Abstract
Early detection of functional decline, a major risk among hospitalized older adults, can facilitate interventions that could significantly reduce it. We aimed to examine the contribution of the Timed Up and Go (TUG) test in predicting Hospitalization Associated Functional Decline (HAFD) among older adults, able to independently ambulate before admission. We used a cross-sectional study design; a total of 310 older adults (age ≥ 65) hospitalized in internal medicine wards between December 2018 and August 2020 were included; exclusion criteria were inability to ambulate, a diagnosis restricting mobility, hospitalization for end-of-life care, or impaired cognition. The Modified Barthel Index was used to assess HAFD; it was administered at admission to evaluate patients’ independence in activities of daily living 2 weeks prior hospitalization, and at discharge. The TUG test was performed on admission and to predict significant functional decline (defined by a reduction of three points or more in the Modified Barthel Index), while accounting for demographics, length of hospitalization, comorbidity burden (Charlson’s comorbidity index), and cognitive function (ALFI-MMSE). Participants were divided into three groups according to their TUG score—under or over a cut-off score of 12 s, or inability to complete the test. Adjusting for age, comorbidity, cognitive ability, and duration of hospitalization, the group that performed the test in less than 12 s showed no statistically significant change in the Modified Barthel Index, therefore no significant HAFD. The other groups showed a statistically significant decline in function. Risk for significant HAFD is currently underestimated in clinical settings, limited to subjective assessment, and underused in the context of implementing early interventions to prevent HAFD. The TUG may support screening for those at risk of hospitalizing-associated functional decline and could help identify patients suitable for preventative interventions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hospitalization Associated Functional Decline (HAFD) in older adults has been recognized as a major phenomenon with significant consequences such as slower recovery, higher rates of nursing home placement, and increased morbidity and mortality [1,2,3,4]. Functional decline, defined as a reduction in functional autonomy and an increase in disability [5], was previously linked with reduced mobility levels among older adults both in community and hospital settings [6, 7]. Moreover, functional decline was found to be associated with risk of falls or a consequence of low mobility abilities [8]. Many factors were previously associated with a risk to develop HAFD, most of which can be divided into personal or environmental factors [9, 10]. However, there is currently no objective test that can directly estimate personal risk for HAFD. Having a simple, easy to administer, objective tool for early identification of individuals at greater risk of functional decline may support implementation of early, hospitalization-specific, mobility programs aiming to reduce older adults’ functional decline during hospital stays [4] or otherwise support proper utilization of hospital resources.
Function can be measured objectively or subjectively [11, 12]. Subjective assessment, such as The Activities of Daily Living Questionnaire [13], is based on a subjective rating of the patient’s ability, while objective assessment of function involves tasks that requires demonstration of the ability to walk, get up from a chair, maintain balance while performing a task, and so on (e.g., Short Physical Performance Battery, 6-min walk) [14], offering a more reliable metric of function [15]. Functional decline can be estimated using different tests or clinical tools [16]; one such tool used in hospital settings is the Barthel Index [1, 4].
The Barthel Index includes 10 items relating to activities of daily living and mobility (e.g., bathing, dressing, chair transfer, stair climbing), rated by level of independence to perform each item [17, 18]. The Barthel Index is commonly performed based on a subjective report by the patient or family members [19]. The total score ranges from 0 to 100, and the minimum clinically important difference changes across cohorts, ranging from 1 to 10 points or more, depending on the reference population [20,21,22]. Among ambulating older adults, a 3 points reduction in the Barthel Index is considered a minimum clinically important difference [21]. Using simple and feasible functional measures, such as the Timed Up and Go (TUG) test, can provide a better assessment for HAFD risk by adding an objective dimension of mobility to currently available predictors [23].
