Abstract
The SARS-CoV-2 is a deceptive virus. Despite the remarkable progress in genetic sequencing and subsequent vaccine development, the world continues to grapple with the ominous threats of rapidly appearing SARS-CoV-2 variants. The objective of this manuscript is to rank world countries based on the anticipated scope of COVID-19 morbidity and mortality, measured in terms of prevalence per 1 million persons, from the lowest to the highest. The ranking of 162 countries is based on predictions of empirical models, which include three explanatory variables: hospital beds per thousand persons, population density, and the median age of the country’s population. Referring to the COVID-19 scope of morbidity, the lowest likelihood of infection is obtained in Niger and Mali, where the dominant characteristic is the young median age (15.1–16.4 years). Referring to the COVID-19 scope of mortality, the lowest likelihood is obtained in Singapore. For Singapore, the dominant feature is the high population density. The optimal solution is intensive vaccination campaigns in the initial phase of the pandemic, particularly among countries with low GDP per capita. Yet, vaccinations may work only where the personal immune system is healthy and thus respond by creating antibodies to the SARS-CoV2 virus. Referring to populations that lack the natural protection of the healthy immune system and thus cannot be vaccinated (e.g., old people, cancer patients undergoing chemotherapy treatments), a complementary solution might be coordination between countries and the establishment of field hospitals, testing laboratories, isolation of areas, humanitarian aid—in the same manner of treatment in other disasters like earthquakes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), responsible for the COVID-19 pandemic, is a deceptive virus. Despite the remarkable progress in genetic sequencing and subsequent vaccine development (Kim et al. 2020), the world continues to grapple with the ominous threats of rapidly appearing SARS-CoV-2 variants (García et al. 2022). Consequently, it is important to investigate the COVID-19 risk factors and their relative impact on country ranking in terms of the anticipated scope of morbidity and mortality. From a public policy perspective, Flaxman et al. (2020) concluded that major non-pharmaceutical interventions—and lockdowns in particular—have had a large effect on reducing transmission. Continued intervention should be considered to keep the transmission of SARS-CoV-2 under control.
The objective of the current study is to explore the optimal country in which the criteria for ranking are projected cases and deaths per 1 million persons obtained from a regression analysis. In that respect, we can rank the optimal countries and attempt to study from their experience in an effort to address future pandemics. The explanatory variables from which projected values are generated include three risk factors applied to 162 countries from January 22, 2020, to January 21, 2022: (1) the number of hospital beds per thousand persons, (2) population density, and (3) median age of the country’s population. Estimation is based on the fractional probit, negative binomial, and Poisson regressions. The former models can only be applied to dependent variables bounded between zero and one.Footnote 1
The number of beds per thousand persons may be considered a proxy for other latent variables, including the wealth of the country and the type of regime and civil liberties. In democratic societies, public representatives need to be re-elected. Consequently, their inclination to invest in public health is higher (e.g., Arbel et al. 2022). The incentive structure, which promotes health services in democracies, might emanate from the objective function of the politicians to maximize their prospects for re-election. Consequently, improved health services may, in turn, promote public satisfaction (e.g., Martinez-Bravo et al. 2012, who demonstrated that elections significantly increase public goods expenditure in rural China Mainland). Several recent studies demonstrated that a better medical infrastructure in hospitals and the accrual of clinical knowledge with time promote the prospects of survival (Docherty et al. 2021; Grosso et al. 2021). The other two variables considered—population density and median age—were identified in the literature as salient risk factors of COVID-19 (e.g., Hägg et al. 2020; Hamidi et al. 2020; Petrilli et al. 2020; O’Driscoll et al. 2021). Alternatively, as proposed by Hradsky and Komarek (2021), the number of hospital beds is one of the very few variables that can be controlled by authorities in the face of future pandemics, at least in some countries.
The findings of our analysis demonstrate that the lowest likelihood of infection is obtained in Niger (3684 anticipated cases per 1 million persons) and Mali (3830 anticipated cases per 1 million persons), where the dominant characteristic is the young median age (15.1–16.4 years). Referring to the COVID-19 scope of mortality, the lowest likelihood is obtained in Singapore (2.35 anticipated deaths per 1 million persons—lower by a factor of \(\frac{104.6}{2.35}=\) 44.51 from the second optimal country). For Singapore, the dominant feature is the high population density (7915 persons per square kilometer).
