Abstract
Self-rated health (SRH) is a subjective indicator of overall health based on a single questionnaire item. Previous evidence found that it is a strong predictor of mortality, although the underlying mechanism is poorly understood. Epigenetic age is an objective, emerging biomarker of health, estimated using DNA methylation data at hundreds of sites across the genome. This study aimed to assess the overlap and interaction between SRH and epigenetic ageing in predicting mortality risk. We used DNA methylation data from 1059 participants in the Melbourne Collaborative Cohort Study (mean age: 69 years) to calculate three age-adjusted measures of epigenetic ageing: GrimAge, PhenoAge, and DunedinPACE. SRH was assessed using a five-category questionnaire item (“excellent, very good, good, fair, poor”). Cox models were used to assess the associations of SRH, epigenetic ageing, and their interaction, with all-cause mortality over up to 17 years of follow-up (Ndeaths = 345). The association of SRH with mortality per category increase was HR = 1.29; 95%CI: 1.14–1.46. The association was slightly attenuated after adjusting for all three epigenetic ageing measures (HR = 1.25, 95%CI: 1.10–1.41). A strong gradient was observed in the association of GrimAge (Pinteraction = 0.006) and DunedinPACE (Pinteraction = 0.002) with mortality across worsening SRH strata. For example, the association between DunedinPACE and mortality in participants with “excellent” SRH was HR = 1.02, 95%CI: 0.73–1.43 and for “fair/poor” HR = 1.72, 95%CI: 1.35–2.20. SRH and epigenetic ageing were synergistic risk factors of mortality in our study. These findings suggest that consideration of subjective and objective factors may improve general health assessment, which has implications for the ongoing development of molecular markers of ageing.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Self-rated health (SRH) is a widely used subjective summative measure of health referred to as an “active cognitive process” that indicates individuals’ physical and mental health in conjunction with their objective clinical conditions, social characteristics, and even genetic factors [1]. It has been consistently observed that poorer SRH is associated with higher risk of all-cause and cause-specific mortality [2,3,4,5,6,7,8]. A substantial body of research has also shown that this association cannot be fully explained by a range of physiological and non-physiological factors that contribute to health [1, 4, 9], which highlights that, despite being simple and subjective, SRH provides a valuable assessment of health.
SRH is associated with many biomarkers of ageing. In a study that included over 15,000 adults sampled from three cohorts, SRH was associated with 57 out of 150 biomarkers that are closely related to physiological regulation [10]. Poor SRH has consistently been found to be associated with low-grade inflammation and elevated levels of inflammatory biomarkers such as interleukin-6 and C-reactive protein (CRP) [11,12,13,14] which are important indicators of biological ageing [15,16,17]. Many studies have examined the relative value of SRH and objective markers of health in predicting mortality. A study based on nearly 500,000 participants in the UK Biobank assessed the associations of 655 demographic, lifestyle, and health markers with 5-year all-cause mortality and found that SRH was more strongly predictive of mortality than the majority of more objective markers of health such as walking pace, illnesses and disability [18]. Another study of 8138 participants in the Northern Ireland Cohort for the Longitudinal Study of Ageing found that the risk of mortality associated with poor SRH was higher than with limiting long-term illnesses (any long-term illnesses or disability and whether these conditions limited activities), but lower than with a modified Charlson Index (calculated based on 16 selected chronic conditions) [4]. Some studies also explored how SRH might interact with objective health indicators in their association with mortality [7, 19], and one found that the association of SRH with mortality was stronger in participants with type II diabetes [19].
DNA methylation (DNAm)-based markers of ageing, “epigenetic ageing”, are well-established and powerful measures of biological age [20, 21]. A previous review that compared six biological age predictors: epigenetic age, telomere length, transcriptomic, proteomic and metabolomics-based predictors, and composite biomarker predictors, concluded that epigenetic age is currently the most valid and predictive measure of biological age [22], and epigenetic ageing markers have been considerably improved since the review was published [23,24,25,26]. Therefore, we hypothesised that with epigenetic ageing being such an excellent estimator of biological age, it might contribute to explain the mechanisms by which SRH relates to poor health at the molecular level.
Limited research has investigated the link between SRH and epigenetic ageing. DunedinPACE, a third-generation epigenetic clock, was found to be correlated with SRH [25]. In another cohort study, SRH was reported to mediate the association between subjective age (how old individuals perceived themselves relative to their chronological age) and PhenoAge [27]. Although the respective individual associations of SRH and epigenetic ageing with mortality have been studied extensively [2, 4,5,6, 28, 29], there is a lack of evidence on i) whether epigenetic ageing could provide an explanation for the SRH/mortality association; ii) whether epigenetic ageing measures, developed using clinical markers, encompass subjective aspects of the ageing process; and iii) whether these subjective and objective markers could have a synergistic effect on mortality prediction. Therefore, we investigated the overlap and interaction between SRH and epigenetic ageing to help explain the underlying mechanism of SRH in predicting mortality and inform precision prevention of mortality and morbidity.