The TUG test, an objective assessment of mobility, is linked with an individual’s functional ability, including lower extremity muscular strength [24], aerobic capacity, and walking endurance [25]. The test, commonly used as a measure of mobility and for risk of falls assessment [26], is comprised by getting up from a chair, walking 3 m, turning, and returning to the starting seated position. The TUG test is extensively used in community-based facilities and is recommended by various geriatric societies both for assessing older adults’ mobility and as a screening tool for risk of falls [27, 28]. The TUG test was also found to be associated with other various impairments in older adults, such as frailty [29], severity of Parkinson’s disease [30], and functional decline [31]. The TUG test is also associated with cognition, as the test procedure requires adequate attention and executive function [32]; thus, it extends our ability to quantify an individual’s ability to participate in activities of daily living.
The TUG test has clear advantages relative to other mobility tests, such as the de Morton Mobility Index [33] and the Acute Care Mobility Assessment [34]: it is objective, takes a short time to complete, and is easy to administer [23]. The parameter of interest in the TUG test is time-to-completion. Different studies have used various TUG test clinical cut-off points, ranging from 13 to 32.6 s [35]. The Centers for Disease Control and Prevention (CDC) Stopping Elderly Accidents, Death and Injuries (STEADI) initiative suggests using a relatively rigorous cut-off point of 12 s to differentiate individuals at risk [36], suggesting that setting a higher performance bar is preferable. Moreover, although inability of hospitalized older adults to complete the TUG test is perceived as a hinderance to its usability, some studies show that this response can also be informative—for example, inability to complete the TUG test was found to be predictive of future falls [37] and of length of hospitalization [38].
Despite its use in community facilities, the TUG test is regarded as an objective measure for risk of fall by most practitioners [39], and thus is not commonly used for assessing functional ability in acute care hospital settings. Re-examining it as a tool for objective assessment of function would be beneficial, as HAFD has been shown to be modifiable through in-hospital interventions [1, 4, 40]. This study suggests expanding the existing model of the TUG test to include three categories (i.e., completion under 12 s, completion 12 s and over, and not being able to complete the test); we aimed to examine the use of the TUG test, with these three objective categories, as a possible screening tool for HAFD risk in older hospitalized patients.
Methods
Setting
This observational longitudinal study is part of the HoPE-MOR (Hospitalization Process Effects on Mobilization Outcomes and Recovery) study, conducted in two internal medical units in two hospitals in northern Israel (Ha’emek Medical Center and Bnei-Zion Medical Center). The study was approved by the ethics committee of the Faculty of Social Welfare and Health Sciences at University of Haifa, Israel (approval no. 324/17) and funded by the Israel Science Foundation (ISF 1216/17).
Participants
Older adults (age ≥ 65 years), who were admitted in one of the two internal medicine units via the adjacent emergency department due to an acute condition or the exacerbation of a chronic condition, were screened for participation in the study. Inclusion criteria were speaking Hebrew, Russian, or Arabic and being able to walk at time of admission. Exclusion criteria were a diagnosis or a condition restricting walking ability (e.g., hip fracture, wheelchair user), hospitalization for end-of-life care, isolation due to resistant bacteria, and impaired cognition (Short Portable Mental Status Questionnaire score ≤ 5 or a score of > 4 in the 4AT Delirium Screening Tool) [41, 42]. Written consent was obtained from all participants prior to any study procedure.
Study procedures
The TUG test was administered within 24 h of admission by research team members who were trained beforehand by one of the authors (a physical therapist) and periodically observed to ensure procedure fidelity. The participants were asked to stand up from a standard height chair (seat height approximately 46 cm, as per TUG test guidelines [43]), walk around a cone positioned at 3 m, and return to the seated position [23]. The test was demonstrated by a study team member prior to measurement and a single training attempt was allowed for familiarity with the test. A study team member remained in proximity to the participant to assure safety, without interfering with the procedure. Time to complete the test was recorded using a stopwatch; failure to complete was also recorded. The TUG test has a good test–retest reliability and excellent test–retest reliability and validity in similar population [44]. Functional decline was assessed using The Modified Barthel Index [45]; this version of the tool was chosen for its ability to detect more subtle changes in ability than the original version [46]. An individual’s subjective assessment for level of independence in 10 activities of daily living was rated, for a total score ranging from 0 (completely dependent) to 100 (completely independent). The tool was administered by research team members who were trained beforehand by one of the authors (a licensed nurse) and periodically observed to ensure procedure fidelity. The Modified Barthel Index administered at admission was used to evaluate patients’ independence in activities of daily living 2 weeks prior to administration. Administration at discharge provided quantification of HAFD. The Barthel Index has a good test–retest reliability and validity as a measure of physical dependency [47].
