Abstract
Incense burning releases heavy particulate matter (PM) and nitrogen dioxide (NO2), known to have adverse effects on human health. Long-term exposure to PM and NO2 increases inflammatory cytokine levels and can induce respiratory diseases. This study examined the association between incense burning exposure and the health status, especially inflammatory biomarkers, of temple workers and volunteers in Taiwan. The longitudinal observational study compared adult temple workers and volunteers, with long-term incense burning exposure, to residents from outpatient clinics in the Chiayi area. Forced expiratory volume in 1 s (FEV1) and serum and exhaled breath condensate (EBC) cytokines were assessed. Nonparametric Mann-Whitney U tests were used to compare cytokine levels of the exposure and control groups during the cold and hot weather seasons. FEV1 was significantly more diminished in the exposed group than in the control group during the cold season. Exposure status was associated with greater hot-cold seasonal differences in serum interleukins (IL)-1β (regression coefficient (B) = 6.6, 95% confidence interval (CI) = 5.0 to 8.3, p < .001), IL17-A (B = 2.4, 95% CI = 0.3 to 4.5, p = .03), and plasminogen activator inhibitor [PAI]-1 (B = 5.4, 95% CI = 1.5 to 9.3, p = .009). After adjusting for confounders, the groups’ serum levels of IL-1β, IL-17A, and PAI-1 significantly differed. EBC cytokines did not show significant differences. Elevated levels of IL-1β, IL17-A, and PAI-1 have been associated with various autoinflammatory syndromes and diseases. Given the cultural significance of incense burning, culturally sensitive interventions, including education, policy development, and program implementation, are crucial to protect individuals’ health, especially temple workers, from the adverse effects of exposure, addressing the manufacture, importation, and sale of incense.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Avoid common mistakes on your manuscript.
Introduction
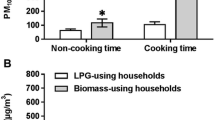
The burning of incense, a long-standing ritual in temples and homes for worship purposes, releases heavy air pollutants, such as particulate matter (PM10 and PM2.5) (Lin et al. 2008; Kuo et al. 2016), polycyclic aromatic hydrocarbons (PAHs), nitrogen dioxide (NO2), and other carcinogens, posing risks to human health (Lin et al. 2007; Liou et al. 2008; Yang et al. 2012; Shen et al. 2017). Studies in Taiwan have shown that burning incense can lead to high concentrations of PM2.5 (185–625 μg/m3) during certain events and inside temples, far exceeding recommended levels (Bootdee et al., 2016). In Taiwan, PM10 concentrations inside two temples (539 μg/m3 and 626 μg/m3, respectively) were 4 to 6 times those outside the temples (gates 148 μg/m3, street 121 μg/m3), and visitors were exposed to about 512 μg/m3 in the temples during worshipping dates (Lung and Kao 2003). Another study also indicated that PM1 concentrations (120.3 ± 48.8 μg/m3) and PM2.5 concentrations (149.9 ± 59.6 μg/m3) on event days were higher than those non-event days (PM1, 62.8 ± 47.9 μg/m3; PM2.5, 83.4 ± 59.6 μg/m3) in Taiwan (Hien et al. 2022). In addition, according to our ongoing investigation (unpublished), the indoor data of the same temple showed that PM2.5 concentrations exceed Taiwan standard by 5–18 times (401.44±220.46 μg/m3). Moreover, PAHs released from incense burning have also been measured at significant levels, with potential implications for cancer risk (Kuo et al. 2003; Chiang and Liao 2006; Chen et al. 2022). Therefore, long-term exposure to these carcinogens from incense smoke can have adverse effects on human health, particularly on the respiratory system and brain connectivity (Lin et al. 2008; Chen et al. 2017; Wong et al. 2020).
Smokers exposed to indoor incense burning, in addition to cigarette smoke, have been found to have an increased risk of lung cancer; high levels of cumulative incense exposure and cigarette smoking seem to have a synergistic effect (Tse et al. 2011). Chen et al. (2022) subsequently found that indoor incense burning, even in the absence of cigarette smoking, is associated with an increased risk of lung cancer. It is capable of initiating oxidative stress (cell and tissue damage), leading to systemic or chronic inflammation and pulmonary diseases such as asthma and chronic obstructive pulmonary disease (COPD), as well as sepsis-induced acute lung injury (MacNee 2001; Caramori and Papi 2004; Guo and Ward 2007; Hoshino and Mishima 2008; Pizzino et al. 2017). Polycyclic aromatic hydrocarbons (PAH), found in incense smoke, can also damage cells and cause proinflammatory effects (Miousse et al. 2015; Tong et al. 2019).
Human health can be adversely affected by both incense burning and outdoor air pollution. In Taiwan, rituals involving burning incense are conducted indoors in semi-open or closed temples, leading to higher air pollution levels (Hien et al. 2022). Similarly, a study in Hong Kong found that temples located in urban and residential areas, whether semi-open or closed, could impact the health of nearby pedestrians and residents (Cai and Wong 2021). Such rituals can elevate air pollutant concentrations around the temples beyond background levels, influencing the health of temple workers, worshippers, and residents (Lau and Luk 2001; Cai and Wong 2021).
Moreover, atmospheric pollution exhibits seasonal variation, with fine particulate matter (PM2.5) showing higher daily mean concentrations during cold weather seasons compared to warm seasons (Hwang et al. 2018). In Taiwan, air pollution worsens in the cold season, and higher PM2.5 levels are associated with increased hospital emergency room visits for respiratory diseases (Hwang et al. 2017). Analyzing data from the Beijing Environmental Center in 2016, Lu et al. (2018) observed worse PM2.5, NO2, and carbon monoxide (CO) pollution in autumn and winter than in spring and summer, while PM10 pollution was worse in spring and autumn than in winter and summer.