This study aimed to assess in a large sample of middle-aged and older Australians: 1) the extent to which epigenetic ageing captures the association between SRH and mortality, and 2) the joint effect of epigenetic ageing and SRH on mortality.
Methods
Study participants
The Melbourne Collaborative Cohort Study (MCCS) is a prospective cohort study of 41,513 middle-aged to older Australians (59% females) of white European origin who were aged between 40 and 69 (99% of them) at recruitment between 1990 and 1994 (baseline) [30]. A face-to-face follow-up (follow-up 2) was carried out between 2003 and 2007 and data on lifestyle, health status, physical measurements and blood samples were collected [30].
The present study used follow-up 2 data of a subset of 1100 controls from six cancer case–control studies nested in the MCCS. Genome-wide DNA methylation was measured in participants who had provided blood samples (stored as dried blood spot on a Guthrie card) at follow-up using the Illumina HumanMethylation450K BeadChip array [30]. Details of DNA extraction and processing and quality control of methylation data have been described elsewhere [31,32,33]. After excluding participants who failed DNAm quality control (n = 12, 1%) and those with missing data for SRH (n = 29, 3%), 1059 participants were included in the analysis.
Participants were passively followed from the time they attended the follow-up interview to 31st October, 2019, and deaths were identified by annual record linkage to the Victorian Registry of Births, Deaths and Marriages [30].
The MCCS was approved by the Human Research Ethics Committee of the Cancer Council Victoria, Melbourne, VIC, Australia, and informed consent was provided by all participants according to the Declaration of Helsinki.
Self-rated health
SRH was one item extracted from the 12-Item Short Form Survey [1, 34] used at follow-up 2 and collected by asking participants: “In general, would you say your health is …?” with five response options provided: excellent, very good, good, fair, and poor. Since only 20 participants reported “poor” health the “poor” and “fair” categories were merged into one “fair/poor” category. SRH was also used as a pseudo-continuous variable scored from 0 to 3, with 0 representing “excellent” health.
Epigenetic ageing
Three epigenetic ageing measures that are widely used and most strongly associated with mortality were considered in this study: GrimAge, PhenoAge, and DunedinPACE. GrimAge was developed with chronological age, sex, and DNAm predictors of smoking pack-years and seven plasma proteins based on 1030 CpGs [24]. PhenoAge incorporated 513 CpGs selected based on chronological age and nine clinical markers predictive of mortality [23]. DunedinPACE measures the rate of ageing with 173 CpGs based on the Pace of Ageing calculated from changes in 19 biomarkers [25]. In the MCCS, GrimAge and PhenoAge were calculated using the Horvath Lab’s web tool (http://dnamage.genetics.ucla.edu/new), and DunedinPACE using the R code provided in the original publication [25, 35]. All three measures were regressed on chronological age and the residuals were used as the age-adjusted measures of epigenetic ageing in all analyses. Since these measures are expressed on a different scale, we standardised them to a mean of 0 and standard deviation of 1 in the survival analyses.
Confounders
We considered age, sex, smoking status (never/former/current smokers), and country of birth (Australia/New Zealand/other, UK/Malta, Greece, and Italy) as major confounding factors. Physical measurements on waist circumference, weight, height, blood pressure, and resting heart rate were carried out by trained personnel and the average values from 2–3 measurements were calculated [30]. BMI (kg/m2) was calculated using weight and height data. Blood glucose concentration (mmol/L) was measured with a glucometer (95% fasted). The low-density (LDL) and high-density lipoprotein (HDL) cholesterol concentrations were also measured [30]. A fatigue score (soma-6) was created by summing the SOMA-6 part of the 12-item Somatic and Psychological Health Report questionnaire [36] where one point was assigned to each item (ranges 0–6, with higher score representing severer fatigue).
Statistical analysis
Pearson correlation coefficients of SRH with epigenetic ageing and between different epigenetic ageing measures (all age-adjusted) were calculated. Since GrimAge was developed based on sex and a DNAm-based marker of smoking pack-years [24], we expected that it would capture the effects of smoking and sex on mortality risk; to validate the logic of our study, we compared Cox models including these factors with and without adjustment for GrimAge.
