tubes to give 0% CO-Hb, and CO gas was introduced into another tube to provide 100% CO-Hb. The third tube was not treated with any gas before the CO-Hb concentration was measured. In this case, the necessary oxygen gas volume to provide a 0% CO-Hb solution should depend on the initial CO-Hb concentration of the test sample. However, the CO-Hb concentration of a test sample is, of course, unknown. As shown in Fig. 3, we needed a larger volume of oxygen gas to reduce the concentration of CO-Hb in the high-CO-Hb blood to nearly 0%. Furthermore, 10 mL of oxygen gas was enough to reduce a 3% concentration of CO-Hb to 0.1%. Therefore, we considered that the blood of nonsmokers (CO-Hb concentration lower than 2% [5, 15, 20, 21]) was able to be converted to nearly 0% CO-Hb by bubbling of 10 mL of oxygen gas. We recommend preparing 0% and 100% CO-Hb for calibration standards from the blood of a nonsmoker.
Procedure (4) gave %CO-Hb values relatively close to the actual values at first test, but standard deviation (SD) of data obtained was large (Fig. 2). However, the SD became smaller for the second test (Fig. 3). Focusing on the dispersion of the measurement values, A0, A100 and Ax, only A100 value gave remarkable large dispersion flor the first test (data not shown). Because procedure (4) calculates the %CO-Hb levels of unknown sample based on A0 and A100 values, A100 value should affect the %CO-Hb value of an unknown sample. Procedure (4) may be little bit complicated, compared to the other procedures which have been examined frequently in the forensic science laboratories, and has been tried by the laboratories for the first time. So the large dispersion may be due to the untrained operation of this newly examined procedure. The dispersion of A100 value became smaller for the second test; thus, we thought that the SD of %CO-Hb was improved by improved technical operation.
Equations for calculating CO-Hb concentrations are provided below for procedures (2) and (3).
The formula for procedure (2) was introduced from the ratio of optical density of two components at two wavelengths (Eq. 5) [22].
(c, total concentration of two components; c2, concentration of target component; λ1 and λ2, wavelengths for measurements, λ2 is the isosbestic point; ε1 and ε2, extinction coefficient of two components; Aλ1 and Aλ2, absorbance at λ1 and λ2).
When Eq. 5 was applied to measure the ratio of CO-Hb in the blood sample by procedure (2), the wavelengths for the measurements were 539 nm and 579 nm (isosbestic point). The ratio of CO-Hb (c2) to total Hb concentration (c) is indicated by Eq. 6.
(X, A539/A579 of unknown sample; X100% and X0%: A539/A579 of the 100% and 0% CO-Hb sample, respectively).
Thus, a higher-precision measurement of X100% and X0% can give an accurate equation for the calculation of CO-Hb.
On the other hand, Katsumata’s equation (3-1) was introduced as follows [8]. When the percentage of CO-Hb in the blood sample is indicated by the equation Y (%CO-Hb) = (a − A558/A532) × b, the constant a is identical to A558/A532 of 0% CO-Hb. The constant b is easily obtained from A558/A532 of 100% CO-Hb [8]. The constants of modified Katsumata’s equation (3-2) was reset as a result of reexamination. The results in this study indicated that the modified Katsumata’s equation (3-2) was improved to provide greater accuracy, but these values were not still accurate enough. The exact values of A558/A532 for 0 and 100% CO-Hb are needed to introduce the correct equation.
In both procedures (2) and (3), the exact measured values of absorbance for 0% and 100% CO-Hb were necessary to introduce the correct equation. We considered that the preparation of absolute 100% and 0% CO-Hb samples is most important for that purpose. Further improvement of the equations is necessary to obtain measured values sufficiently close to the actual values.
As for the laboratory differences in reported values, a certain tendency was observed (data not shown). The number of the laboratories presenting more than two of three of %CO-Hb values outside of the average ± SD within three concentration samples in the respective procedures were 1, 3, 5, 5 and 3 within 16 laboratories for the procedures (1), (2), (3-1), (3-2), and (4), in the inter-method variation experiment, and 4 within 17 laboratories in the accuracy evaluation test. The different characteristics of the operation techniques and equipment in the laboratories may influence the above tendency, but this tendency was not extreme. Really, there was no laboratory which presented results all outside of the average ± 2SD values in the respective procedures. Therefore, the %CO-Hb values are regarded to be randomly distributed, not depending on the laboratory difference.
Conclusions
Procedure (1), the “Standard Method of Chemical Analysis in Poisoning 2017”, and procedure (2), the “isosbestic point method” (developed by Department of Forensic Medicine, Kagawa University), gave results close to the actual %CO-Hb values from low-%CO-Hb samples, but both of these methods underestimated the %CO-Hb value from high-%CO-Hb blood samples. Procedure (3) using the formula proposed by Katsumata gave overestimates for blood samples with low %CO-Hb, while using modified Katsumata’s formula, underestimated the values in all samples. Procedure (4), ISO 27368 with a slight modification, gave %CO-Hb values relatively close to the actual values. The results of the accuracy evaluation test showed again that procedure (4) gave results closest to the actual values.