To prevent the occurrence of disease or to ensure early diagnosis, detection of the short-term immediate impacts of air pollution is critical. Short-term exposure to PM2.5 and NO2 can cause a neutrophil-mediated airway inflammatory response, which can lead to clinical symptoms (Guo et al. 2020a, b, c). Early detection can motivate medical therapy or the reduction of exposure to major pollutants and effectively minimize any clinical symptoms. Therefore, we conjectured that detecting inflammatory responses could be a rapid and direct method of understanding the impact of burning incense on human health (Di et al. 2021).
Studies of the effects of air pollution on inflammation have mostly focused on serum analyses of fibrinogen, interleukin (IL)-1β, IL-6, IL-17, PAI-1, 8-hydroxy-2-deoxyguanosine (8-OHdG)-tumor necrosis factor (TNF)-alpha, and high-sensitivity C-reactive protein (hs-CRP). However, collecting exhaled breath condensate (EBC) may also be effective in evaluating the effects of air pollution on inflammatory responses (Seifi et al. 2021). EBC, a non-invasive method of collecting airway lining fluid, is a simple way to observe the pulmonary environment (Pirozzi et al. 2015). It is a promising method to reflect the levels of inflammatory biomarkers and monocyte chemoattractant protein (MCP)-1 and to identify respiratory or pulmonary-related diseases (Kharitonov and Barnes 2001; Montuschi and Barnes 2002; Fireman et al. 2019).
Exposure to burning incense can increase inflammation. Many studies have focused on the effects of incense burning on serum components (Fang et al. 2003; Pandey et al. 2013); few studies have examined the impact of incense burning on inflammatory cytokines (Navasumrit et al. 2008). Hence, the association between incense burning and systemic inflammatory cytokines needs to be studied further. Inflammatory responses are the most direct effect of burning incense exposure on health. We investigated the effects of burning incense on inflammatory biomarkers among temple workers and other residents in the Chiayi area, Taiwan.
Material and methods
Study design and participants
A longitudinal observational design was employed. Participants were divided into two groups: exposed and control. The former group included workers and volunteers, recruited from a temple in Chiayi County, Taiwan, who had long-term exposure to burning incense. The control group included residents of the Chiayi area recruited from outpatient clinics of a regional hospital’s family medicine department. The inclusion criteria for the participants were (1) lived in the Chiayi area for at least 1 year; (2) aged 18 years or older; and (3) had the ability to understand and communicate in Mandarin or Taiwanese. Patients with any known diseases, such as heart disease, asthma, tuberculosis, autoimmune diseases, or cancer, which would have been associated with inflammation indistinguishable from PM-associated inflammation were excluded from the control group, as were patients who had undergone surgery within 1 month of enrollment. Age and sex were matched between the exposed and control groups. We scheduled two follow-up visits between November 2019 and December 2020. One follow-up visit was conducted in the hot weather season (May–November) and one in the cold season (December–April).
A power analysis, conducted to determine an adequate sample size for analyses of covariance with statistical power of .80, a medium effect size of .25, and an alpha level of 0.05 (Guo et al. 2020a, b, c), showed that a target sample size of 128 participants was sufficient. Thus, the targeted total sample size was 64 participants per group. Ethical approval was obtained from the Institutional Review Board (IRB) of the Chang Gung Medical Foundation (IRB No. 201901540B0C501, approved on October 28, 2019).
Participants, who are temple workers or volunteers, in the exposed group (n = 64) were recruited before the control group participants were recruited. Sixty-four potential participants were asked to participate in the control group; however, eight of them declined to participate and one did not live in the Chiayi area. In total, 119 participants consented to participate. During the study, 25 participants in the exposed group and 27 in the control group were lost to follow-up because they did not complete the follow-up questionnaires or blood tests; additionally, two participants withdrew because of concerns about the COVID-19 pandemic and were excluded from the final analysis. Consequently, the data of 67 participants were included in the final analysis, 39 in the exposed group and 28 in the control group (see Fig. 1 for details).
Demographic and health characteristics of participants
After explaining the objectives and procedures of the study, informed consent was obtained from those who were willing to participate. We requested enrolled participants to complete a questionnaire through an interview, to provide blood samples, and to undergo a lung function test. The questionnaire obtained information about the participants’ sex, age, occupation, religion, marital status, education level, and diagnoses, so that a Charlson Comorbidity Index could be calculated. The Charlson Comorbidity Index is a method of categorizing comorbidities of patients based on the International Classification of Diseases (ICD) and was first developed by Charlson et al. as a weighted index to predict risk of death within 1 year of hospitalization for patients with specific comorbid conditions. The environmental conditions of the participants’ private residences and lifestyles (i.e., exercise, smoking history, environmental tobacco smoke exposure, incense burning, and diet) were also collected so that potential confounding variables could be controlled. All of the participants were required to complete the questionnaire items during each follow-up.
Air quality
To investigate the impact of exposure to burning incense on inflammatory biomarkers in serum and EBC, PM2.5 and NO2 data were acquired from official monitoring stations of the Taiwan Air Quality Monitoring Network (TAQMN). To measure the exposure to burning incense, PM2.5 and NO2 concentrations were adopted from the 24-h average data acquired from the stations near the temple or private residences where the participants were located. Data from a monitoring station near these areas were considered appropriate to evaluate personal exposure (Di et al. 2021).
Inflammatory biomarkers
Exhaled breath condensate (EBC)
EBC was collected as a liquid on an Eco screen using a Turbo DECCS (Medivac, Parma, Italy) within 10–15 min and stored at −80 °C. EBC examination is a non-invasive and safe method of collecting airway lining fluid to observe the pulmonary environment (Seifi et al. 2021; Pirozzi et al. 2015), and is used to evaluate pulmonary inflammation. It is a promising method to reflect the levels of inflammatory biomarkers (such as IL-1β, IL-6, and IL-8) and identify respiratory or pulmonary diseases (Kharitonov et al. 2001; Montuschi et al. 2002; Fireman et al. 2019). In the current study, EBC was collected to analyze the levels of inflammatory cytokines, including IL-1β, IL-6, IL-8, IL-17A, and MCP-1. The inflammation levels of these cytokines were determined using an enzyme-linked immunosorbent assay (ELISA) kit using ELISA MAX™ Deluxe Set (BioLegend, San Diego, CA, USA). Absorbance at 450 and 540 nm was measured using an ELISA reader.