A series of Cox proportional hazard models with time since blood draw as the time-scale were applied to assess the association between SRH and mortality. Four models were considered: 1) adjusted for age at blood draw, sex, and country of birth; 2) additionally adjusted for each individual epigenetic ageing measure; 3) adjusting for all three epigenetic ageing measures; 4) adding an interaction term between SRH and epigenetic ageing to Model 2. Likelihood ratio tests comparing Model 4 to Model 2 were applied to test for potential interactions between SRH and epigenetic age. The concordance statistic (c-index) was calculated for all models to evaluate the prediction of mortality obtained for different combinations of subjective and objective health indicators.
Sensitivity analysis
To further assess the independence of the association for SRH with mortality, we added more covariates to Model 2, including smoking status, waist circumference, height, BMI, blood glucose concentration, HDL and LDL cholesterol concentrations, systolic blood pressure, resting heart rate, and soma-6 score.
All statistical analyses were conducted with R version 4.2.2 (Vienna, Austria, 2022) and all P-values were two-sided.
Results
Sample characteristics
The average age of the 1059 participants at follow-up 2 was 68.7 years (SD = 8.1) and 345 (33%) died over a mean follow-up of 13.0 years (range: 0.3–17.2 years), Table 1. Participants reporting poorer SRH were older than those reporting better SRH (e.g. mean age for “poor” health: 74.1 years; for “excellent” health: 66.6 years). SRH was positively correlated with epigenetic ageing (Figure S1), and the correlation coefficients were greater than that with chronological age (r = 0.15), ranging between r = 0.16 for PhenoAge and r = 0.23 for DunedinPACE, Table S1. There was moderate correlation between epigenetic ageing measures with the strongest correlation between GrimAge and DunedinPACE (r = 0.61).
Smoking, sex, and mortality
Compared to never smokers, current smokers had strongly elevated mortality risk (HR = 2.3, 95%CI: 1.4–3.7; Table S2) as did former smokers (HR = 1.3; 95%CI: 1.1–1.7). After adjusting for GrimAge, these associations were very close to null: current smokers: HR = 1.1, 95%CI: 0.7–2.0, former smokers: HR = 1.0, 95%CI: 0.8–1.3, whereas the association for GrimAge remained strong (per SD: HR = 1.4; P = 5 × 10–8). Similarly, the mortality risk for males compared to females attenuated from 1.4 (95%CI: 1.1–1.8) to 1.1 (95%CI: 0.9–1.5) after adjusting for GrimAge. There was also some but less significant reduction of the HRs for smoking status and sex after adjusting for DunedinPACE (e.g. for current smokers compared to never smokers: HR = 1.7, 95%CI: 1.0–2.8). Conversely, these associations remained virtually unchanged after adjustment for SRH and PhenoAge (Table S2).
SRH and mortality
Participants reporting “fair/poor” health had substantially higher mortality than those reporting “excellent” health (HR = 2.02; 95%CI: 1.36–2.99; Table 2), whereas those reporting “very good” health had a similar mortality risk (HR = 1.01; 95%CI: 0.71–1.43). There was small attenuation of the HRs after adjusting for epigenetic ageing. For example, after adjusting for GrimAge, the HR for “fair/poor” health compared to “excellent” health attenuated to 1.85 (95%CI: 1.25–2.75).
When SRH was analysed as a pseudo-continuous variable, a unit increase in SRH was associated with a 1.29-fold (95%CI: 1.14–1.46, P = 4 × 10–5; Table 3) increase in mortality risk, whereas the HR per SD increase of GrimAge was HR = 1.45 (P = 5 × 10–11), which was greater than for DunedinPACE (per SD, HR = 1.34; P = 9 × 10–8) and PhenoAge (per SD, HR = 1.20; P = 2 × 10–4). The HR for SRH decreased to 1.25 (95%CI: 1.11–1.42) after adjusting for GrimAge or DunedinPACE and to 1.26 (95%CI: 1.11–1.43) after adjusting for PhenoAge; it was not further attenuated after adjustment for all three epigenetic ageing measures: HR = 1.25 (95%CI: 1.10–1.41). Similarly, there was only negligible attenuation of the HRs for epigenetic ageing after adjusting for SRH (e.g. GrimAge: HR = 1.43, 95%CI: 1.28–1.60).