One of the important lessons that emanate from the empirical evidence might be the need to extend budget spending on health and cooperation across states in emergency situations. In light of the related limitations, it is difficult to prevent the spread of future pandemics. However, coordination between countries and the establishment of international medical professional teams for the management of the crisis—such as the treatment of earthquakes—the establishment of field hospitals, testing laboratories, isolation of areas, humanitarian aid in infected areas, international studies with prioritization, and incentives for the same issue.
The remainder of this article is organized as follows. The “Addressing the COVID-19 pandemic: proposed measures and solutions” section gives the literature review. The “Methods” section reports the sample and data, the measures, and the model and data analysis procedures. The “Results” section provides the results and the “Robustness tests” section—the robustness test. Finally, the “Conclusions” section concludes and summarizes.
Addressing the COVID-19 pandemic: proposed measures and solutions
COVID-19 is a global pandemic with extensive collateral damages manifested in losses of lives and livelihoods. Msemburi et al. (2023) mentioned several problems associated with the official World Health Organization COVID-19 mortality rate statistics at a global level including inconsistent certification of COVID-19 as the cause of death, differential diagnostic capacity, and variations in testing access. A more accurate measure is that of an excess mortality, namely the difference between pre- and post-pandemic total mortality rates. Using a Poisson count framework, Msemburi et al. (2023) estimated global excess mortality by 14.83 million persons, 2.74 times more deaths than the 5.42 million reported due to COVID-19 for the study period of 2020–2021. Tomer et al. (2021) indicate a paradox associated with the initial spread of the COVID-19 pandemic. While countries with the lowest ranking on World Health Index (WHI), either escape or were least affected by the disease initially, countries with the highest WHI were mostly affected by the pandemic. Yet, higher-ranking countries in WHI overcome significantly and more quickly than lower ranks countries. In that context, Yuan et al. (2020) estimated the R(t) measure in selected European countries at the beginning of the pandemic (prior to March 2020) to be greater than two. The implication is that each COVID-19 patient infects more than two persons.
One of the fundamental problems in the COVID-19 pandemic crisis is the measurement of the preparedness of countries to cope with pandemic threats. Coccia (2022a) proposed two measures. The resilience index identifies the countries with the best performance in reducing the negative impact of mortality related to the COVID-19 pandemic and the preparedness and prevention index evaluates the countries with the best performance to support COVID-19 vaccinations. Results suggest that the best-performer European countries to cope with the COVID-19 pandemic crisis have a smaller population size and/or better public governance, associated with high expenditures in the health system. Coccia (2020) defines critical decisions as an attempt to apply efficient modes of cognition and action to enable the organizations/individuals to cope with consequential environmental threats. This is particularly important given a growing dynamic of emergencies, such as the COVID-19 pandemic.
Benati and Coccia (2022) demonstrated a positive association between doses of vaccines administered and the local governance index. Dowd et al. (2020) compared South Korea and Italy—countries with similar characteristics, but different age compositions. The authors recommended to adjust the social distancing and other policies to the age composition of local and national contexts as well as intergenerational interactions.
An important aspect of the spread of the pandemic is the environmental one. In fact, human-to-human transmission is a critical factor, but shedding of the SARS-CoV-2 virus (and/or other pathogenic microbes) through excreta, reaching wastewater, and then watercourses or other environmental compartments (soil, plants, surface and groundwater, etc.) is of increasing concern. It is especially important in those regions where wastewater collection and treatment are not available, and sanitation is limited. In addition, the effects of weather conditions, as well as those of air pollutants, are being investigated for this virus and other microbes causing epidemics. In this sense, airborne transmission has been considered crucial, now and in the future. The eventual waterborne transmission is also important, with relevance due to wastewater-based epidemiology, and mostly considering that future mutations could make more feasible fecal–oral and/or other transmission routes, which highlights the great interest in interdisciplinary research (Núñez-Delgado et al. 2021). Based on statistical analyses from March 2020 to February 2021 in Italy, Bontempi and Coccia (2021) suggest a high association between the total import and export of provinces with confirmed COVID-19 cases over time.