Blood biomarkers
Blood samples were collected to determine the serum concentration of inflammatory cytokines, including IL-1β, IL-6, IL-8 IL-17A, TNF-α, hs-CRP, a biomarker of oxidative stress, 8-OHdG, and inflammatory responses of participants. The 8-OHdG level is also an indicator of PAHs. The serum levels of IL-1β, IL-6, IL-8, IL-17A, and TNF-α were determined with an ELISA kit using ELISA MAX™ Deluxe Set (BioLegend, San Diego, CA, USA). The hs-CRP levels were measured with an ELISA kit using a Human C-Reactive Protein ELISA Kit (Assaypro, St Charles, MO, USA). ELISA was performed to determine PAI-1 concentrations using the Human PAI-1 Assay Max ELISA Kit (Assaypro, St Charles, MO, USA). 8-OHdG levels were measured using an 8-OHdG ELISA Kit (Finetest, Wuhan, Hubei, China). Absorbance at 450 and 540 nm was measured using an ELISA reader.
Dyspnea and lung function
The modified Medical Research Council (mMRC) dyspnea scale was used to assess dyspnea among participants. The mMRC scale ranges from 0 to 4, with a higher value indicating a more severe state of dyspnea; the scale has been shown to have good reliability (Tsai et al. 2012). Each study participant underwent a lung function test in both the hot and cold weather seasons. A spirometer (BTL-08 Spiro Pro; BTL, UK) was used to measure the forced expiratory volume in 1 s (FEV1), forced vital capacity (FVC), and the FEV1/FVC.
Self-care knowledge of particulate matter
Self-care knowledge of particulate matter (PM) was a questionnaire developed by the research team and consisted of 16 items about self-care knowledge regarding air pollution (Guo et al. 2020a, b, c). The results were evaluated by three experts for scale-content validity, which was found to be .92, thus, exhibiting good validity, based on a study by Shi (2012). Additionally, Cronbach’s alphas of the original and current studies were .84 and .81, respectively. Participants with higher scores demonstrated superior self-care knowledge regarding air pollution.
Statistics
Demographics and characteristics of the exposed and control groups were compared using independent t-tests for continuous variables and Fisher’s exact tests for categorical variables. The mMRC scores were compared using the Mann-Whitney U-test due to non-normal distribution. Wilcoxon signed-rank test was used to compare changes in serum tests and EBC between cold and warm seasons (combined exposed and control groups). Differences in serum tests and EBC between exposed and control group participants were assessed using the Mann-Whitney U-test. Quantile regression was employed to evaluate the association between exposure status and weather changes (hot-cold difference) in serum tests/EBCs, while controlling for confounding factors. Covariates included waist-to-hip ratio, education level, self-care knowledge of PM, smoking by family members in the house, exposure to burning incense, PM2.5, and NO2 in the living township and some health behaviors (use of air purifiers, and total duration of exercise). The desired quantile was the 50th percentile and the standard error was calculated under the assumption of independent and identically distributed errors. Statistical analyses were conducted using SPSS 26 software (IBM SPSS, Chicago, IL, USA). SPSS 26 software was used for statistical analyses, with a significance level set at p < .05.
Results
Demographics and characteristics
Female participants outnumbered male participants (40 (59.7%) vs. 27 (40.3%)). The mean age, in the cold weather season, was 61.2 years (standard deviation (SD) = 10.9 years), ranging from 33 to 82 years. Table 1 presents the demographics and characteristics of the exposed and control group participants. The exposed group participants were more likely to have religious beliefs, lower education levels, and poorer self-care knowledge of PM, and were more likely to be exposed to burning incense than the control group participants, in both the cold and hot weather seasons. The lung symptoms (mMRC score and FEV1) were significantly more severe in the exposed group than in the control group in the cold weather season but not in the hot season. Furthermore, ambient PM2.5 and NO2 levels were significantly lower in the exposed group during the cold season, whereas they were significantly higher in the exposed group during the hot season (see Table 1).
Based on the study design, EBC samples were collected in the hot and cold weather seasons; however, some participants could only collect EBC once during the study period because of the social interruption caused by the COVID-19 pandemic. Therefore, we excluded the participants with only one EBC dataset (n = 16); consequently, 118 EBC datasets from the two groups were analyzed.
Serum tests and EBC between the cold and warm seasons
We compared serum tests and EBC between the cold and warm seasons (see Table 2). The results showed significant changes in all these parameters (p < .05). Specifically, hs-CRP and 8-OHdG values decreased significantly from the cold to warm seasons, while the values of other parameters significantly increased during this period.
Serum tests and EBC of the exposed and control group participants
Serum tests and EBC of the exposed and control group participants were compared in the cold and hot weather seasons (see Table 3). We found that the serum IL17-A and TNF-α levels were significantly higher in the exposed group than in the control group in both seasons. The serum IL-6 and hs-CRP levels were significantly higher in the exposed group than in the control group in the cold season, whereas the serum IL-1β and IL-8 levels were significantly higher in the exposed group in the hot season. The 8-OHdG level was significantly lower in the exposed group during the hot season. In terms of the EBC, the IL-6 and MCP-1 levels were significantly higher in the exposed group than in the control group during the cold weather season, but not during the hot season. The IL-8 levels were significantly lower in the exposed group during both seasons (see Table 3).