Interaction between SRH and epigenetic ageing
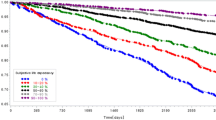
We observed strong evidence of interactions of SRH with GrimAge (P = 0.006) and DunedinPACE (P = 0.002), but not with PhenoAge (P = 0.92), with a stronger association of SRH with mortality in participants with higher GrimAge or DunedinPACE (Fig. 1). This is further illustrated in Fig. 2, showing a strong gradient across SRH strata for the association of GrimAge (or DunedinPACE) with mortality, which was small in participants reporting “excellent” SRH (GrimAge: HR = 1.15, 95%CI: 0.84–1.59; DunedinPACE: HR = 1.02, 95%CI: 0.73–1.43), and very large in those reporting “fair/poor” SRH (GrimAge: HR = 1.64, 95%CI: 1.31–2.04; DunedinPACE: HR = 1.72, 95%CI: 1.35–2.20).
Interaction between SRH and epigenetic ageing measures in their associations with all-cause mortality (n = 1059, ndeaths = 345). *Models adjusted for age, sex, country of birth, SRH (continuous), epigenetic ageing, and an interaction term between SRH and epigenetic ageing. All epigenetic ageing measures were standardised to a mean of 0 and standard deviation of 1
Associations of epigenetic ageing with all-cause mortality across self-rated health strata (n = 1059, ndeaths = 345). *Models adjusted for age, sex, country of birth, SRH (categorical), epigenetic ageing, and an interaction term between SRH and epigenetic ageing. All epigenetic ageing measures were standardised to a mean of 0 and standard deviation of 1
Sensitivity analysis
Very similar results were observed in the association between SRH and mortality after adjustment of a large number of health-related lifestyle variables and biomarkers (based on 802 participants, adjusting for GrimAge: HR = 1.28; 95%CI: 1.09–1.50; Table S3). There was also no notable change to the associations of epigenetic ageing measures with mortality.
Contribution to prediction
In univariate models, the c-index was 0.589 for SRH, 0.590 for GrimAge, 0.552 for PhenoAge, 0.574 for DunedinPACE, which was substantially lower than Model 0 (age, sex, and country of birth, c = 0.748), Table S4. Adding SRH to Model 0 (Model 1) increased the c-index to 0.756. This was slightly lower than for GrimAge (c = 0.763) and DunedinPACE (c = 0.760), but higher than for PhenoAge (c = 0.754). Adding epigenetic ageing to Model 1 further increased the c-index (e.g. GrimAge: c = 0.768) with minimal increase after including all three epigenetic clocks (c = 0.769). Models using continuous or categorical SRH had similar c-indices. Some further increase in the c-index was observed after including an interaction term between SRH score and epigenetic ageing (e.g. GrimAge: c = 0.771). In the sensitivity analysis, inclusion of more covariates in the model also increased the c-index (to 0.782 for GrimAge and to 0.777 for PhenoAge and DunedinPACE).
Discussion
This study found that the association of SRH with long-term all-cause mortality was largely not explained by a group of objective markers of biological ageing (epigenetic age) in a large sample of middle-aged and older Australians. Both subjective and objective health assessments showed strong associations with mortality. GrimAge appeared to be the best mortality predictor among the four, followed by DunedinPACE, while SRH and PhenoAge showed similar results in mortality prediction. Combining SRH and epigenetic age improved mortality prediction of the models. GrimAge and DunedinPACE strongly interacted with SRH, with risk of death being much stronger in participants with higher GrimAge or DunedinPACE and poorer SRH. No interaction was observed for PhenoAge, which is an epigenetic ageing measure less strongly predictive of mortality. Lifestyle-related variables and clinical markers did not appear to explain any of the associations of SRH and epigenetic ageing with mortality.
Our findings on the association between SRH and mortality are consistent with previous studies, where only part of the SRH/mortality association could be explained by a wide range of indicators of physical function, biomarkers of ageing and inflammation, medical and psychological conditions, and lifestyle and psycho-social factors [2,3,4,5,6,7, 9, 10, 37, 38]. For example, in the study by Kananen et al., the relative risk of mortality for “poor” SRH compared to “good” SRH attenuated from 2.6 to 2.4 after adjusting for the number of chronic diseases, and to 2.0 after further including ten biomarkers that were strongly associated with SRH [10]. A study based on the Chinese Longitudinal Healthy Longevity Survey observed a relative risk attenuation of 15% after adjusting for major health risk factors including chronic diseases and cognitive impairment [38]. Although investigating the interactions between SRH and objective health indicators may help identify population subgroups more suitable to receive health interventions according to their health status, to our knowledge very few studies have examined such interactions [7, 19]. Wuorela et al. found no interaction between SRH and a frailty index [7], whereas Dankner et al. observed that the association between SRH and mortality was stronger in participants with type II diabetes than their normoglycemic counterparts [19].
