Abstract
Lithium is an established first-line treatment for bipolar disorder. Beyond its therapeutic effect as a mood stabiliser, lithium exhibits potential anti-ageing effects. This study aimed to examine the relationship between the duration of lithium use, biological ageing and mortality. The UK Biobank is an observational study of middle-aged and older adults. We tested associations between the duration of lithium use (number of prescriptions, total duration of use and duration of the first prescription period) and telomere length, frailty, metabolomic age (MileAge) delta, pulse rate and all-cause mortality. Five hundred ninety-one individuals (mean age = 57.49 years; 55% females) had been prescribed lithium. There was no evidence that the number of prescriptions (β = − 0.022, 95% CI − 0.081 to 0.037, p = 0.47), the total duration of use (β = − 0.005, 95% CI − 0.023 to 0.013, p = 0.57) or the duration of the first prescription period (β = − 0.018, 95% CI − 0.051 to 0.015, p = 0.29) correlated with telomere length. There was also no evidence that the duration of lithium use correlated with frailty or MileAge delta. However, a higher prescription count and a longer duration of use was associated with a lower pulse rate. The duration of lithium use did not predict all-cause mortality. We observed no evidence of associations between the duration of lithium use and biological ageing markers, including telomere length. Our findings suggest that the potential anti-ageing effects of lithium do not differ by the duration of use.
Similar content being viewed by others
Introduction
Lithium is considered the gold standard treatment for patients with bipolar disorder who experience recurrent episodes of (hypo)mania and depression [1]. Lithium is also used to augment antidepressant medication, for example in patients with difficult-to-treat major depressive disorder [2]. While the evidence supports lithium’s therapeutic effects [3], its mechanisms of action are incompletely understood. Studies indicate that lithium influences neurotransmitter signalling and acts on second messenger systems including the adenyl cyclase and protein kinase A pathways [4].
Beyond its therapeutic effects as a mood stabiliser, multiple lines of evidence suggest that lithium may impact biological ageing and longevity [5]. For example, mitochondrial dysfunction is a hallmark of ageing [6], and lithium treatment has been shown to enhance mitochondrial metabolism by increasing the activity of electron transport complexes [7, 8]. Preclinical and clinical studies suggest that lithium can reduce oxidative stress, which is linked to several age-related diseases [9, 10]. Notably, studies have demonstrated that lithium extends the lifespan of model organisms, including Caenorhabditis elegans (“C. elegans”) and Drosophila [11, 12].
A focus of research on lithium’s potential anti-ageing properties has been to examine its link with telomere length. Telomeres, which are repetitive nucleoprotein complexes at the ends of chromosomes, progressively shorten with cell division and play an important role in maintaining genomic stability. Telomere attrition is a hallmark of ageing and is linked to cellular senescence [6]. Telomere dysfunction plays a role in many human diseases [13]. For example, meta-analyses suggest that individuals with bipolar disorder have shorter telomeres than healthy controls [14,15,16]. However, several studies have found no evidence of a difference in telomere length or observed longer telomeres in patients with bipolar disorder. These inconsistencies may in part result from differences in lithium treatment. Some clinical studies suggest that lithium protects against telomere attrition. Indeed, studies have shown that bipolar disorder patients treated with lithium had longer telomeres than healthy controls [17] and that lithium-treated patients had longer telomeres than patients who were not treated with lithium [17, 18]. While these group differences in telomere length could be due to other factors, several studies found that a longer duration of lithium treatment correlated with longer telomeres [19].
Building on studies in the UK Biobank that have identified predictors and correlates of telomere length [20,21,22], we examined the potential impact of the duration of lithium treatment on telomere length and other markers of biological ageing. We defined three measures of lithium treatment duration using primary care prescription records and assessed multiple markers of biological ageing and longevity, including telomere length, frailty, metabolomic age (MileAge) delta and all-cause mortality. The overall aim was to elucidate the broader implications of lithium treatment on biological ageing.
Methods
Study population
The UK Biobank is a prospective community-based study that recruited over 500,000 middle-aged and older adults, aged 40 to 69 years [23]. Individuals who were registered with the UK National Health Service (NHS) and lived within a 25-mi (~ 40 km) radius of one of 22 assessment centres were invited to participate. At the baseline assessment, which took place between 2006 and 2010, participants reported their sociodemographic characteristics, health behaviours and medical history. They also underwent physical examinations and had blood and urine samples taken. Data linkage to primary care health records is available for about 230,000 participants.
Duration of lithium use
The duration of lithium use was derived from medication prescriptions recorded by general practitioner practices as part of routine patient care. These data included prescriptions recorded between July 1945 and September 2017 and were available for 222,073 participants. Lithium prescriptions were identified using a combination of the British National Formulary (BNF), Read v2 and Dictionary of Medicines and Devices (dm + d) codes and by searching for relevant string permutations across the prescription medication names. The duration of lithium use was defined in three ways, similar to a previous study on antidepressants [24]. First, we calculated the total number of lithium prescriptions across all primary care prescription records. Second, we calculated the total number of weeks across all prescription windows, which we defined as periods of less than 90 days between consecutive prescriptions. Third, we calculated the number of weeks of the first prescription window. Prescriptions after the baseline assessment date were excluded from these calculations.