Hot-cold differences in the exposed and control group participants
Table 4 shows the hot-cold weather differences between the exposed and control participants. The unadjusted quantile regression models demonstrated that the hot-cold differences in serum IL-1β, IL-6, IL-8, IL17-A, TNF-α, and PAI-1 were significantly greater in the exposed group than in the control group (all p values < .05; see the exact p values in Table 4). After multivariable adjustment, exposure status was significantly associated with a greater hot-cold difference in serum IL-1β (regression coefficient (B) = 6.6, 95% confidence interval (CI) = 5.0–8.3, p < .001), IL17-A (B = 2.4, 95% CI = 0.3–4.5, p = .03), and PAI-1 (B = 5.4, 95% CI = 1.5–9.3, p = .01). The exposed group had a greater hot-cold difference in serum TNF-α than the control group (p = .06). Figure 2 illustrates the distribution of serum levels of IL-1β, IL17-A, TNF-α, and PAI-1 in the two groups. In terms of EBC, the unadjusted quantile regression models showed that the hot-cold differences in IL-1β, IL-6, and IL-8 were significantly lower in the exposed group than in the control group (all p values < .05). However, exposure status was not independently associated with the hot-cold differences in all the EBC measurements, after adjusting for the covariates (see Table 4).
Discussion
This study examined the inflammatory responses of temple workers and volunteers to air pollutants from burning incense. The exposed group showed higher inflammatory levels than the control group in both hot and cold weather seasons, and environmental incense emission was associated with changes in serum biomarkers. In this study, the control group participants had higher PM2.5 and NO2 concentrations compared to the exposed group. However, the inflammatory levels in the control group were lower than those in the exposed group. This discrepancy might be due to the fact that the PM2.5 and NO2 concentrations were based on official data from the TAQMN near their homes, rather than their actual PM2.5 exposure data. Although the representation of exposure situations in the exposed group during incense burning at the temple or at home is limited, the inflammatory levels still reflect their true levels of air pollution exposure. The exposed (temple) group experienced long-term exposure to higher concentrations of indoor air pollutants both at the temple and at home. Our ongoing investigation (unpublished) has revealed that PM2.5 concentrations at the temple exceed Taiwan’s standard by 5–18 times. Additionally, participants in the exposed group, following their religious practices, burn incense at home frequently, leading to high concentrations of PM at home (Lung et al. 2021). Indoor burning of incense and joss papers results in PM2.5 and PM1 concentrations of 277.3 μg/m3 and 201.0 μg/m3, respectively (Lung et al. 2021). Moreover, PM2.5 from incense emissions indoors is approximately 1.53 ± 1.79 times higher than outdoor concentrations when burning incense for 30 to 60 min (Lung et al. 2021; Hien et al. 2022). Another study in Taiwan demonstrated that PM10 and PM2.5 concentrations were highest within 30 min after incense burning (Guo et al. 2020a, b, c). Consequently, the exposed group may have high exposure to air pollutants both at the temples and at home, potentially impacting their inflammatory biomarker reaction for long period compared to the control group.
Compared with the control group, the exposed group exhibited lower scores in their knowledge of air pollution and higher frequency of incense burning, which may have resulted in exposure to a higher concentration of indoor air pollutants; moreover, this group did not apply air pollution prevention interventions. The temple usually holds about 13 important festivals in the cold weather season, during which many worshippers visit the temple and burn incense, increasing the health risks of temple workers and volunteers who stay in the temple for prolonged periods. We found that the cold season exhibited a peak in the frequency of temple religious activities and festivals and the number of worshippers. Lung symptoms, mMRC scores, and FEV1 were significantly different between the two groups in the cold season; thus, in addition to atmospheric factors, intensive religious festivals during the cold season could influence the air quality of the temple and increase the health risk of temple workers and volunteers. Temple workers and volunteers who have long-term exposure to PM from incense burning are at risk of respiratory disease, various infectious diseases, inflammatory and autoimmune disorders, and cancer.
In addition to ambient particles, indoor incense burning releases synergistic PM and PM components that deteriorate health (Lin et al. 2008; Chen et al. 2017; Tse et al. 2011) and elicit an inflammatory response (Niu et al. 2019; Lin et al. 2012; Aalapati et al. 2014; Zhao et al. 2019). A previous study found that the PAH levels inside a temple were much higher than those in the outside environment and that temples were significant PAH and TSP producers, thus contributing to serious health hazards in local workers (Yadav et al. 2022). However, in the current study, 8-OHdG levels did not significantly differ between the two groups. Indoor air pollutants may differ in the groups, but we did not control for the involvement of participants in specific occupations and did not monitor PAH levels. A future examination of PAH levels and biomarkers between the two groups may reveal notable findings.
Incense burning generates heavy PM2.5 and NO2 emissions, which can induce oxidative stress (Niu et al. 2019) and stimulate an increase in inflammatory cytokines, including IL-1, IL-6, IL-8, IL-17A, and TNF-α (Lin et al. 2012; Aalapati et al. 2014; Zhao et al. 2019). In our study, temple workers and volunteers with long-term exposure to incense emissions had significantly higher levels of inflammatory responses than the control group. On examining the biomarkers from the serum of the exposed group, we found that TNF-α and IL-1β showed significantly higher levels, thereby releasing high levels of other inflammatory cytokines, such as IL-17, which could initiate the infiltration of neutrophils into the airways by inducing the release of IL-8 (Zou et al. 2017). Hence, the condition of cytokines in our study might reflect an early inflammation stage (see Table 3).
In the univariate analysis, serum IL-6 and IL-8 levels were significantly higher in the exposed group, consistent with findings from other studies. For example, Lin et al. (2012) found that the exposure of human coronary artery endothelial cells (HCAECs) to particles and PAHs caused an increase in IL-6. IL-6 production is often associated with increased levels of particles (Hassanvand et al. 2017; Ramos et al. 2017). Another study reported that short-term exposure to NO2 increased IL-8 levels (Dadvand et al. 2014), which could explain why the control group had significantly higher levels of EBC IL-8 with higher exposure to NO2 in the cold season.