Demographic data including age, gender, and duration of hospitalization (days) were collected from medical records. The burden of chronic medical diagnosis was assessed using Charlson’s comorbidity index (CCI) [48] and was filled out by the research team within 24 h of admission; CCI refers to 19 health conditions divided into three categories of severity, with scores ranging from 0 to 37. Higher scores indicate higher risk of mortality. Cognitive function was assessed within 24 h of admission using the Adult Lifestyle and Function Interview—Mini-Mental State Examination (ALFI-MMSE) [49], a reliable and validated short version of the MMSE. This tool includes 22 items, with scores from 0 to 22, where lower scores indicate lower cognitive function; a score of 17 points or less in ALFI-MMSE is used to discriminate individuals with impaired cognition.
Statistical analysis
Analyses were performed using either SPSS 27 (IBM SPSS Statistics, New York, US) or Jamovi (v. 2.4.11) [50]. Continuous data were presented as either mean ± SD or mean ± SE, as appropriate, and categorical data were presented as percentage and raw number of individuals. Differences in demographic variables were examined by Welch’s ANOVA with Games-Howell tests for post hoc comparisons, the Kruskal–Wallis with Dwass-Steel-Critchlow-Fligner (DSCF) tests for post hoc comparisons, and Pearson’s chi-squared tests, with post hoc comparisons conducted via adjusted standardized residuals. Games-Howell and DSCF tests control for familywise type I error, and false discovery rate adjustment was used for the post hoc comparisons for Pearson’s chi-squared tests. To estimate exact p-values for Pearson’s chi-squared tests, the Monte Carlo sampling method (200,000 samples) was applied to compute p-values. As Modified Barthel Index scores are count data, a mixed Poisson model was used. The model included random intercepts for participants and hospitals as random variables, to account for random variability.
Results
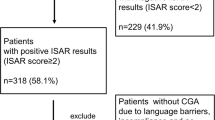
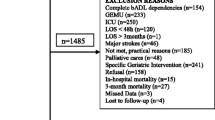
Data collection was initiated in December 2018 and terminated in August 2020; a total of 2615 older adults were admitted to both units, and a total of 310 participants (age 77 ± 7) were recruited to this study. A flow chart with full procedures and reasons for exclusion is provided as supplementary Fig. S1. Included participants were divided into three groups according to their TUG test results, based on the 12 s cut-off point set by the CDC [36] or inability to complete the test altogether. Group 1 included 46 participants scoring TUG < 12 s; group 2 included 165 participants scoring TUG ≥ 12 s, and the remaining 99 participants were included in group 3, being unable to complete the TUG test. Table 1 presents participants’ demographics as well as covariates data; ALFI-MMSE scores (global cognitive function) were significantly different between the groups, with group 1 exhibiting the highest scores. Participants allocated to group 1 were significantly younger than patients from groups 2 and 3. No differences were found between the groups regarding sex and CCI (comorbidity index).
Table 2 presents the cohort descriptive statistics; Tables 3 and 4 present the mixed Poisson model results, comparing the model-adjusted Modified Barthel Index scores at each time point while controlling for selected covariates. Note that while group 1 showed no clinically significant change in Modified Barthel Index scores, the other two groups demonstrate a significant functional decline, shown by ΔBarthel Index of − 4.03 and − 8.79 respectively. Figure 1 presents a visual summary of the main results (note that “greatly reduced” refers to the magnitude of change in ΔBarthel Index).