Telomere length
Leukocyte telomere length was measured using a quantitative polymerase chain reaction (PCR) assay that expresses telomere length as the ratio of the telomere repeat copy number (T) relative to a single-copy gene (S) that encodes haemoglobin subunit beta [25]. The T/S ratio is proportional to an individual’s average telomere length [26]. Measurements were adjusted for operational and technical parameters (PCR machine, staff member, enzyme batch, primer batch, temperature, humidity, primer batch × PCR machine, primer batch × staff member, A260/A280 ratio of the DNA sample and A260/A280 ratio squared), loge transformed and Z-standardised.
Frailty Index
A frailty Index was derived from health deficits that met the following criteria: indicators of poor health, more prevalent in older individuals, neither rare nor universal, covering multiple areas of functioning and available for ≥ 80% of participants [27]. The index included 49 variables ascertained via touch-screen questionnaires and nurse-led interviews, including cardiometabolic, cranial, immunological, musculoskeletal, respiratory and sensory traits, well-being, infirmity, cancer and pain. Categorical variables were dichotomised (no deficit = 0; deficit = 1), and ordinal variables were mapped onto a score between 0 and 1. The sum of deficits was divided by the total number of possible deficits, resulting in frailty Index scores between 0 and 1, with higher scores indicating greater levels of frailty [28]. Participants with missing data for ≥ 10/49 variables were excluded [27].
Metabolomic age (MileAge) delta
Nuclear magnetic resonance (NMR) spectroscopy–derived metabolomic biomarkers were quantified in non-fasting plasma samples using the Nightingale Health platform, which ascertains 168 circulating metabolites using a high-throughput standardised protocol [29]. In 101,359 participants, we developed a metabolomic ageing clock using a Cubist rule–based regression model [30]. This algorithm is an ensemble technique that derives rules from decision trees and fits linear regression models in the subsets of data defined by these rules. The model incorporates boosting techniques and may adjust predictions based on k-nearest neighbours [31, 32]. Model performance was assessed using nested cross-validation with 10 outer loops and 5 inner folds for hyperparameter tuning. The cross-validation mean absolute error (MAE) was 5.42 years. Metabolomic age (MileAge) delta represents the difference between predicted and chronological age, with positive and negative values indicating accelerated and decelerated biological ageing, respectively [30].
Pulse rate
Resting pulse rate in beats per minute was recorded using an Omron 705 IT digital blood pressure monitor device or, exceptionally, a manual sphygmomanometer. We calculated the average of the two available readings to reduce potential measurement error.
All-cause mortality
The date of death was obtained through linkage with national death registries: NHS Digital (England and Wales) and the NHS Central Register (Scotland). The censoring date was 30 November 2022. The most recent death was recorded on 19 December 2022, although the data were incomplete for December 2022.
Covariates
Covariates for the cross-sectional and prospective analyses were identified from prior studies and domain knowledge. They included chronological age, sex, body mass index (kg/m2), morbidity count (none/one, two, three, four or five +), gross annual household income (< £18,000, £18,000–£30,999, £31,000–£51,999 or £52,000–£100,000/ > £100,000), highest educational/professional qualification (none, O levels/GCSEs/CSEs, A levels/NVQ/HND/HNC or degree) and cohabitation status (single or with spouse/partner). A directed acyclic graph (DAG) of the relationships between the duration of lithium use, telomere length and selected confounders is shown in Figure S1.
Statistical analyses
The data processing and analyses were performed in R (version 4.2). Sample characteristics were summarised using means and standard deviations or counts and percentages. Associations between the duration of lithium use (number of prescriptions, total duration of use and duration of the first prescription period) and telomere length were estimated using ordinary least squares regression. We further tested associations between the duration of lithium use and two other indicators of biological age (the frailty Index and MileAge delta) and pulse rate. Hazard ratios (HRs) and 95% confidence intervals were estimated using Cox proportional hazards models to examine associations between the duration of lithium use and all-cause mortality. We examined both quintiles of the distribution, with the lowest quintile as the reference group, and spline functions of the distribution with the median as reference value. Age in years was used as the underlying time axis, with age 40 as the start of follow-up. The cross-sectional and prospective analyses were adjusted for chronological age and sex (model 1) and chronological age, sex, body mass index, morbidity count, household income, highest qualification and cohabitation status (model 2).
Sensitivity analyses
We conducted two sensitivity analyses of the duration of lithium use and biological ageing. First, we restricted the sample to individuals with a total duration of lithium use of (a) at least 1 year (52 weeks) or (b) at least 4.5 years (234 weeks) because of prior research identifying an association between the duration of lithium use and telomere length only in chronic lithium users [19]. Second, we additionally adjusted for current antidepressant medication use (yes/no) at the time of the baseline assessment because of prior evidence that antidepressant medication use may be associated with shorter telomeres [20, 33, 34], though not all studies support this finding [35, 36]. We did not adjust for the duration of antidepressant use because previous studies found no evidence that telomere length differed between individuals who had been on antidepressant medications for periods shorter or longer than 6 months [37] or that telomere length was associated with the lifetime duration of antidepressant use [38].