Although the expression of inflammatory cytokines was demonstrated using the univariate analysis, after controlling for confounding variables (such as waist-to-hip ratio, education level, knowledge of indoor air pollution, use of air purifiers, smoking by family members in the house, exposure to incense burning, total duration of exercise, and PM2.5 and NO2 levels), only IL-1β, IL-17A, and PAI-1 showed significant differences; there were no differences in EBC. The PAI-1 in our analysis was significant, which was consistent with the findings of Wang et al., who reported that short-term exposure to air pollutants, including PM2.5 and NO2, is positively associated with PAI-1 (Wang et al. 2022). Green et al. (2016) reported that PAI-1 levels were related to long-term exposure to PM2.5 in middle-aged women. The long-term effects of incense burning on inflammation in the blood require further investigation. Although the preceding discussion mainly focused on the impact of air pollution on inflammation, it is essential to explore whether incense burning could elicit a similar response in future research.
The results of the current study showed that EBC did not differ after controlling for confounding variables. It could be possible that the inflammatory cytokines in EBC showed no obvious changes for participants in exposing to air pollutant for a long time, and the results of EBC reactions of our study were consistent with those of the study by Hu et al., who observed the effects of long-term exposure to traffic-related air pollution and found that EBC IL-6 is not associated with the distance of road and pollution exposure (Hu et al. 2016). Nevertheless, a previous study reported that the levels of EBC IL-6 and IL-8 increased on the third day after exposure, and TNF-α and IL-17 levels in EBC increased in the first 4 days after exposure to PM2.5; particularly, on the first day, the effects of pollutants on the levels of these cytokines in EBC were remarkable. Moreover, when comparing the effect of the 4-day moving average with the 7-day moving average of PM2.5, it was observed that higher levels of TNF-α and IL-17 in EBC may suggest inflammation occurring in the air passages and subsequently in the lungs (Alves et al. 2018). Another study found a 38.73% increase in EBC TNF-α with exposure to PM2.5 in the past 24 h (lag 0), but a decrease at lag 4 and lag 5. Additionally, a regional difference was observed in the changes of IL-6 in EBC with exposure to PM2.5, and a strong negative correlation between IL-6 and PM2.5 was observed at lags 0, 3, and 4. However, EBC IL-6 was not significantly related to PM2.5 in a less polluted group (Sabeti et al. 2021). These findings suggest that EBC could potentially reflect short-term inflammatory reactions, and emphasize the importance of designing EBC examinations for specific events to better understand the systematic expression of cytokines in EBC.
Table 2 shows lower biomarker results in the cold season compared to the warm season, which is unexpected based on previous studies. This discrepancy might be due to the influence of the COVID-19 pandemic. During the pandemic, lockdowns in Chinese cities led to reduced air pollution levels in Taiwan during the cold season (Griffith et al., 2020). In contrast, in the warm season of 2020, the Taiwanese government eased restrictions on tourism, resulting in increased pollution as people opted for self-driving. Additionally, mask-wearing during the pandemic might have affected the detection of biomarker differences caused by PM2.5 exposure. Nonetheless, this study emphasizes the impact of incense burning. Therefore, the most crucial aspect is the comparison between the exposed and control groups within the same season (Table 3), where biomarkers in the exposed group were observed to be higher than those in the control group
Ambient particles within the temple contain not only PM but also various toxic chemicals, such as PAHs, and these carcinogens probably cause a discrepancy in the mechanism of inflammatory cytokines that affect the health of temple workers and volunteers. This aspect needs to be addressed in future studies.
Limitations
Our study had some limitations. First, our study only included 39 temple workers and volunteers, as well as 28 residents, which did not meet our planned sample size (n=128) due to the impact of the COVID-19 pandemic. This limitation has resulted in underpowered results for our study. To obtain more precise findings, larger-scale studies with an adequate number of participants are crucial. Additionally, the indoor PM levels varied based on participants’ characteristics and behaviors, such as exposure to smoking and incense burning. We relied on official monitoring stations for PM concentrations, which might not accurately represent individual PM exposure. Using personal monitoring equipment would provide more precise concentration estimations. Moreover, EBC collection was not conducted during specific events or worship dates, limiting the observation of short-term inflammatory reactions. To address this, future studies should design EBC examinations during particular events or dates to observe such changes in inflammatory cytokines.
Conclusion
In conclusion, adapting the TAQMN data cannot specifically estimate the effects of indoor pollutants on inflammation in individuals, but our analyses of the study results accorded with our study hypothesis. Individual PM monitoring remains the first-priority method for future studies. Although the current findings hardly predict the endpoint of inflammation in causing disease or acute deterioration, our results showed that burning incense may significantly affect inflammatory responses and clinical symptoms. Additionally, our findings provide a guide for selecting a potential biomarker as an indicator to assess clinical diseases for further preventive health care and education.
Burning incense for worship is an age-old practice; and thus, an intervention to protect temple workers’ health is complex. There is evidence that some incense brands produce lower toxicity from combustion. Working with manufacturers, in addition to educating the public, may be an important first step in protecting the health of those exposed to burning incense. Implementing policies that promote adequate ventilation, limit exposure time and burned amount, and raise awareness about incense burning risks and how to minimize exposure may mitigate associated health risks. In some cases, alternative methods of aromatherapy, such as diffusers or essential oils, which do not produce smoke or harmful particles, may represent an acceptable and safer option.
Data availability
The data that have been used is confidential.