The full model for the change in Modified Barthel Index score explained 80.17% of the variance [R2conditional; LRT χ2 (13) = 1224.11, p < 0.001], and the fixed factors explained 30.62% of the variance in the full model [R2margianl; LRT χ2 (9) = 131.39, p < 0.001]. The Group * Time interaction was statistically significant [χ2 (2) = 14.45, p < 0.001], and post hoc testing revealed that groups 1 and 2 had significantly higher Modified Barthel Index scores comparing to group 3 at admission and discharge; this difference was more pronounced at discharge, mainly due to the greater reduction in group 3 (see Tables 3 and 4). On admission, no differences were found between TUG completers (groups 1 and 2); however, due to significant reduction in the Modified Barthel Index scores in group 2 at discharge, significant difference was found between groups 1 and 2. The model, adjusted for age, comorbidity (CCI), cognitive state (ALFI-MMSE) and length of hospitalization, suggests a ΔBarthel Index of − 3.68 for the TUG ≥ 12 group (decrease of 4.02%; mean ratio = 0.959, 95% C.I. = 0.931, 0.988) and − 7.26 for the TUG incompletion group (decrease of 9.44%; mean ratio = 0.905, 95% C.I. = 0.870, 0.942). This statistically significant reduction in the Modified Barthel Index, observed in groups 2 and 3, indicates a clinically significant functional decline.
Discussion
This study aimed to examine TUG as a possible screening tool for risk of functional decline in older hospitalized patients. The findings demonstrate that categorizing hospitalized ambulating older adults based on their TUG performance can add predictive information on their potential to experience HAFD. These findings suggest that the 12 s cut-off set by the CDC, as well as an incompletion category, can identify individuals at risk for significant HAFD and facilitate implementation of designated interventions aiming to maintain functional capacity; these findings remain significant while adjusting for age, comorbidity, cognitive state, and length of hospitalization of the participant.
Incompletion of the TUG test is a relatively underused and understudied metric, previously reported to predict falls in the context of acute care [37]. This novel use of the inability to complete TUG test among participants who were previously ambulatory, for prediction of significant functional decline, expands the potential contribution of the TUG test in patient screening. Differentiating between hospitalized patients at greater risk for functional decline is essential for best care practices; administrating the TUG test is simple, requires minimal resources, and provided an objective screening tool for risk of functional decline. Moreover, the chosen 12 s cut-off, more demanding than the commonly used 13.5 s [35], sets a relevant clinically valuable marker for the use of the TUG test for assessing risk of functional decline, supporting its use for promotion of early, in hospital, mobility interventions [51], or interventions following discharge [52]. Moreover, identifying individuals at greater risk for a significant HAFD may facilitate better utilization of health resources during and following hospitalization [53].
Significant differences in cognitive function and length of hospitalization between the groups were observed (Table 1). Indeed, cognitive status was previously associated with the TUG test [54], and length of hospitalization stay is also linked with greater HAFD [55]. Thus, we accounted for these variables in the statistical model that demonstrates the significant predictive value of the TUG test even after controlling them. Of note, patients with delirium or severe cognitive impairment were excluded.
Previous studies have demonstrated that various interventions during hospitalization, such as engaging patients in daily life activities and physical activities [2], can have a mediating effect on functional decline. Moreover, an individualized, multicomponent exercise intervention may reverse functional decline associated with hospitalization [1]. Patients identified as being at risk for functional decline should be the target population for such interventions and, comparably, when identifying patients with high mobility capacity and lower risk for functional decline, it may be advisable to refrain from limiting their mobility during hospitalization due to safety concerns [56], or use alternatives intending to promote mobility while maintaining safety.
Limitations: This study was conducted in two hospitals with a sample of relatively high functioning older adults; thus, its generalizability is limited. Future studies may examine the use of the three TUG categories for the prediction of functional decline in various samples of older inpatients to establish generalizability. Future studies are encouraged to use objective measures of activities of daily living, which may offer a broader perspective for function, thus expanding our understanding of the relationships between TUG test results and functional decline.