Results
Sample characteristics
Of the 502,476 participants in the UK Biobank, 222,073 individuals (about 44.2% of the sample) had prescription data available through their linked primary care records. Of the 773 participants with a lithium prescription in their primary care record, n = 182 were excluded because their first prescription followed the baseline assessment. The duration of lithium use was estimated for 591 participants (Figure S2). Sample characteristics are shown in Table 1. Based on our previously reported criteria [39, 40], 71.74% of participants had a lifetime history of mood disorders (n = 248 had bipolar disorder and n = 176 had depression).
Duration of lithium use and telomere length
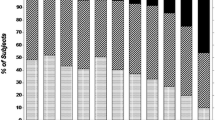
In the model adjusted for chronological age and sex, there was no evidence that the number of lithium prescriptions (N = 569, β = − 0.022, 95% CI − 0.081 to 0.037, p = 0.47), the total duration of use (N = 569, β = − 0.005, 95% CI − 0.023 to 0.013, p = 0.57) or the duration of the first prescription period (N = 569, β = − 0.018, 95% CI − 0.051 to 0.015, p = 0.29) were associated with telomere length. Additional adjustments for body mass index, morbidity count, household income, highest qualification and cohabitation status had no discernible impact on these results (Table 2). Individuals with a higher prescription count or longer duration of lithium use were more likely to use lithium at the time of the baseline assessment (Fig. 1).
Scatter plots of telomere length (T/S ratio loge transformed and Z-standardised) by lithium prescription count, total duration of use and duration of the first prescription period. The lines were estimated using ordinary least squares regression, and the shaded areas correspond to 95% confidence intervals. Lithium use (yes/no) at the time of the baseline assessment when telomere length was measured is shown in different colours. Individuals without baseline data on current lithium use are not shown. Tx = treatment; Rx = prescription
Duration of lithium use, frailty and metabolomic age (MileAge) delta
There was no evidence that the duration of lithium use was associated with the frailty Index (N = 585, β = − 0.012, 95% CI − 0.030 to 0.006, p = 0.21) or MileAge delta (N = 120, β = 0.030, 95% CI − 0.133 to 0.194, p = 0.72) (Fig. 2). This finding was consistent across all measures of the duration of lithium use and adjustment for additional covariates (Table 2).
Scatter plots of telomere length (T/S ratio loge transformed and Z-standardised), the frailty Index and metabolomic age (MileAge) delta by total duration of lithium use. The lines were estimated using ordinary least squares regression, and the shaded areas correspond to 95% confidence intervals. tx = treatment
Duration of lithium use and pulse rate
To ensure that the lack of statistically significant associations was not due to how we defined the duration of lithium use, we further tested associations between the duration of lithium use and pulse rate (Figure S3). The number of lithium prescriptions (N = 586, β = − 0.061, 95% CI − 0.119 to − 0.002, p = 0.04) and the total duration of lithium use (N = 586, β = − 0.026, 95% CI − 0.044 to − 0.008, p = 0.005) were both associated with a lower pulse rate (Table 2).
Duration of lithium use and all-cause mortality
The median duration of follow-up of censored individuals was 13.71 years (IQR = 1.35 years), with more than 7686 person-years of follow-up. During this period, 94 deaths were observed. There was no evidence that the duration of lithium use predicted all-cause mortality (Table 3). Comparing individuals in the second to fifth quintile of the distribution of the duration of lithium use to individuals in the first quintile resulted in no statistically significant differences in all-cause mortality (lowest p = 0.08) (Fig. 3).
Hazard ratios (HR) and 95% confidence intervals from Cox proportional hazards models for all-cause mortality. Age (in years) was used as the underlying time axis. The model was adjusted for age and sex. Reference group: individuals in the lowest quintile of the distribution of the duration of lithium use (prescription count, total duration and duration of the first prescription period). Tx = treatment; Rx = prescription
Modelling the mortality hazard as a spline function of the duration of lithium use, instead of by quintiles of the distribution, provided little evidence of a statistically significant association between the duration of lithium use and all-cause mortality (Fig. 4 and Figure S4). There was, however, some evidence that prescription counts greater than about 300 were associated with a higher mortality risk.
Sensitivity analyses
Excluding participants with a total duration of lithium use of less than 1 year or less than 4.5 years provided little evidence that the duration of lithium use was associated with biological ageing (Table S1 and Table S2). There was some evidence that a longer duration of the first lithium prescription period was associated with a higher MileAge delta, although this finding did not survive multiple testing corrections in the fully adjusted model. The duration of lithium use was not associated with pulse rate in these analyses.
The relationship between telomere length and the duration of lithium use stratified by current antidepressant use at the time of the baseline assessment is shown in Figure S5. Additional adjustments for current antidepressant use had no discernible impact on the analyses of the relationship between the duration of lithium use and biological ageing (Table S3). However, the association between a higher prescription count and a longer total duration of lithium use and pulse rate was stronger in these analyses.