References
National Research Institute of Police Science (2017) Annual case report of drug and toxic poisoning in Japan No. 60 (Jan-Dec 2016). National Research Institute of Police Science, Kashiwa (in Japanese)
Yoshioka E, Hanley SJB, Kawanishi Y, Saijo Y (2014) Epidemic of charcoal burning suicide in Japan. Br J Psychiatry 204:274–282
National Research Institute of Police Science (2007) Annual case report of drug and toxic poisoning in Japan No. 49 (Jan-Dec 2005). National Research Institute of Police Science, Kashiwa (in Japanese)
Raub JA, Mathieu-Nolf M, Hampson NB, Thom SR (2000) Carbon monoxide poisoning—a public health perspective. Toxicology 145:1–14
Prockop LD, Chichkova RI (2007) Carbon monoxide intoxication: an updated review. J Neurol Sci 262:122–130
Ishizawa F (1981) A study on the spectrophotometric determination of carboxyhemoglobin in blood—isosbestic point method. Jpn J Legal Med 35:191–200
Rodkey FL, Hill TA, Pitts LL, Robertson RF (1979) Spectrophotometric measurement of carboxyhemoglobin and methemoglobin in blood. Clin Chem 25:1388–1393
Katsumata Y, Aoki M, Sato S, Suzuki O, Oya M, Yada S (1982) A simple spectrophotometry for determination of carbonhemoglobin in blood. J Forensic Sci 27:928–934
International Organization for Standardization (2008) ISO27368: analysis of blood for asphyxiant toxicants—carbon monoxide and hydrogen cyanide. International Organization for Standardization, Geneva, pp 14–15
Winek CL, Prex DM (1981) A comparative study of analytical methods to determine postmortem changes in carbon monoxide concentration. Forensic Sci Int 18:181–197
Sakata M, Haga M (1980) Rapid determination of carboxyhemoglobin by absorbance difference between double wave length. Jpn J Toxicol Sci 5:113–121
The Pharmaceutical Society of Japan (2017) Standard method of chemical analysis in poisoning 2017. Tokyo Kagaku Dojin, Tokyo, pp 40–45 (in Japanese)
Tanaka N, Ameno K, Mostofa J, Ohkubo E, Kumihashi M, Kinoshita H (2010) Application of oximeter AVOX 4000 for the determination of CO-Hb in the forensic practice. Res Pract Forensic Med 53:39–43 (in Japanese)
Lee C, Tam JCN, Kung L-K, Yim L (2003) Validity of CO-oximetric determination of carboxyhaemoglobin in putrefying blood and body cavity fluid. Forensic Sci Int 132:153–156
Ohmori T, Kumihashi M, Endo K, Nakazawa H, Takekawa K, Uchikawa T, Seto Y (2018) Comparison of visible spectrophotometric methods for measuring carboxyhemoglobin in blood sample. Jpn J Forensic Sci Technol 23:91–101 (in Japanese with English abstract)
Ohmori T, Otsuka M, Seto Y (2017) Measurement of carbon monoxide in blood sample using gas-chromatography with barrier discharge. Rep Natl Res Inst Police Sci 66:59–64 (in Japanese with English abstract)
Seto Y, Kataoka M, Tsuge K (2001) Stability of blood carbon monoxide and hemoglobin during heating. Forensic Sci Int 121:144–150
Taylor JD, Miller JDM (1965) A source of error in the cyanmetheglobin method of determination of hemoglobin concentration in blood containing carbon monoxide. Am J Clin Pathol 43:265–271
Zettner A (1967) The extinction coefficient of cyanmethemoglobin. Am J Clin Pathol 48:332
Coburn RF, Blakemore WS, Forster RE (1963) Endogenous carbon monoxide production in man. J Clin Invest 42:1172–1178
Stewart RD (1975) The effect of carbon monoxide on humans. Annu Rev Pharmacol 15:409–423
Van Kampen EJ, Zijlstra WG (1966) Determination of hemoglobin and its derivatives. Adv Clin Chem 8:141–187
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Because the coauthor Yasuo Seto of this manuscript is one of the Chief Editors of this journal and has been assigned as the handling editor of this manuscript, another Chief Editor Osamu Suzuki has carefully checked the contents of this manuscript, each process of reviews and decision makings, and has concluded that the paper is sound and does not need further revision. Other (co)authors declare no competing interest.
Ethical approval
Blank intravenous blood samples were drawn from 10 healthy volunteers after obtaining informed consent. This article does not contain any studies with animals performed by any of the authors. All experiments were approved by the Ethical Review Board for Human Sample Experiments at the National Research Institute of Police Science (approval no. 2014004).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Ohmori, T., Saito, Y., Mamiya, K. et al. Comparison of measurement methods for carboxyhemoglobin in blood samples based on visible spectra with 17 institutions. Forensic Toxicol 37, 330–338 (2019). https://doi.org/10.1007/s11419-019-00469-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11419-019-00469-y