Similarly, epigenetic ageing was found to be largely independent of other biological age estimators. In 1314, Scottish individuals aged 70–90 years [39] the first-generation epigenetic clocks and telomere length were independently associated with mortality. Using MCCS data, we previously found that inflammaging (increased concentrations of age-related inflammation markers) only explained a small amount of the association between epigenetic ageing and mortality [40]. Another study assessed the longitudinal association between nine biological ageing measures (including four epigenetic clocks) and mortality and reported that GrimAge and HorvathAge, but not PhenoAge and HannumAge, were independently associated with mortality [41].
The variation between epigenetic ageing measures also aligned with existing evidence. These measures were developed to estimate different aspects of ageing: PhenoAge was developed to predict phenotypic age based on ten clinical markers [23]; GrimAge was developed based on eight DNAm-based surrogate markers to predict mortality [24], while DunedinPACE used DNAm-based surrogated markers of rate of changes in 19 selected biomarkers in four waves of follow-up over 20 years to estimate the rate of ageing [25]. Such variation can be seen in previous studies. For example, DunedinPACE had the strongest association with obesity compared to PhenoAge and GrimAge since it incorporates more obesity-related markers of ageing [42], PhenoAge and GrimAge showed slightly different patterns of association with risk of various cancers, GrimAge being more strongly associated with lung and urothelial cancer risk, which are mainly smoking-related [43]. A randomized controlled trial found that caloric restriction caused reduction only in DunedinPACE, but not in GrimAge or PhenoAge [44].
Despite intense exploration of both SRH and epigenetic ageing in previous studies, to our knowledge, this is the first time these two variables have been considered jointly and a strong interaction was found between them. Epigenetic ageing measures, which have been developed based on clinical markers to predict mortality, appeared to be better predictors of mortality in those reporting fair/poor health, and were less effective in participants reporting to be very healthy. Our study therefore highlights that SRH, as a subjective measure of health which plays an important role in mortality prediction regardless of many objective health indicators, might have important implications for the interpretation and ongoing development of biological age estimators. Future studies could also explore the associations between other epigenetic markers and SRH, which could be helpful in developing potential epigenetic measures that capture subjective aspects of ageing.
This study has some limitations. Although our sample was reasonably large, our findings should be replicated and extended in additional and larger studies. The MCCS participants were healthier than the general population [45], which may not have caused major bias because selection bias is usually considered to be small and a previous study reported that excluding participants who were too sick to respond to SRH questions had little impact on the effect estimates of the SRH/mortality association [38]. A shared limitation of our study and others is that SRH was collected at only one time point. Since SRH is expected to change with time [1], SRH information collected at additional time points might capture its association with mortality more accurately. In our study, the participants were followed for an average of 13 years and both SRH and epigenetic ageing measures were less predictive of long-term than short-term mortality, but the results were materially unchanged when follow-up time was restricted to five or ten years (not shown).
Evidence from our study and others suggests that the mechanisms underlying the association between SRH and mortality are not fully explained by objective factors including diseases, biomarkers, lifestyle, and psycho-social factors usually collected in large epidemiological studies. Although the epigenetic biomarkers of ageing we assessed use information from many DNAm sites (173 CpGs for DunedinPACE to 1030 GpGs for GrimAge), were designed to capture the collective effect of a large number of health-related variables and biomarkers of physiological functions, and have been widely reported to be excellent markers of ageing, they also accounted for a small proportion of the SRH/mortality association. This conclusion was further supported by our validation test showing that GrimAge almost entirely captured the effect of smoking and sex on mortality [24]. Future studies could consider other biological, clinical, and psycho-social variables that may explain why individuals reporting their health to be poor die younger.
In conclusion, SRH and epigenetic ageing were correlated with each other, both strongly associated with mortality, and showed a strong interaction whereby the associations of GrimAge and DunedinPACE with mortality was close to null in participants reporting excellent health and very large in those reporting poor health. These findings highlight that both subjective and objective markers of ageing are important to comprehensively evaluate an individual’s health and risk of mortality. This has implications for the ongoing development of molecular markers of ageing. Additional research efforts are required to uncover the mechanisms underlying the association between SRH and mortality and identify potential molecular markers underlying poor self-rated health.
Data availability
Due to ethical constraints related to the consent of participants, we cannot share the full deidentified dataset. For most participants included in this study, the data are publicly available under controlled-access at dbGaP (#phs003213.v1.p1, for which more details can be found at https://www.ncbi.nlm.nih.gov/projects/gap/cgi-bin/study.cgi?study_id=phs003213.v1.p1).