References
Aalapati S, Ganapathy S, Manapuram S, Anumolu G, Prakya BM (2014) Toxicity and bio-accumulation of inhaled cerium oxide nanoparticles in CD1 mice. Nanotoxicology 8(7):786–798
Alves AGF, de Azevedo Giacomin MF, Braga ALF, Sallum AME, Pereira LAA, Farhat LC, Strufaldi FL, Lichtenfels AJDFC, Carvalho TDS, Nakagawa NK, Silva CA, Farhat SCL (2018) Influence of air pollution on airway inflammation and disease activity in childhood-systemic lupus erythematosus. Clinical Rheumatol 37:683–690. https://doi.org/10.1007/s10067-017-3893-1
Bootdee S, Chantara S, Prapamontol T (2016) Determination of PM2.5 and polycyclic aromatic hydrocarbons from incense burning emission at shrine for health risk assessment. Atmos Pollut Res 7:680–689. https://doi.org/10.1016/j.apr.2016.03.002
Cai WH, Wong PPY (2021) Associations between incense-burning temples and respiratory mortality in Hong Kong. Atmosphere 12(6):774. https://doi.org/10.3390/atmos12060774
Caramori G, Papi A (2004) Oxidants and asthma. Thorax 59(2):170–173. https://doi.org/10.1136/thorax.2002.002477
Chen YC, Ho WC, Yu YH (2017) Adolescent lung function associated with incense burning and other environmental exposures at home. Indoor Air 27(4):746–752. https://doi.org/10.1111/ina.12355
Chen KC, Tsai SW, Shie RH, Zeng C, Yang HY (2022) Indoor air pollution increases the risk of lung cancer. Int J Environ Res Public Health 19(3):1164. https://doi.org/10.3390/ijerph19031164
Chiang KC, Liao CM (2006) Heavy incense burning in temples promotes exposure risk from airborne PMs and carcinogenic PAHs. Sci Total Environ 372(1):64–75. https://doi.org/10.1016/j.scitotenv.2006.08.012
Dadvand P, Nieuwenhuijsen MJ, Agustí À, de Batlle J, Benet M, Beelen R, Cirach M, Martinez D, Hoek G, Basagaña X, Ferrer A, Ferrer J, Rodriguez-Roisin R, Sauleda J, Guerra S, Antó JM, Garcia-Aymerich J (2014) Air pollution and biomarkers of systemic inflammation and tissue repair in COPD patients. Eur Respir J 44(3):603–613. https://doi.org/10.1183/09031936.00168813
Di N, He W, Zhang K, Cui J, Chen J, Cheng J, Chu B, Li S, Xie Y, Xiang H (2021) Association of short-term air pollution with systemic inflammatory biomarkers in routine blood test: a longitudinal study. Environ Res Lett 16(3):035007. https://doi.org/10.1088/1748-9326/abd9f3
Fang GC, Chang CN, Chu CC, Wu YS, Fu PPC, Chang SC, Yang IL (2003) Fine (PM 2.5), coarse (PM 2.5-10), and metallic elements of suspended particulates for incense burning at Tzu Yun Yen temple in central Taiwan. Chemosphere 51(9):983–991. https://doi.org/10.1016/s0045-6535(03)00124-3
Fireman KE, Adir Y, Krencel A, Fireman EM, Peri R, Kessel A (2019) Ultrafine particles in airways: a novel marker of inflammation and chronic obstructive pulmonary disease (COPD) exacerbation risk. Am J Respir Crit Care Med 199:A4050. https://doi.org/10.1164/ajrccm-conference.2019.199.1_MeetingAbstracts.A4050
Green R, Broadwin R, Malig B, Basu R, Gold EB, Qu L, Stemfeld B, Bromberger JT, Greendale GA, Kravitz HM, Tomey K, Matthews K, Derby C, Jackson EA, Green R, Ostro B (2016) Long- and short-term exposure to air pollution and inflammatory/hemostatic markers in midlife women. Epidemiology 27(2):211–220. https://doi.org/10.1097/EDE.0000000000000421
Griffith SM, Huang WS, Lin CC, Chen YC, Chang KE, Lin TH, Wang SH, Lin NH (2020) Long-range air pollution transport in East Asia during the first week of the COVID-19 lockdown in China. Sci Total Environ 741:140214. https://doi.org/10.1016/j.scitotenv.2020.140214
Guo RF, Ward PA (2007) Role of oxidants in lung injury during sepsis. Antioxid Redox Signal 9(11):1991–2002. https://doi.org/10.1089/ars.2007.1785
Guo SE, Chi MC, Hwang SL, Lin CM, Lin YC (2020a) Effects of particulate matter education on self-care knowledge regarding air pollution, symptom changes, and indoor air quality among patients with chronic obstructive pulmonary disease. Int J Environ Sci Pollut Res 17(11):4103. https://doi.org/10.3390/ijerph17114103
Guo SE, Chi MC, Lin CM, Yang TM (2020b) Contributions of burning incense on indoor air pollution levels and on the health status of patients with chronic obstructive pulmonary disease. Peer J 8:e9768. https://doi.org/10.7717/peerj.9768
Guo C, Sun X, Diao W, Shen N, He B (2020c) Correlation of clinical symptoms and sputum inflammatory markers with air pollutants in stable COPD patients in Beijing area. Int J Chron Obstruct Pulmon Dis 15:1507
Hassanvand MS, Naddafi K, Kashani H, Faridi S, Kunzli N, Nabizadeh R, Momeniha F, Gholampour A, Arhami M, Zare A, Pourpak Z, Hoseini M, Yunesian M (2017) Short-term effects of particle size fractions on circulating biomarkers of inflammation in a panel of elderly subjects and healthy young adults. Environ Pollut 223:695–704. https://doi.org/10.1016/j.envpol.2017.02.005
Hien TT, Ngo TH, Lung SCC, Ngan TA, Minh TH, Cong-Thanh T, Nauyen LSP, Chi NDT (2022) Characterization of particulate matter (PM1 and PM2.5) from incense burning activities in temples in Vietnam and Taiwan. Aerosol Air Qual Res 22:220193. https://doi.org/10.4209/aaqr.220193
Hoshino Y, Mishima M (2008) Redox-based therapeutics for lung diseases. Antioxid Redox Signal 10(4):701–704. https://doi.org/10.1089/ars.2007.1961