Discussion
We examined the relationship between the duration of lithium use and multiple markers of biological ageing, including telomere length, frailty, metabolomic age (MileAge) delta and all-cause mortality. Both cross-sectional and prospective analyses provided little evidence of an association between the duration of lithium use and biological ageing or mortality.
Our findings are inconsistent with most prior studies of the duration of lithium use and telomere length, several of which identified a positive association between lithium and telomere length. Martinsson et al. found that lithium-treated bipolar disorder patients had on average 35% longer telomeres than healthy controls [17]. In the same study, the duration of lithium treatment was positively correlated with telomere length, particularly in patients who had been treated for more than 2.5 years. Pisanu et al. [41] and Coutts et al. [19] corroborated these observations, identifying statistically significant associations between chronic lithium treatment and telomere length in patients with bipolar disorder. Squassina et al. also reported a positive correlation between the duration of lithium use and telomere length in 150 bipolar disorder patients who had been treated for more than 2 years [42]. A mechanistic in vitro study provided further evidence supporting lithium’s putative effect on telomeres by demonstrating that lithium administration to lymphoblastoid cell lines from bipolar disorder patients increased telomere length [18]. Nevertheless, there is some precedent for our findings. Ferensztajn-Rochowiak et al. reported that in a sample of 41 patients with bipolar disorder, the duration of lithium treatment did not correlate with telomere length in peripheral blood leukocytes [43]. Another in vitro study found that the administration of lithium to lymphoblastoid cell lines from bipolar disorder patients had no effect on telomere length [44], though it is worth noting that these patients had previously been treated with lithium.
There are several potential explanations for the observed differences between our findings and those of prior studies. For example, most clinical studies determined the duration of lithium treatment retrospectively during the study visit, while we derived the duration of lithium use in our study from prescription records. Furthermore, there is some evidence that clinical factors such as bipolar disorder diagnosis, number of episodes, chronicity and severity of illness impact telomere length. The participants in our study likely represent a healthier subset of the population than the patients included in prior clinical studies. Moreover, genetic factors can moderate the effect of lithium on telomere length [19]. Although we adjusted for several confounders in our analyses, we also found little evidence of any statistical associations in the model adjusted only for chronological age and sex. The sample size of our study (n = 569) is one of the largest in the field, and we used three definitions of the duration of lithium use to increase the robustness of our findings. In addition, we conducted a sensitivity analysis of pulse rate, which we expected to be negatively correlated with the duration of lithium use [45]. The observed correlation between the duration of lithium use and a lower pulse rate supports the validity of our measures of the duration of lithium use.
There has been little prior research on the relationship between lithium use and the other biological ageing markers explored in this study. Okazaki et al. found that bipolar disorder patients who were taking mood stabilisers had a younger epigenetic age, according to Horvath’s epigenetic ageing clock, than patients who were not taking mood stabilisers [46]. However, an in vitro study of lymphoblastoid cell lines did not find that administration of lithium impacted the Horvath clock [18]. We found no evidence of an association between the duration of lithium use and metabolomic age (MileAge) delta in our study. However, it is worth noting that epigenetic and metabolomic age may not strongly correlate [47]. We also explored the relationship between the duration of lithium use and frailty, which is a measure of age-related health deficit accumulation. While some evidence suggests that frailty and telomere length are not strongly linked [48], frailty is a key marker of biological ageing and physical ill-health [49, 50]. Our study provided no evidence of a statistically significant association between the duration of lithium use and frailty. Taken together, these findings suggest that the lack of association between the duration of lithium use and biological ageing—at least in our sample—was not specific to telomere length.
The duration of lithium use was not linked to all-cause mortality in our study. Multiple observational studies have previously shown that lithium use is associated with a lower mortality risk. For example, a cohort study of 826 patients in Finland found that lithium treatment, compared to no lithium treatment, was associated with a lower all-cause mortality risk [51]. Another cohort study in Taiwan found that lithium was associated with the lowest all-cause mortality risk in bipolar disorder patients, relative to other mood stabiliser treatments [52]. A recent study in the UK Biobank found that lithium treatment was associated with a lower all-cause mortality risk than treatment with antipsychotics [53]. However, it is important to note that we examined the duration of lithium use, not whether patients were treated versus not treated with lithium, which prior studies examined. As such, our findings suggest that there may not be a link between longer duration of lithium use and all-cause mortality in a community-based, real-world sample. These findings do not imply that lithium use (yes/no) is not linked to all-cause mortality, and they do not invalidate findings from clinical trials where lithium adherence is more controlled.
Limitations
We acknowledge certain limitations to our study. The UK Biobank primarily recruited individuals between the ages of 40 and 69 years, limiting the conclusions drawn from our findings to middle-aged and older adults. There is evidence of a healthy volunteer participation bias in the UK Biobank [54, 55], which could mean that the participants in our study were healthier than the patients included in prior clinical studies. The observational nature of our study precludes any causal inferences, and residual confounding factors may exist despite our efforts to account for relevant covariates. The duration of lithium use was derived from primary care prescription records. Prescriptions may not perfectly reflect medication use, and there is some evidence that, despite the need for regular blood tests, adherence to lithium is poor in clinical practice [56]; furthermore, prescription dates are a proxy of date of use. Nonetheless, we derived and tested three different definitions of the duration of lithium use to be as robust as possible within these constraints. Telomere length was measured using leukocyte DNA, and findings might differ from telomere length measured in other tissues. However, prior evidence suggests that leukocyte telomere length correlates well with telomere length in other tissues [57]. Finally, we could only examine average telomere length and were unable to evaluate whether the duration of lithium use was associated with variability in telomere length, which may be more important for telomere dysfunction and biological ageing [26].