As demonstrated in Coccia (2022b, c) the short-run optimal solution seems to be about 80 doses of vaccines per 100 inhabitants combined with intensive vaccination campaigns in the initial phase of the pandemic, particularly among countries with low GDP per capita. Yet, vaccinations may work only where the immune system is healthy and thus respond by creating antibodies to the SARS-CoV2 virus. Also, according to Coccia (2022d), many factors may attenuate the vaccination effectiveness, including (1) the Peltzman effects, namely the tendency to increase risky behavior (e.g., not wearing facemasks, attending crowded places) following the vaccination campaign, (2) New SARS-CoV2 variants (Delta; Omicron), (3) health investment—where the weak health sector is associated with increased fatality rates, (4) High density of cities and intensive commercial activities (Bontempi and Coccia 2021; Bontempi et al. 2021), (5) environmental pollution and climate factors (Diao et al. 2020).
Referring to populations that lack the natural protection of the healthy immune system and thus cannot be vaccinated (e.g., old people, cancer patients undergoing chemotherapy treatments), a complementary solution might be the transfer of such populations from one country to another—with better prospects in terms of COVID-19 infection and mortality rates.
Finally, referring to strict public policy measures such as lockdowns, an interesting debate emerged regarding the effectiveness of such measures. On the one hand, Coccia (2023) suggests that the substantial social and economic costs associated with high levels of strict restriction policies may provide limited benefits in terms of controlling the spread and negative impact of pandemics. On the other hand, Diao et al. (2020) point out that the effect of population density was almost nonexistent in China due to the implementation of strict lockdowns. In contrast, decay duration demonstrated the highest correlation with population density, absolute humidity, and maximum temperature in England, Germany, and Japan. Also, the United Nation Committee for Development Policy (2021) stresses an overlooked reason for the outcome, according to which less developed countries (LDC) account for 14% of the world population, but only 2% of the COVID-19 cases. This unnoticed reason is the immediate implementation of lockdowns and travel restrictions by governments in less developed countries (page 2).
Methods
Sample and data
Information for this study spans five continents (Africa, Asia, Europe, America, Oceania) and encompasses 162 countries,Footnote 2 from January 22, 2020, to January 21, 2022. This yields 109,813 (109,322) observations with the availability of information on the total COVID-19 cases (deaths) per 1 million persons. Yet the data structure permits variations across both time and space only for these two variables. The rest of the explanatory variables vary among countries, but not across time.
Measures of variables
Table 1 reports the descriptive statistics of the variables, which are subsequently incorporated into the empirical model. The table is divided into two parts. The upper (lower) part includes the descriptive statistics of observations for which information on total COVID-19 cases (deaths) per 1 million persons is available. The sample mean of COVID-19 cases (deaths) is 25,371.90 (491.52) per million persons and the sample median is 5057.098 (120.273). The implication is right-tailed distributions of both variables, namely positive skewness of 2.244 (2.501). The standard deviation equals 39,671.99 COVID-19 cases (766.664 COVID-19 deaths) per 1 million persons. The maximum scope of morbidity (mortality) is obtained in Seychelles Islands (Peru) with 347,457.30 cases (6115.035 deaths) per 1 million persons.
Referring to the number of hospital beds in each country, the sample mean is 2.959–2.977 beds, and the sample median is 2.32. Once again, right-tailed distributions are obtained (positive skewness of 1.5345), with an implicit low number of hospital beds per thousand persons. The standard deviation is 2.36–2.37 hospital beds per thousand persons. The maximum (minimum) number of beds per thousand persons is obtained in Japan (Mali) with 13.05 (0.1) beds per thousand persons.
Referring to the population density variable, the sample mean is 204–205 persons per square kilometer, and the sample median is 82.805–82.6. Once again, right-tailed distributions are obtained (positive skewness of 10.41), with an implicit low population density prevalence. The standard deviation is 671.5761–674.1418 persons per square kilometer. The maximum (minimum) population density is obtained in Singapore (Mongolia) with 7915.73 (1.98) persons per square kilometer.
Finally, referring to the median age of the country, the sample mean is 31.438–31.639 years, and the sample median is 31.4–31.6. Unlike other variables, for the age variable, the null hypothesis of symmetrical distribution cannot be rejected (p = 0.8796 for 162 countries, where, according to the null hypothesis, the skewness equals zero). The standard deviation is 8.869–8.905 years. The maximum (minimum) median age is obtained in Japan (Niger) with 48.2 (15.1) years.