Conclusions and implications
This study has established the TUG test as a feasible screening tool for HAFD in older adults; by using the suggested categories, healthcare professionals can differentiate individuals at greater risk for functional decline. Older adults unable to successfully complete the TUG test in under 12 s or those unable to complete it altogether show significant functional decline following hospitalization, and thus may require early mobilization intervention effort, while hospitalized or immediately post-discharge, that may counteract the negative impact of acute hospitalization. Furthermore, where needed, additional resources (e.g., hospital-based physical therapy, informative guidance provided to accompanying family members) should be allocated to those at risk.
Data availability
The data that support the findings of this study are available from the corresponding author, MA, upon request.
Abbreviations
- HAFD:
-
Hospitalization Associated Functional Decline
- TUG:
-
Timed Up and Go
- CDC:
-
Centers for Disease Control and Prevention
- STEADI:
-
Stopping Elderly Accidents, Death and Injuries
- CCI:
-
Charlson’s comorbidity index
- ALFI-MMSE:
-
Adult Lifestyle and Function Interview—Mini-Mental State Examination
- DSCF:
-
Dwass-Steel-Critchlow-Fligner
References
Martínez-Velilla N, Casas-Herrero A, Zambom-Ferraresi F, de Souza, de Sáez Asteasu L ML, Lucia A, Galbete A, et al. Effect of exercise intervention on functional decline in very elderly patients during acute hospitalization: a randomized clinical trial. JAMA Internal Medicine. 2019;179:28–36.
Boltz M, Resnick B, Capezuti E, Shuluk J, Secic M. Functional decline in hospitalized older adults: can nursing make a difference? Geriatr Nurs. 2012;33(4):272–9. https://doi.org/10.1016/j.gerinurse.2012.01.008.
Brown CJ, Redden DT, Flood KL, Allman RM. The underrecognized epidemic of low mobility during hospitalization of older adults. J Am Geriatr Soc. 2009;57(9):1660–5. https://doi.org/10.1111/j.1532-5415.2009.02393.x.
Cohen Y, Zisberg A, Chayat Y, Gur-Yaish N, Gil E, Levin C, et al. Walking for better outcomes and recovery: the effect of WALK-FOR in preventing hospital-associated functional decline among older adults. The Journals of Gerontology: Series A. 2019;74(10):1664–70. https://doi.org/10.1093/gerona/glz025.
Ryan A, Wallace E, O’Hara P, Smith SM. Multimorbidity and functional decline in community-dwelling adults: a systematic review. Health Qual Life Outcomes. 2015;13(1):168. https://doi.org/10.1186/s12955-015-0355-9.
Zisberg A, Shadmi E, Sinoff G, Gur-Yaish N, Srulovici E, Admi H. Low mobility during hospitalization and functional decline in older adults. J Am Geriatr Soc. 2011;59(2):266–73. https://doi.org/10.1111/j.1532-5415.2010.03276.x.
Ley L, Khaw D, Duke M, Botti M. The dose of physical activity to minimise functional decline in older general medical patients receiving 24-hr acute care: a systematic scoping review. J Clin Nurs. 2019;28(17–18):3049–64. https://doi.org/10.1111/jocn.14872.
Takehito H, Shigeatsu H, Hideyuki K, Noriko H, Yumi K, Takako K, et al. Risk factors of falls in inpatients and their practical use in identifying high-risk persons at admission: Fukushima Medical University Hospital cohort study. BMJ Open. 2014;4(8):e005385. https://doi.org/10.1136/bmjopen-2014-005385.
McCusker J, Kakuma R, Abrahamowicz M. Predictors of functional decline in hospitalized elderly patients: a systematic review. The Journals of Gerontology: Series A. 2002;57(9):M569–77. https://doi.org/10.1093/gerona/57.9.M569.
Geyskens L, Jeuris A, Deschodt M, Van Grootven B, Gielen E, Flamaing J. Patient-related risk factors for in-hospital functional decline in older adults: a systematic review and meta-analysis. Age and Ageing. 2022;51:afac007. https://doi.org/10.1093/ageing/afac007.
Brach JS, Vanswearingen JM, Newman AB, Kriska AM. Identifying early decline of physical function in community-dwelling older women: performance-based and self-report measures. Phys Ther. 2002;82(4):320–8. https://doi.org/10.1093/ptj/82.4.320.