References
Jylhä M. What is self-rated health and why does it predict mortality? Towards a unified conceptual model. Soc Sci Med. 2009;69(3):307–16. https://doi.org/10.1016/j.socscimed.2009.05.013.
Dramé M, Cantegrit E, Godaert L. Self-rated health as a predictor of mortality in older adults: a systematic review. Enviro Res Publ Health. 2023;20(5):3813. https://doi.org/10.3390/ijerph20053813.
Lorem G, Cook S, Leon DA, Emaus N, Schirmer H. Self-reported health as a predictor of mortality: A cohort study of its relation to other health measurements and observation time. Sci Rep. 2020;10(1):4886. https://doi.org/10.1038/s41598-020-61603-0.
Miller AC, O’Reilly D, Kee F, Cruise S, Young I. Multimorbidity, activity limitation and self-reported health all predict mortality risk, but better measures were required. J Clin Epidemiol. 2022;144:144–62. https://doi.org/10.1016/j.jclinepi.2021.12.010.
DeSalvo KB, Bloser N, Reynolds K, He J, Muntner P. Mortality prediction with a single general self-rated health question. J Gen Intern Med. 2006;21(3):267–75. https://doi.org/10.1111/j.1525-1497.2005.00291.x.
Torres-Collado L, García de la Hera M, Compañ-Gabucio L, Oncina-Cánovas A, González-Palacios S, Notario-Barandiaran L, et al. Self-reported health status and mortality from all-causes of death, cardiovascular disease and cancer in an older adult population in Spain. PLoS ONE. 2022;17(1):0261782. https://doi.org/10.1371/journal.pone.0261782.
Wuorela M, Lavonius S, Salminen M, Vahlberg T, Viitanen M, Viikari L. Self-rated health and objective health status as predictors of all-cause mortality among older people: a prospective study with a 5-, 10-, and 27-year follow-up. BMC Geriatr. 2020;20(1):120. https://doi.org/10.1186/s12877-020-01516-9.
Shen C, Schooling CM, Chan WM, Zhou JX, Johnston JM, Lee SY, et al. Self-rated health and mortality in a prospective Chinese elderly cohort study in Hong Kong. Prev Med. 2014;67:112–8. https://doi.org/10.1016/j.ypmed.2014.07.018.
Xiong S, Wang Z, Lee B, Guo Q, Peoples N, Jin X, et al. The association between self-rated health and all-cause mortality and explanatory factors in China's oldest-old population. 2022(2047–2986 (Electronic)). https://doi.org/10.7189/jogh.12.11005.
Kananen L, Enroth L, Raitanen J, Jylhävä J, Bürkle A, Moreno-Villanueva M, et al. Self-rated health in individuals with and without disease is associated with multiple biomarkers representing multiple biological domains. Sci Rep. 2021;11(1):6139. https://doi.org/10.1038/s41598-021-85668-7.
Carin W, Mats L, Tomas H, Kimmo S, Bo M, Anna A. Is poor self-rated health associated with low-grade inflammation in 43 110 late adolescent men of the general population? A cross-sectional study. BMJ Open. 2016;6(4):e009440. https://doi.org/10.1136/bmjopen-2015-009440.
Arnberg FK, Lekander M, Morey JN, Segerstrom SC. Self-rated health and interleukin-6: Longitudinal relationships in older adults. Brain Behav Immun. 2016;54:226–32. https://doi.org/10.1016/j.bbi.2016.02.008.
Leshem-Rubinow E, Shenhar-Tsarfaty S, Milwidsky A, Toker S, Shapira I, Berliner S, et al. Self-rated Health is associated with elevated c-reactive Protein even among apparently Healthy individuals. Isreal Medical Association Journal. 2015;14(4).
Christian LM, Glaser R, Porter K, Malarkey WB, Beversdorf D, Kiecolt-Glaser JK. Poorer self-rated health is associated with elevated inflammatory markers among older adults. Psychoneuroendocrinology. 2011;36(10):1495–504. https://doi.org/10.1016/j.psyneuen.2011.04.003.
Santos A, Sinha S. Obesity and aging: Molecular mechanisms and therapeutic approaches Ageing Research Reviews. 2021;67. https://doi.org/10.1016/j.arr.2021.101268.
Puzianowska-Kuźnicka M, Owczarz M, Wieczorowska-Tobis K, Nadrowski P, Chudek J, Slusarczyk P, et al. Interleukin-6 and C-reactive protein, successful aging, and mortality: the PolSenior study. Immunity and Ageing. 2016;13(21). https://doi.org/10.1186/s12979-016-0076-x.