Hu ZW, Zhao YN, Cheng Y, Guo CY, Wang X, Li N, Liu JQ, Kang H, Xia GG, Hu P, Zhang PJ, Ma J, Liu Y, Zhang C, Su L, Wang GF (2016) Living near a major road in Beijing: association with lower lung function, airway acidification, and chronic cough. Chin Med J 129(18):2184–2190. https://doi.org/10.4103/0366-6999.189923
Hwang SL, Lin YC, Guo SE, Chi MC, Chou CT, Lin CM (2017) Emergency room visits for respiratory diseases associated with ambient fine particulate matter in Taiwan in 2012: a population-based study. Atmos Pollut Res 8(3):465–473. https://doi.org/10.1016/j.apr.2016.11.008
Hwang SL, Chi MC, Guo SE, Lin YC, Chou CT, Lin CM (2018) Seasonal variation and source apportionment of PM2.5-bound trace elements at a coastal area in southwestern Taiwan. Environ Sci Pollut Res 25(9):9101–9113. https://doi.org/10.1007/s11356-017-1144-2
Kharitonov SA, Barnes PJ (2001) Exhaled markers of pulmonary disease. Am J Respir Crit Care Med 163(7):1693–1722. https://doi.org/10.1164/ajrccm.163.7.2009041
Kuo CY, Hsu YW, Lee HS (2003) Study of human exposure to particulate PAHs using personal air samplers. Arch Environ Contam Toxicol 44:454–459. https://doi.org/10.1007/s00244-002-1177-4
Kuo SC, Tsai YI, Sopajaree K (2016) Emission characteristics of carboxylates in PM2.5 from incense burning with the effect of light on acetate. Atmospheric Environ 138:125–134. https://doi.org/10.1016/j.atmosenv.2016.05.004
Lau OW, Luk SF (2001) Leaves of Bauhinia blakeana as indicators of atmospheric pollution in Hong Kong. Atmospheric Environ 35(18):3113–3120. https://doi.org/10.1016/S1352-2310(01)00069-3
Lin TC, Yang CR, Chang FH (2007) Burning characteristics and emission products related to metallic content in incense. J Hazard Mater 140:165–172
Lin TC, Krishnaswamy G, Chi DS (2008) Incense smoke: clinical, structural and molecular effects on airway disease. Clin Mol Allergy 6(1):3
Lin LY, Lin HY, Chen HW, Su TL, Huang LC, Chuang KJ (2012) Effects of temple particles on inflammation and endothelial cell response. Sci Total Environ 414:68–72. https://doi.org/10.1016/j.scitotenv.2011.08.050
Liou SW, Chen CY, Yang TT, Lin JM (2008) Determination of particulate-bound formaldehyde from burning incense by solid phase microextraction. Bull Environ Contam Toxicol 80:324–328. https://doi.org/10.1007/s00128-008-9381-1
Lu L, Zhang AW, Kang XY (2018) Temporal and spatial characteristics of air pollutants in Beijing. Adv Geosci 8(3):673–682. https://doi.org/10.12677/ag.2018.83071
Lung SC, Kao MC (2003) Worshippers’ exposure to particulate matter in two temples in Taiwan. J Air Waste Manag Assoc 53(2):130–135. https://doi.org/10.1080/10473289.2003.10466140
Lung SC, Tsou MM, Hu SC, Hsieh YH, Wang WV, Shui CK, Tan CH (2021) Concurrent assessment of personal, indoor, and outdoor PM2.5 and PM1 levels and source contributions using novel low-cost sensing devices. Indoor Air 31(3):755–768. https://doi.org/10.1111/ina.12763
MacNee W (2001) Oxidative stress and lung inflammation in airways disease. Eur J Pharmacol 429(1-3):195–207. https://doi.org/10.1016/S0014-2999(01)01320-6
Miousse IR, Chalbot MCG, Pathak R, Lu X, Nzabarushimana E, Krager K, Aykin-Burns N, Hauer-Jensen M, Demokritou P, Kavouras IG, Koturbash I (2015) In vitro toxicity and epigenotoxicity of different types of ambient particulate matter. Toxicol Sci 148(2):473–487. https://doi.org/10.1093/toxsci/kfv200
Montuschi P, Barnes PJ (2002) Analysis of exhaled breath condensate for monitoring airway inflammation. Trends Pharmacol Sci 23(5):232–237. https://doi.org/10.1016/s0165-6147(02)02020-5
Navasumrit P, Arayasiri M, Hiang OMT, Leechawengwongs M, Promvijit J, Choonvisase S, Chantchaemsai S, Nakngam N, Mahidol C, Ruchirawat M (2008) Potential health effects of exposure to carcinogenic compounds in incense smoke in temple workers. Chem Biol Interact 173(2008):19–31. https://doi.org/10.1016/j.cbi.2008.02.004
Niu X, Ho KF, Chuang HC, Sun J, Huang Y, Hu T, Xu H, Duan J, Lui KH, Cao J (2019) Comparison of cytotoxicity induced by PM2.5-bound polycyclic aromatic compounds from different environments in Xi’an, China. Atmos Environ 216:116929. https://doi.org/10.1016/j.atmosenv.2019.116929
Pandey P, Patel DK, Khan AH, Barman SC, Murthy RC, Kisku GC (2013) Temporal distribution of fine particulates (PM2.5, PM10), potentially toxic metals, PAHs and Metal-bound carcinogenic risk in the population of Lucknow City, India. J Environ Sci Health Part A-Toxic/Hazard Subst Environ Eng 48(7):730–745. https://doi.org/10.1080/10934529.2013.744613
Pirozzi C, Sturrock A, Weng HY, Greene T, Scholand MB, Kanner R (2015) Effect of naturally occurring ozone air pollution episodes on pulmonary oxidative stress and inflammation. Int J Environ Res Public Health 12(5):5061–5075. https://doi.org/10.3390/ijerph120505061
Pizzino G, Irrera N, Cucinotta M, Pallio G, Mannino F, Arcoraci V, Squadrito F, Altavilla D, Bitto A (2017) Oxidative stress: harms and benefits for human health. Oxid Med Cell Longev 2017:8416763. https://doi.org/10.1155/2017/8416763
Ramos D, Proenca M, Leite MR, Ferreira AD, Trevisan IB, Brígida GFS, Tacao GY, Ramos EMC (2017) Effects of exposure to biomass burning on pulmonary inflammatory markers and pulmonary function in individuals with COPD. Rev Port Pneumol 23(5):273–279. https://doi.org/10.1016/j.rppnen.2017.04.003