Conclusion
Our findings, in a larger sample, challenge prior research on the relationship between the duration of lithium use and telomere length. Given that we also did not observe statistically significant associations with other biological ageing markers such as frailty and metabolomic age (MileAge) delta, nor with all-cause mortality, our findings suggest that the potential anti-ageing effects of lithium do not differ by the duration of use. Our findings encourage further scientific inquiry into the complex interplay between lithium medication, biological ageing and lifespan.
Data availability
UK Biobank data used are available to all bona fide researchers for health-related research that is in the public interest, subject to an application process and approval criteria. Study materials are publicly available online at http://www.ukbiobank.ac.uk.
References
National Institute for Health Care Excellence. Bipolar disorder: assessment and management. 2020. Retrieved on 11 December 2023, from https://www.nice.org.uk/guidance/cg185.
Cleare A, Pariante C, Young A, Anderson I, Christmas D, Cowen P, Dickens C, Ferrier I, Geddes J, Gilbody S, Haddad P, Katona C, Lewis G, et al. Evidence-based guidelines for treating depressive disorders with antidepressants: a revision of the 2008 British Association for Psychopharmacology guidelines. J Psychopharmacol. 2015;29:459–525.
Gadelrab R, Hampsey E, Strawbridge R, Taylor RH, Ulrichsen A, Young AH. Comparing measurements of lithium treatment efficacy in people with bipolar disorder: systematic review and meta-analysis. BJPsych Open. 2023;9: e98.
Malhi GS, Tanious M, Das P, Coulston CM, Berk M. Potential mechanisms of action of lithium in bipolar disorder. CNS Drugs. 2013;27:135–53.
Salarda EM, Zhao NO, Lima CNNC, Fries GR. Mini-review: the anti-aging effects of lithium in bipolar disorder. Neurosci Lett. 2021;759:136051.
López-Otín C, Blasco MA, Partridge L, Serrano M, Kroemer G. Hallmarks of aging: an expanding universe. Cell. 2023;186:243–78.
Maurer IC, Schippel P, Volz H-P. Lithium-induced enhancement of mitochondrial oxidative phosphorylation in human brain tissue. Bipolar Disord. 2009;11:515–22.
de Sousa RT, Streck EL, Zanetti MV, Ferreira GK, Diniz BS, Brunoni AR, Busatto GF, Gattaz WF, Machado-Vieira R. Lithium increases leukocyte mitochondrial complex I activity in bipolar disorder during depressive episodes. Psychopharmacology. 2015;232:245–50.
Machado-Vieira R, Andreazza AC, Viale CI, Zanatto V, Cereser V, Vargas RdS, Kapczinski F, Portela LV, Souza DO, Salvador M, Gentil V. Oxidative stress parameters in unmedicated and treated bipolar subjects during initial manic episode: a possible role for lithium antioxidant effects. Neurosci Lett. 2007;421:33–6.
Khairova R, Pawar R, Salvadore G, Juruena MF, de Sousa RT, Soeiro-de-Souza MG, Salvador M, Zarate CA, Gattaz WF, Machado-Vieira R. Effects of lithium on oxidative stress parameters in healthy subjects. Mol Med Rep. 2012;5:680–2.
McColl G, Killilea DW, Hubbard AE, Vantipalli MC, Melov S, Lithgow GJ. Pharmacogenetic analysis of lithium-induced delayed aging in Caenorhabditis elegans. J Biol Chem. 2008;283:350–7.
Castillo-Quan Jorge I, Li L, Kinghorn Kerri J, Ivanov Dobril K, Tain Luke S, Slack C, Kerr F, Nespital T, Thornton J, Hardy J, Bjedov I, Partridge L. Lithium promotes longevity through GSK3/NRF2-dependent hormesis. Cell Rep. 2016;15:638–50.
Rossiello F, Jurk D, Passos JF, d’Adda di Fagagna F. Telomere dysfunction in ageing and age-related diseases. Nat Cell Biol. 2022;24:135–47.
Colpo GD, Leffa DD, Köhler CA, Kapczinski F, Quevedo J, Carvalho AF. Is bipolar disorder associated with accelerating aging? A meta-analysis of telomere length studies. J Affect Disord. 2015;186:241–8.
Darrow SM, Verhoeven JE, Révész D, Lindqvist D, Penninx BWJH, Delucchi KL, Wolkowitz OM, Mathews CA. The association between psychiatric disorders and telomere length: a meta-analysis involving 14,827 persons. Psychosom Med. 2016;78:776–87.
Huang Y-C, Wang L-J, Tseng P-T, Hung C-F, Lin P-Y. Leukocyte telomere length in patients with bipolar disorder: an updated meta-analysis and subgroup analysis by mood status. Psychiatry Res. 2018;270:41–9.