Dugué PA, Hodge AM, Ulvik A, Ueland PM, Midttun Ø, Rinaldi SAO, et al. Association of Markers of Inflammation, the Kynurenine Pathway and B Vitamins with Age and Mortality, and a Signature of Inflammaging. J Gerontol: Ser. 2022;77(4):826–36. https://doi.org/10.1093/gerona/glab163.
Ganna A, Ingelsson E. 5 year mortality predictors in 498 103 UK Biobank participants: a prospective population-based study. Lancet. 2015;386(9993):533–40. https://doi.org/10.1016/S0140-6736(15)60175-1.
Dankner R, Olmer L, Kaplan G, Chetrit A. The joint association of self-rated health and diabetes status on 14-year mortality in elderly men and women. Qual Life Res. 2016;25(11):2889–96. https://doi.org/10.1007/s11136-016-1291-9.
Oblak L, van der Zaag J, Higgins-Chen AT, Levine ME, Boks MP. A systematic review of biological, social and environmental factors associated with epigenetic clock acceleration. Ageing Research Reviews. 2021;69:101348 %U https://linkinghub.elsevier.com/retrieve/pii/S1568163721000957. https://doi.org/10.1016/j.arr.2021.101348
Horvath S, Raj K. DNA methylation-based biomarkers and the epigenetic clock theory of ageing. Nature Reviews Genetics. 2018;19(6):371–84 %U http://www.nature.com/articles/s41576-018-0004-3. https://doi.org/10.1038/s41576-018-0004-3.
Jylhävä J, Pedersen NL, Hägg S. Biological Age Predictors EBioMedicine. 2017;21:29–36. https://doi.org/10.1016/j.ebiom.2017.03.046.
Levine ME, Lu AT, Quach A, Chen BH, Assimes TL, Bandinelli S, et al. An epigenetic biomarker of aging for lifespan and healthspan. Aging. 2018;10(4):573–91. https://doi.org/10.18632/aging.101414.
Lu AT, Quach A, Wilson JG, Reiner AP, Aviv A, Raj K, et al. DNA methylation GrimAge strongly predicts lifespan and healthspan. Aging. 2019;11(2):303–27. https://doi.org/10.18632/aging.101684.
Belsky DW, Caspi A, Corcoran DL, Sugden K, Poulton R, Arseneault L, et al. DunedinPACE, a DNA methylation biomarker of the pace of aging. eLife. 2022;11:e73420 %U https://elifesciences.org/articles/. https://doi.org/10.7554/eLife.73420.
Lu AT, Binder AM, Zhang J, Yan Q, Reiner AP, Cox SR, et al. DNA methylation GrimAge version 2. Aging (Albany NY). 2022;14(23):9484–549. https://doi.org/10.18632/aging.204434.
Stephan Y, Sutin AR, Luchetti MAO, Terracciano A. An older subjective age is related to accelerated epigenetic aging. Psychol Aging. 2021;36(6):767–72. https://doi.org/10.1037/pag0000607.
Faul JD, Kim JK, Levine ME, Thyagarajan B, Weir DR, Crimmins EM. Epigenetic-based age acceleration in a representative sample of older Americans: Associations with aging-related morbidity and mortality. Proc Natl Acad Sci USA. 2023;120(9):e2215840120. https://doi.org/10.1073/pnas.2215840120.
Fransquet PD, Wrigglesworth J, Woods RL, Ernst ME, Ryan J. The epigenetic clock as a predictor of disease and mortality risk: a systematic review and meta-analysis. Clin Epigenetics. 2019;11:1868–7083. https://doi.org/10.1186/s13148-019-0656-7.
Milne RL, Fletcher AS, MacInnis RJ, Hodge AM, Hopkins AH, Bassett JK, et al. Cohort Profile: The Melbourne Collaborative Cohort Study (Health 2020). International Journal of Epidemiology. 2017;46(6):1757-i %U http://academic.oup.com/ije/article/46/6//3882696. https://doi.org/10.1093/ije/dyx085
Dugué P-A, English DR, MacInnis RJ, Jung C-H, Bassett JK, FitzGerald LM, et al. Reliability of DNA methylation measures from dried blood spots and mononuclear cells using the HumanMethylation450k BeadArray. Sci Rep. 2016;6(1):30317. https://doi.org/10.1038/srep30317.
Dugué PA, Wilson R, Lehne B, Jayasekara H, Wang X, Jung CH, et al. Alcohol consumption is associated with widespread changes in blood DNA methylation: Analysis of cross‐sectional and longitudinal data. Addiction Biology. 2021;26(1). https://doi.org/10.1111/adb.12855.