Reuben DB, Valle LA, Hays RD, Siu AL. Measuring physical function in community-dwelling older persons: a comparison of self-administered, interviewer-administered, and performance-based measures. J Am Geriatr Soc. 1995;43(1):17–23. https://doi.org/10.1111/j.1532-5415.1995.tb06236.x.
Johnson N, Barion A, Rademaker A, Rehkemper G, Weintraub S. The Activities of Daily Living Questionnaire: a validation study in patients with dementia. Alzheimer Dis Assoc Disord. 2004;18(4):223–30.
Patrizio E, Calvani R, Marzetti E, Cesari M. Physical functional assessment in older adults. J Frailty Aging. 2020;141:1–9. https://doi.org/10.14283/jfa.2020.61.
Numbers K, Jang S, Brodaty H, Sachdev PS, Draper B, Reppermund S. Instrumental activities of daily living by subjective and objective measures: the impact of depression and personality. Front Aging Neurosci. 2022;14:829544. https://doi.org/10.3389/fnagi.2022.829544.
Sutton M, Grimmer-Somers K, Jeffries L. Screening tools to identify hospitalised elderly patients at risk of functional decline: a systematic review. Int J Clin Pract. 2008;62(12):1900–9. https://doi.org/10.1111/j.1742-1241.2008.01930.x.
Sainsbury A, Seebass G, Bansal A, Young JB. Reliability of the Barthel Index when used with older people. Age Ageing. 2005;34(3):228–32. https://doi.org/10.1093/ageing/afi063.
Fi M. Functional evaluation: the Barthel index. Md State Med J. 1965;14:61–5.
Hachisuka K, Okazaki T, Ogata H. Self-rating Barthel index compatible with the original Barthel index and the Functional Independence Measure motor score. J UOEH. 1997;19(2):107–21.
Unnanuntana A, Jarusriwanna A, Nepal S. Validity and responsiveness of Barthel index for measuring functional recovery after hemiarthroplasty for femoral neck fracture. Arch Orthop Trauma Surg. 2018;138(12):1671–7. https://doi.org/10.1007/s00402-018-3020-z.
Bouwstra H, Smit EB, Wattel EM, van der Wouden JC, Hertogh CMPM, Terluin B, et al. Measurement properties of the Barthel Index in geriatric rehabilitation. J Am Med Dir Assoc. 2019;20(4):420-5.e1. https://doi.org/10.1016/j.jamda.2018.09.033.
Hsieh Y-W, Wang C-H, Wu S-C, Chen P-C, Sheu C-F, Hsieh C-L. Establishing the minimal clinically important difference of the Barthel Index in stroke patients. Neurorehabil Neural Repair. 2007;21(3):233–8. https://doi.org/10.1177/1545968306294729.
Shumway-Cook A, Brauer S, Woollacott M. Predicting the probability for falls in community-dwelling older adults using the Timed Up & Go Test. Phys Ther. 2000;80(9):896–903.
Benavent-Caballer V, Sendín-Magdalena A, Lisón JF, Rosado-Calatayud P, Amer-Cuenca JJ, Salvador-Coloma P, et al. Physical factors underlying the Timed “Up and Go” test in older adults. Geriatr Nurs. 2016;37(2):122–7. https://doi.org/10.1016/j.gerinurse.2015.11.002.
Pedrosa R, Holanda G. Correlation between the walk, 2-minute step and tug tests among hypertensive older women. Braz J Phys Ther. 2009;13(3):252–6. https://doi.org/10.1590/s1413-35552009005000030.
Park S-H. Tools for assessing fall risk in the elderly: a systematic review and meta-analysis. Aging Clin Exp Res. 2018;30(1):1–16.
Neser SB. Stopping elderly accidents, deaths and injuries: fall prevention for community-dwelling older adults. STEADI Fall Prevention 2020.
Alexandre TS, Meira DM, Rico NC, Mizuta SK. Accuracy of Timed Up and Go Test for screening risk of falls among community-dwelling elderly. Braz J Phys Ther. 2012;16(5):381–8. https://doi.org/10.1590/s1413-35552012005000041.