Martinsson L, Wei Y, Xu D, Melas PA, Mathé AA, Schalling M, Lavebratt C, Backlund L. Long-term lithium treatment in bipolar disorder is associated with longer leukocyte telomeres. Transl Psychiatr. 2013;3:e261-e.
Fries GR, Zamzow MJ, Colpo GD, Monroy-Jaramillo N, Quevedo J, Arnold JG, Bowden CL, Walss-Bass C. The anti-aging effects of lithium in lymphoblastoid cell lines from patients with bipolar disorder and controls. J Psychiatr Res. 2020;128:38–42.
Coutts F, Palmos AB, Duarte RRR, de Jong S, Lewis CM, Dima D, Powell TR. The polygenic nature of telomere length and the anti-ageing properties of lithium. Neuropsychopharmacology. 2019;44:757–65.
Mutz J, Lewis CM. Telomere length associations with clinical diagnosis, age, and polygenic risk scores for anxiety disorder, depression, and bipolar disorder. Biol Psychiatr Glob Open Sci. 2023;3:1012–20.
Bountziouka V, Musicha C, Allara E, Kaptoge S, Wang Q, Angelantonio ED, Butterworth AS, Thompson JR, Danesh JN, Wood AM, Nelson CP, Codd V, Samani NJ. Modifiable traits, healthy behaviours, and leukocyte telomere length: a population-based study in UK Biobank. Lancet Healthy Longev. 2022;3:e321–31.
Luo S, Wong ICK, Chui CSL, Zheng J, Huang Y, Schooling CM, Yeung SLA. Effects of putative metformin targets on phenotypic age and leukocyte telomere length: a mendelian randomisation study using data from the UK Biobank. Lancet Healthy Longev. 2023;4:e337–44.
Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, Motyer A, Vukcevic D, Delaneau O, O’Connell J, Cortes A, Welsh S, Young A, et al. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018;562:203–9.
Wong WL, Fabbri C, Laplace B, Li D, van Westrhenen R, Lewis CM, Dawe GS, Young AH. The effects of CYP2C19 genotype on proxies of SSRI antidepressant response in the UK Biobank. Pharmaceuticals. 2023;16(9).
Codd V, Denniff M, Swinfield C, Warner SC, Papakonstantinou M, Sheth S, Nanus DE, Budgeon CA, Musicha C, Bountziouka V, Wang Q, Bramley R, Allara E, et al. Measurement and initial characterization of leukocyte telomere length in 474,074 participants in UK Biobank. Nature Aging. 2022;2:170–9.
Lai T-P, Wright WE, Shay JW. Comparison of telomere length measurement methods. Philos Trans Royal Soc B: Biol Sci. 2018;373:20160451.
Williams DM, Jylhävä J, Pedersen NL, Hägg S. A Frailty index for UK biobank participants. J Gerontol: Ser A. 2018;74:582–7.
Mutz J, Choudhury U, Zhao J, Dregan A. Frailty in individuals with depression, bipolar disorder and anxiety disorders: longitudinal analyses of all-cause mortality. BMC Med. 2022;20:274.
Würtz P, Kangas AJ, Soininen P, Lawlor DA, Davey Smith G, Ala-Korpela M. Quantitative serum nuclear magnetic resonance metabolomics in large-scale epidemiology: a primer on -omic technologies. Am J Epidemiol. 2017;186:1084–96.
Mutz J, Iniesta R, Lewis CM. Metabolomic Age (MileAge) predicts health and lifespan: a comparison of multiple machine learning algorithms. medRxiv. 2024. https://doi.org/10.1101/2024.02.10.24302617.
Quinlan JR. Learning with continuous classes. 5th Australian joint conference on artificial intelligence: World Scientific, pp 343–8. 1992.
Kuhn M, Johnson K. Regression trees and rule-based models. In: Kuhn M, Johnson K, editors. Applied predictive modeling. New York, NY: Springer, New York; 2013. p. 173–220.
Palmos AB, Breen G, Goodwin L, Frissa S, Hatch SL, Hotopf M, Thuret S, Lewis CM, Powell TR. Genetic risk for psychiatric disorders and telomere length. Front Genet. 2018; 9.
Needham BL, Mezuk B, Bareis N, Lin J, Blackburn EH, Epel ES. Depression, anxiety and telomere length in young adults: evidence from the National Health and Nutrition Examination Survey. Mol Psychiatry. 2015;20:520–8.
Verhoeven JE, Révész D, Picard M, Epel EE, Wolkowitz OM, Matthews KA, Penninx BWJH, Puterman E. Depression, telomeres and mitochondrial DNA: between- and within-person associations from a 10-year longitudinal study. Mol Psychiatry. 2018;23:850–7.
Powell TR, Dima D, Frangou S, Breen G. Telomere length and bipolar disorder. Neuropsychopharmacology. 2018;43:445–53.