Sabeti Z, Ansarin K, Seyedrezazadeh E, Jafarabadi MA, Zafari V, Dastgiri S, Shakerkhatibi M, Gholampour A, Khamnian Z, Sepehri M, Dahim M, Sharbafi J, Hakimi D (2021) Acute responses of airway oxidative stress, inflammation, and hemodynamic markers to ambient PM2. 5 and their trace metal contents among healthy adolescences: a panel study in highly polluted versus low polluted regions. Environ Pollut 288:117797. https://doi.org/10.1016/j.envpol.2021.117797
Seifi M, Rastkari N, Hassanvand MS, Naddafi K, Nabizadeh R, Nazmara S, Kashani H, Zare A, Pourpak Z, Hashemi SY, Yunesian M (2021) Investigating the relationship between particulate matter and inflammatory biomarkers of exhaled breath condensate and blood in healthy young adults. Sci Rep 11(1):1–11. https://doi.org/10.1038/s41598-021-92333-6
Shen H, Tsai CM, Yuan CS, Jen YH, Ie IR (2017) How incense and joss paper burning during the worship activities influences ambient mercury concentrations in indoor and outdoor environments of an Asian temple? Chemosphere 167:530–540. https://doi.org/10.1016/j.chemosphere.2016.09.159
Shi J, Mo X, Sun Z (2012) Content validity index in scale development. Journal of Central South University. Med Sci 37(2):152–155. https://doi.org/10.3969/j.issn.1672-7347.2012.02.007
Tong X, Chen XC, Chuang HC, Ho SSH, Lui KH, Ho KF (2019) Characteristics and cytotoxicity of indoor fine particulate matter (PM2.5) and PM2.5-bound polycyclic aromatic hydrocarbons (PAHs) in Hong Kong. Air Qual Atmos. Health 12(12):1459–1468. https://doi.org/10.1007/s11869-019-00762-0
Tsai MJ, Huang HP, Wang CY, Yang CJ, Sheu CC, Hung JY, Wang TH, Huang MS (2012) Chronic obstructive pulmonary disease assessment test (CAT) correlated well with modified medical research council (MMRC) dyspnea scale. Thoracic Med 27(6):338–348. https://doi.org/10.29806/TM.201212.0003
Tse LA, Yu ITS, Qiu H, Au JSK, Wang XR (2011) A case-referent study of lung cancer and incense smoke, smoking, and residential radon in Chinese men. Environ. Health Perspect 119(11):1641–1646. https://doi.org/10.1289/ehp.1002790
Wang K, Wang W, Lei L, Lan Y, Liu Q, Ren L, Wu S (2022) Association between short-term exposure to ambient air pollution and biomarkers of coagulation: a systematic review and meta-analysis. Environ Res 215:114210. https://doi.org/10.1016/j.envres.2022.114210
Wong A, Lou W, Ho KF, Yiu BKF, Lin S, Chu WCW, Abrigo J, Lee D, Lam BYK, Au LWC, Soo YOY, Lau AYL, Kwok TCY, Leung TWH, Lam LCW, Ho K, Mok VCT (2020) Indoor incense burning impacts cognitive functions and brain functional connectivity in community older adults. Sci Rep 10(1):1–11. https://doi.org/10.1038/s41598-020-63568-6
Yadav VK, Malik P, Tirth V, Khan SH, Yadav KK, Islam S, Choudhary N, Inwati GK, Arabi A, Kim DH, Jeon BH (2022) Health and environmental risks of incense smoke: mechanistic insights and cumulative evidence. J Inflamm Res 15:2665–2693. https://doi.org/10.2147/JIR.S347489
Yang TT, Lin ST, Lin TS, Hong WL (2012) Characterization of polycyclic aromatic hydrocarbon emissions in the particulate phase from burning incenses with various atomic hydrogen/carbon ratios. Sci Total Environ 414(1):335–342. https://doi.org/10.1016/j.scitotenv.2011.11.014
Zhao CN, Xu Z, Wu GC, Mao YM, Liu LN, Wu Q, Dan YL, Tao SS, Zhang Q, Sam NB, Fan YG, Zou YF, Ye DQ, Pan HF (2019) Emerging role of air pollution in autoimmune diseases. Autoimmun Rev 18(6):607–614. https://doi.org/10.1016/j.autrev.2018.12.010
Zou Y, Chen X, Liu J, Zhou DB, Kuang X, Xiao J, Yu Q, Lu X, Li W, Xie B, Chen Q (2017) Serum IL-1β and IL-17 levels in patients with COPD: associations with clinical parameters. Int J Chron Obstruct Pulmon Dis 12:1247–1254. https://doi.org/10.2147/COPD.S131877
Acknowledgements
The authors gratefully acknowledge the financial support provided by the Chang Gung Medical Foundation of Taiwan and National Science and Technology Council. The authors would also like to thank Chiayi Chang Gung Hospital and all the participants of this study for their valuable contributions.
Funding
This research was supported by the Chang Gung Medical Foundation of Taiwan (grant numbers: CMRPF6H0111, CMRPF6J0031, CMRPF6J0041, CMRPF6K0101, and CMRPF6K0102) and National Science and Technology Council (grant numbers: NMRPF6G0021 and NMRPF6H0021).
Author information
Authors and Affiliations
Contributions
S.E.G.: conceptualization, methodology, software, data curation, visualization, investigation, supervision, validation, writing- original draft preparation, writing–reviewing and editing. P.A.R., S.C.T., C.M.L., M.C.C., C.W. L., and Y.C.Y.: writing–original draft preparation, writing–reviewing and editing. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent was obtained for all study participants. The study was approved by the Institutional Review Board (IRB) of the Chang Gung Medical Foundation (IRB No. 201901540B0C501, approved on October 28, 2019).
Consent for publication
Not applicable
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Guo, SE., Ratner, P.A., Tseng, SC. et al. Exposure to incense burning, biomarkers, and the physical health of temple workers in Taiwan. Environ Sci Pollut Res 30, 101804–101816 (2023). https://doi.org/10.1007/s11356-023-29420-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-023-29420-w