Savva GM, Donoghue OA, Horgan F, O’Regan C, Cronin H, Kenny RA. Using Timed Up-and-Go to identify frail members of the older population. J Gerontol Ser A. 2012;68(4):441–6. https://doi.org/10.1093/gerona/gls190.
Brusse KJ, Zimdars S, Zalewski KR, Steffen TM. Testing functional performance in people with Parkinson disease. Phys Ther. 2005;85(2):134–41. https://doi.org/10.1093/ptj/85.2.134.
Eagles D, Perry JJ, Sirois M-J, Lang E, Daoust R, Lee J, et al. Timed Up and Go predicts functional decline in older patients presenting to the emergency department following minor trauma†. Age Ageing. 2016;46(2):214–8. https://doi.org/10.1093/ageing/afw184.
Donoghue OA, Horgan NF, Savva GM, Cronin H, O’Regan C, Kenny RA. Association between Timed Up-and-Go and memory, executive function, and processing speed. J Am Geriatr Soc. 2012;60(9):1681–6. https://doi.org/10.1111/j.1532-5415.2012.04120.x.
de Morton NA, Davidson M, Keating JL. The de Morton Mobility Index (DEMMI): an essential health index for an ageing world. Health Qual Life Outcomes. 2008;6:1–15.
Tinetti ME, Franklin Williams T, Mayewski R. Fall risk index for elderly patients based on number of chronic disabilities. Am J Med. 1986;80(3):429–34. https://doi.org/10.1016/0002-9343(86)90717-5.
Schoene D, Wu SMS, Mikolaizak AS, Menant JC, Smith ST, Delbaere K, et al. Discriminative ability and predictive validity of the Timed Up and Go Test in identifying older people who fall: systematic review and meta-analysis. J Am Geriatr Soc. 2013;61(2):202–8. https://doi.org/10.1111/jgs.12106.
Sarmiento K, Lee R. STEADI: CDC’s approach to make older adult fall prevention part of every primary care practice. J Safety Res. 2017;63:105–9. https://doi.org/10.1016/j.jsr.2017.08.003.
Large J, Gan N, Basic D, Jennings N. Using the Timed Up and Go Test to stratify elderly inpatients at risk of falls. Clin Rehabil. 2006;20(5):421–8. https://doi.org/10.1191/0269215506cr959oa.
Gan N, Large J, Basic D, Jennings N. The Timed Up and Go Test does not predict length of stay on an acute geriatric ward. Australian Journal of Physiotherapy. 2006;52(2):141–4. https://doi.org/10.1016/S0004-9514(06)70050-2.
Bassett AM, Siu K-C, Honaker JA. Functional measures for fall risk in the acute care setting: a review. West J Nurs Res. 2018;40(10):1469–88. https://doi.org/10.1177/0193945917705321.
Graf C. Functional decline in hospitalized older adults: it’s often a consequence of hospitalization, but it doesn’t have to be. AJN The American Journal of Nursing. 2006;106(1):58–67.
Pfeiffer E. A Short Portable Mental Status Questionnaire for the assessment of organic brain deficit in elderly patients†. J Am Geriatr Soc. 1975;23(10):433–41. https://doi.org/10.1111/j.1532-5415.1975.tb00927.x.
Bellelli G, Morandi A, Davis DHJ, Mazzola P, Turco R, Gentile S, et al. Validation of the 4AT, a new instrument for rapid delirium screening: a study in 234 hospitalised older people. Age Ageing. 2014;43(4):496–502. https://doi.org/10.1093/ageing/afu021.
Podsiadlo D, Richardson S. The Timed “Up & Go”: a test of basic functional mobility for frail elderly persons. J Am Geriatr Soc. 1991;39(2):142–8. https://doi.org/10.1111/j.1532-5415.1991.tb01616.x.
Christopher A, Kraft E, Olenick H, Kiesling R, Doty A. The reliability and validity of the Timed Up and Go as a clinical tool in individuals with and without disabilities across a lifespan: a systematic review. Disabil Rehabil. 2021;43(13):1799–813. https://doi.org/10.1080/09638288.2019.1682066.