Vance MC, Bui E, Hoeppner SS, Kovachy B, Prescott J, Mischoulon D, Walton ZE, Dong M, Nadal MF, Worthington JJ, Hoge EA, Cassano P, Orr EH, et al. Prospective association between major depressive disorder and leukocyte telomere length over two years. Psychoneuroendocrinology. 2018;90:157–64.
Pisanu C, Tsermpini EE, Skokou M, Kordou Z, Gourzis P, Assimakopoulos K, Congiu D, Meloni A, Balasopoulos D, Patrinos GP, Squassina A. Leukocyte telomere length is reduced in patients with major depressive disorder. Drug Dev Res. 2020;81:268–73.
Mutz J, Lewis CM. Lifetime depression and age-related changes in body composition, cardiovascular function, grip strength and lung function: sex-specific analyses in the UK Biobank. Aging. 2021;13:17038–79.
Mutz J, Young AH, Lewis CM. Age-related changes in physiology in individuals with bipolar disorder. J Affect Disord. 2022;296:157–68.
Pisanu C, Congiu D, Manchia M, Caria P, Cocco C, Dettori T, Frau DV, Manca E, Meloni A, Nieddu M, Noli B, Pinna F, Robledo R, et al. Differences in telomere length between patients with bipolar disorder and controls are influenced by lithium treatment. Pharmacogenomics. 2020;21:533–40.
Squassina A, Pisanu C, Congiu D, Caria P, Frau D, Niola P, Melis C, Baggiani G, Lopez JP, Cruceanu C, Turecki G, Severino G, Bocchetta A, et al. Leukocyte telomere length positively correlates with duration of lithium treatment in bipolar disorder patients. Eur Neuropsychopharmacol. 2016;26:1241–7.
Ferensztajn-Rochowiak E, Hołysz H, Kurczewska E, Lulkiewicz M, Rubiś B, Rybakowski F, Rybakowski JK. Decreased leucocyte telomere length in male patients with chronic bipolar disorder: lack of effect of long-term lithium treatment. Acta Neuropsychiatrica. 2021;33:299–306.
Squassina A, Meloni A, Congiu D, Bosganas P, Patrinos GP, Lin R, Turecki G, Severino G, Ardau R, Chillotti C, Pisanu C. Analysis on in vitro effect of lithium on telomere length in lymphoblastoid cell lines from bipolar disorder patients with different clinical response to long-term lithium treatment. Hum Genomics. 2022;16:45.
Mehta N, Vannozzi R. Lithium-induced electrocardiographic changes: a complete review. Clin Cardiol. 2017;40:1363–7.
Okazaki S, Numata S, Otsuka I, Horai T, Kinoshita M, Sora I, Ohmori T, Hishimoto A. Decelerated epigenetic aging associated with mood stabilizers in the blood of patients with bipolar disorder. Transl Psychiatry. 2020;10:129.
Robinson O, Chadeau Hyam M, Karaman I, Climaco Pinto R, Ala-Korpela M, Handakas E, Fiorito G, Gao H, Heard A, Jarvelin M-R, Lewis M, Pazoki R, Polidoro S, et al. Determinants of accelerated metabolomic and epigenetic aging in a UK cohort. Aging Cell. 2020;19:e13149.
Araújo Carvalho AC, Tavares Mendes ML, da Silva Reis MC, Santos VS, Tanajura DM, Martins-Filho PRS. Telomere length and frailty in older adults—a systematic review and meta-analysis. Ageing Res Rev. 2019;54:100914.
Ji L, Jazwinski SM, Kim S. Frailty and biological age. Ann Geriatr Med Res. 2021;25:141–9.
Mitnitski A, Collerton J, Martin-Ruiz C, Jagger C, von Zglinicki T, Rockwood K, Kirkwood TBL. Age-related frailty and its association with biological markers of ageing. BMC Med. 2015;13:161.
Toffol E, Hätönen T, Tanskanen A, Lönnqvist J, Wahlbeck K, Joffe G, Tiihonen J, Haukka J, Partonen T. Lithium is associated with decrease in all-cause and suicide mortality in high-risk bipolar patients: a nationwide registry-based prospective cohort study. J Affect Disord. 2015;183:159–65.
Chen P-H, Tsai S-Y, Chen P-Y, Pan C-H, Su S-S, Chen C-C, Kuo C-J. Mood stabilizers and risk of all-cause, natural, and suicide mortality in bipolar disorder: a nationwide cohort study. Acta Psychiatr Scand. 2023;147:234–47.
Araldi E, Jutzeler CR, Ristow M. Lithium treatment extends human lifespan: findings from the UK Biobank. Aging (Albany NY). 2023;15:421–40.
Fry A, Littlejohns TJ, Sudlow C, Doherty N, Adamska L, Sprosen T, Collins R, Allen NE. Comparison of sociodemographic and health-related characteristics of UK Biobank participants with those of the general population. Am J Epidemiol. 2017;186:1026–34.
Schoeler T, Speed D, Porcu E, Pirastu N, Pingault J-B, Kutalik Z. Participation bias in the UK Biobank distorts genetic associations and downstream analyses. Nat Hum Behav. 2023;7:1216–27.
Johnson R, McFarland B. Lithium use and discontinuation in a health maintenance organization. Am J Psychiatry. 1996;153:993–1000.