Joo JE, Wong EM, Baglietto L, Jung C-H, Tsimiklis H, Park DJ, et al. The use of DNA from archival dried blood spots with the Infinium HumanMethylation450 array. BMC Biotechnol. 2013;13(1):23. https://doi.org/10.1186/1472-6750-13-23.
Ware J Jr, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–33. https://doi.org/10.1097/00005650-199603000-00003.
Higgins-Chen AT, Thrush KL, Wang Y, Minteer CJ, Kuo P-L, Wang M, et al. A computational solution for bolstering reliability of epigenetic clocks: implications for clinical trials and longitudinal tracking. Nature Aging. 2022;2(7):644–61. https://doi.org/10.1038/s43587-022-00248-2.
Berryman C, McAuley JH, Moseley LG. Sphere 12 Screening Questionnaire. J Physiother. 2012;58(4):273. https://doi.org/10.1016/S1836-9553(12)70133-9.
Kaplan GA, Goldberg DE, Everson SA, Cohen RD, Salonen R, Tuomilehto J, et al. Perceived health status and morbidity and mortality: evidence from the Kuopio Ischaemic Heart Disease Risk Factor Study. Int J Epidemiol. 1996;25(2):259–65. https://doi.org/10.1093/ije/25.2.259.
Feng Q, Zhu H, Zhen Z, Gu D. Self-rated health, interviewer-rated health, and their predictive powers on mortality in old age. J Gerontol B Psychol Sci Soc Sci. 2016;71(3):538–50. https://doi.org/10.1093/geronb/gbu186.
Marioni RE, Harris SE, Shah S, McRae AF, von Zglinicki T, Martin-Ruiz C, et al. The epigenetic clock and telomere length are independently associated with chronological age and mortality. Int J Epidemiol. 2016;45(2):424–32. https://doi.org/10.1093/ije/dyw041.
Cribb L, Hodge AM, Yu C, Li SX, English DR, Makalic E, et al. Inflammation and epigenetic aging are largely independent markers of biological aging and mortality. The Journals of Gerontology: Series A. 2022;77(12):2378–86 %U https://academic.oup.com/biomedgerontology/article/77/12//6655953. https://doi.org/10.1093/gerona/glac147.
Li X, Ploner A, Wang Y, Magnusson PKE, Reynolds C, Finkel D, et al. Longitudinal trajectories, correlations and mortality associations of nine biological ages across 20-years follow-up. eLife. 2020;9:e51507. https://doi.org/10.7554/eLife.51507.
Li DL, Hodge AM, Cribb L, Southey MC, Giles GG, Milne RL, et al. Body size, diet quality, and epigenetic aging: cross-sectional and longitudinal analyses. J Gerontol: Ser. 2024;79(4):glae026. https://doi.org/10.1093/gerona/glae026.
Dugué P-A, Bassett JK, Wong EM, Joo JE, Li S, Yu C, et al. Biological aging measures based on blood DNA methylation and risk of cancer: a prospective study. JNCI Cancer Spectr. 2021;5(1):pkaa109. https://doi.org/10.1093/jncics/pkaa109.
Waziry R, Ryan CP, Corcoran DL, Huffman KM, Kobor MS, Kothari M, et al. Effect of long-term caloric restriction on DNA methylation measures of biological aging in healthy adults from the CALERIE trial. Nature Aging. 2023;3(3):248–57. https://doi.org/10.1038/s43587-022-00357-y.
Giles GG, English DR. The Melbourne Collaborative Cohort Study. IARC Sci Publ. 2002;156:69–70.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions Melbourne Collaborative Cohort Study (MCCS) cohort recruitment was funded by VicHealth and Cancer Council Victoria. The MCCS was further supported by Australian National Health and Medical Research Council (NHMRC) grants 209057, 396414, and 1074383 and by infrastructure provided by Cancer Council Victoria. The nested case–control methylation studies were supported by the NHMRC Grants 1011618, 1026892,1027505, 1050198, 1043616, and 1074383. The longitudinal methylation study was supported by the NHMRC grants 1088405 and 1106016. MCS is a recipient of a NHMRC L3 Investigator Fellowship (GNT2017325).
Author information
Authors and Affiliations
Contributions
DLL, AMH, and PAD designed the study; DLL and PAD conducted statistical analyses; MCS, GGG, and RLM acquired funding and provided resources; DLL and PAD drafted the first version of the manuscript; all authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Li, D.L., Hodge, A.M., Southey, M.C. et al. Self-rated health, epigenetic ageing, and long-term mortality in older Australians. GeroScience (2024). https://doi.org/10.1007/s11357-024-01211-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11357-024-01211-2