Shah S, Vanclay F, Cooper B. Improving the sensitivity of the Barthel Index for stroke rehabilitation. J Clin Epidemiol. 1989;42(8):703–9. https://doi.org/10.1016/0895-4356(89)90065-6.
Wang Y-C, Chang P-F, Chen Y-M, Lee Y-C, Huang S-L, Chen M-H, et al. Comparison of responsiveness of the Barthel Index and modified Barthel Index in patients with stroke. Disabil Rehabil. 2023;45(6):1097–102. https://doi.org/10.1080/09638288.2022.2055166.
Quinn TJ, Langhorne P, Stott DJ. Barthel Index for stroke trials. Stroke. 2011;42(4):1146–51. https://doi.org/10.1161/STROKEAHA.110.598540.
Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–83. https://doi.org/10.1016/0021-9681(87)90171-8.
Roccaforte WH, Burke WJ, Bayer BL, Wengel SP. Validation of a telephone version of the mini-mental state examination. J Am Geriatr Soc. 1992;40(7):697–702. https://doi.org/10.1111/j.1532-5415.1992.tb01962.x.
The jamovi project (2023). jamovi (Version 2.4) [Computer Software]. Retrieved from https://www.jamovi.org.
Gil E, Zisberg A, Shadmi E, Gur-Yaish N, Shulyaev K, Chayat Y, et al. Still WALKing-FOR: 2-year sustainability of the ‘WALK FOR’ intervention. Age and Ageing. 2023;52:afad115. https://doi.org/10.1093/ageing/afad115.
Urquiza M, Echeverria I, Besga A, Amasene M, Labayen I, Rodriguez-Larrad A, et al. Determinants of participation in a post-hospitalization physical exercise program for older adults. BMC Geriatr. 2020;20(1):408. https://doi.org/10.1186/s12877-020-01821-3.
Fried TR, Bradley EH, Williams CS, Tinetti ME. Functional disability and health care expenditures for older persons. Arch Intern Med. 2001;161(21):2602–7. https://doi.org/10.1001/archinte.161.21.2602.
Ansai JH, Andrade LPd, Nakagawa TH, Vale FAC, Caetano MJD, Lord SR, et al. Cognitive correlates of Timed Up and Go subtasks in older people with preserved cognition, mild cognitive impairment, and Alzheimer’s disease. Am J Phys Med Rehabil. 2017;96:700–5.
Zisberg A, Shadmi E, Gur-Yaish N, Tonkikh O, Sinoff G. Hospital-associated functional decline: the role of hospitalization processes beyond individual risk factors. J Am Geriatr Soc. 2015;63(1):55–62. https://doi.org/10.1111/jgs.13193.
Growdon ME, Shorr RI, Inouye SK. The tension between promoting mobility and preventing falls in the hospital. JAMA Intern Med. 2017;177(6):759. https://doi.org/10.1001/jamainternmed.2017.0840.
Funding
Open access funding provided by University of Haifa. This study was funded by the Israel Science Foundation (ISF 1216/17).
Author information
Authors and Affiliations
Contributions
All authors contributed to this manuscript; MA, EF, OGH, and RTS—conceptualization and writing; OGH—data collection; KA—analysis and writing; OD—writing and editing. All authors reviewed and edited the final draft and approved the submission for publication.
Corresponding author
Ethics declarations
Ethics approval
Ethics approval for the study design was provided by the ethics committee of the Faculty of Social Welfare and Health Sciences, University of Haifa, Israel (approval no. 324/17). The study was also approved by the Helsinki committees of Haemek and Bnei Zion medical centers.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Gatenio-Hefling, O., Tzemah-Shahar, R., Asraf, K. et al. Revisiting the “Timed Up and Go” test: a 12-s cut-off can predict Hospitalization Associated Functional Decline in older adults. GeroScience (2024). https://doi.org/10.1007/s11357-024-01280-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11357-024-01280-3