Demanelis K, Jasmine F, Chen LS, Chernoff M, Tong L, Delgado D, Zhang C, Shinkle J, Sabarinathan M, Lin H, Ramirez E, Oliva M, Kim-Hellmuth S, et al. Determinants of telomere length across human tissues. Science. 2020;369:eaaz6876.
Acknowledgements
This study was funded by the National Institute for Health and Care Research (NIHR) Maudsley Biomedical Research Centre at South London and Maudsley NHS Foundation Trust and King’s College London. The views expressed are those of the authors and not necessarily those of the NHS, the NIHR or the Department of Health and Social Care. WLEW is supported by the National University of Singapore President’s Graduate Fellowship. TRP is supported by the MRC (UKRI) as part of a New Investigator Research Grant (MR/W028018/1). GSD is supported by the Ministry of Education, Singapore, under its Academic Research Fund Tier 3 Award (MOE2017-T3-1-002). This research has been conducted using data from UK Biobank, a major biomedical database. Data access permission has been granted under UK Biobank application 45514. All analyses were supported by: King’s College London (2023). King’s Computational Research, Engineering and Technology Environment (CREATE). Retrieved May 24, 2023, from https://doi.org/10.18742/rnvf-m076
Author information
Authors and Affiliations
Contributions
JM conceived the idea of the study, acquired the data, carried out the statistical analysis, interpreted the findings and co-wrote the manuscript. WLEW identified the lithium medication codes, pre-processed the data to define the duration of lithium use, interpreted the findings and co-wrote the manuscript. TRP, AHY, GSD and CML interpreted the findings and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics
Ethical approval for the UK Biobank study has been granted by the National Information Governance Board for Health and Social Care and the NHS North West Multicentre Research Ethics Committee (11/NW/0382). No project-specific ethical approval is needed.
Competing interests
AHY declares the following: paid lectures and advisory boards for companies with drugs used in affective and related disorders (Flow Neuroscience, Novartis, Roche, Janssen, Takeda, Noema pharma, Compass, Astrazenaca, Boehringer Ingelheim, Eli Lilly, LivaNova, Lundbeck, Sunovion, Servier, Livanova, Janssen, Allegan, Bionomics, Sumitomo Dainippon Pharma, Sage and Neurocentrx); principal investigator in the Restore-Life VNS registry study funded by LivaNova; principal investigator on “ESKETINTRD3004: An Open-label, Long-term, Safety and Efficacy Study of Intranasal Esketamine in Treatment-resistant Depression”; principal investigator on “The Effects of Psilocybin on Cognitive Function in Healthy Participants”; principal investigator on “The Safety and Efficacy of Psilocybin in Participants with Treatment-Resistant Depression (P-TRD)”; principal investigator on “A Double-Blind, Randomized, Parallel-Group Study with Quetiapine Extended Release as Comparator to Evaluate the Efficacy and Safety of Seltorexant 20 mg as Adjunctive Therapy to Antidepressants in Adult and Elderly Patients with Major Depressive Disorder with Insomnia Symptoms Who Have Responded Inadequately to Antidepressant Therapy” (Janssen); principal investigator on “An Open-label, Long-term, Safety and Efficacy Study of Aticaprant as Adjunctive Therapy in Adult and Elderly Participants with Major Depressive Disorder (MDD)” (Janssen); principal investigator on “A Randomized, Double-blind, Multicentre, Parallel-group, Placebo-controlled Study to Evaluate the Efficacy, Safety, and Tolerability of Aticaprant 10 mg as Adjunctive Therapy in Adult Participants with Major Depressive Disorder (MDD) with Moderate-to-severe Anhedonia and Inadequate Response to Current Antidepressant Therapy”; principal investigator on “A Study of Disease Characteristics and Real-life Standard of Care Effectiveness in Patients with Major Depressive Disorder (MDD) With Anhedonia and Inadequate Response to Current Antidepressant Therapy Including an SSRI or SNR” (Janssen); UK chief investigator for Compass COMP006 & COMP007 studies; UK chief investigator for Novartis MDD study MIJ821A12201; grant funding (past and present) from NIMH (USA), CIHR (Canada), NARSAD (USA), Stanley Medical Research Institute (USA), MRC (UK), Wellcome Trust (UK), Royal College of Physicians (Edin), BMA (UK), UBC-VGH Foundation (Canada), WEDC (Canada), CCS Depression Research Fund (Canada), MSFHR (Canada), NIHR (UK), Janssen (UK) and EU Horizon 2020. No shareholdings in pharmaceutical companies. CML sits on the scientific advisory board for Myriad Neuroscience and has received speaker fees from SYNLAB and consultancy fees from UCB. JM, WLEW, TRP and GSD declare no financial conflict of interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Julian Mutz and Win Lee Edwin Wong contributed equally to this work and are designated as co-first authors.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Mutz, J., Wong, W.L.E., Powell, T.R. et al. The duration of lithium use and biological ageing: telomere length, frailty, metabolomic age and all-cause mortality. GeroScience (2024). https://doi.org/10.1007/s11357-024-01142-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s11357-024-01142-y