Model and data analysis procedure
Following Papke and Wooldridge (1996) and Wooldridge (2010), consider the following maximum likelihood function of the fractional probit regression:
where \({y}_{1,j}=Total\_cases\_per\_million\) and \({y}_{2,j}=Total\_deaths\_per\_million\);
\(\Phi \left(\bullet \right)\) is the standard normal cumulative density function, and \({\widehat{\alpha }}_{1},{\widehat{\alpha }}_{2},{\widehat{\alpha }}_{3},{\widehat{\alpha }}_{4}\) and \({\widehat{\beta }}_{1},{\widehat{\beta }}_{2},{\widehat{\beta }}_{3},{\widehat{\beta }}_{4}\) are estimated parameters (the circumflexes denote the estimated parameters).
It may be readily verified that (1) a global minimum is achieved if \({\widehat{\alpha }}_{2}>0\) and \({\widehat{\beta }}_{2}>0\); (2) the vaccination rates that yield the minimum scope of COVID-19 morbidity are as follows: \(-\frac{{\widehat{\alpha }}_{1}}{2{\widehat{\alpha }}_{2}}\) and \(-\frac{{\widehat{\beta }}_{1}}{2{\widehat{\beta }}_{2}}\); and (3) the minimum scope of morbidity is obtained by substitution of \(-\frac{{\widehat{\alpha }}_{1}}{2{\widehat{\alpha }}_{2}}\) and \(-\frac{{\widehat{\beta }}_{1}}{2{\widehat{\beta }}_{2}}\) in the respective estimated Eqs. (2) and (3) and the conversion to the cumulative normal distribution probabilities.Footnote 3
Based on this estimation procedure, we identify the country with the lowest anticipated likelihood of COVID-19 infection and mortality for each category (hospital beds, population density, and median age of the country’s population). To trace the optimal place in terms of COVID-19 infection and mortality, we then generate the projected probability of infection and mortality for each country and rank them based on these projected probabilities. The outcomes of these ranking procedures are given in Appendix Tables 4 and 5.
Results
Table 2 reports the regression outcomes, and based on these results, Figs. 1, 2, and 3 depict the projected probabilities multiplied by 1 million with respect to the three explanatory variables separately.
Predicted COVID-19 vs. hospital beds per thousand. Notes: Based on the fractional probit regression outcomes reported in columns (1) and (3) in Table 2. The procedure is applied to information regarding 162 countries around the world provided by the World Health Organization (WHO) and spans from January 22, 2020, to January 21, 2022. Predicted values are multiplied by a factor of 1 million
Predicted COVID-19 vs. median age. Notes: Based on the fractional regression outcomes reported in columns (1) and (3) in Table 2. The procedure is applied to information regarding 162 countries around the world provided by the World Health Organization (WHO) and spans from January 22, 2020, to January 21, 2022. Predicted values are multiplied by a factor of 1 million
Figure 1 demonstrates that referring to the number of hospital beds per thousand persons, and like population density (e.g., Hamidi et al. 2020), one should consider two opposing forces. On the one hand, congestion in hospitals and healthcare centers may be a source of elevated infection (Jayaweera and Reyes 2019; Ngandu et al. 2022). This, in turn, might increase morbidity and mortality particularly during periods with high occupancy rates. On the other hand, more hospital beds are associated with better medical infrastructure and increased prospects of COVID-19 recovery. Indeed, as the figure demonstrates, an increase from one to five (four) hospital beds per thousand persons is associated with a projected increase in the anticipated scope of morbidity (mortality) from 20,090 (421) to a maximum of 31,057 (575) cases (deaths) per 1 million persons. Starting from the sixth (fifth) hospital bed and until a maximum of 13 beds per thousand persons, the anticipated scope of morbidity (mortality) drops until a minimum of 2000 (67.4) COVID-19-infected (dead) per 1 million persons.Footnote 4
Figure 1 thus demonstrates, that under equal conditions, the minimum scope of morbidity and mortality at a country level is achieved by the maximum of 13 hospital beds per thousand persons. The leading countries according to this criterion are Japan (13.05 beds per thousand persons) and South Korea (12.27 beds per thousand persons).
Figure 2 indicates, under equal conditions, the anticipated drop in the scope of morbidity (mortality) with increased population density. When population density is at a minimum of 2 persons per square kilometers, the anticipated scope of morbidity (mortality) is 25,867.5 (545) COVID-19 cases (deaths) per 1 million persons. As population density rises to the maximum of 8000 persons per square kilometer, the anticipated scope of morbidity (mortality) is 12,221 (2.57) COVID-19 cases (deaths) per 1 million persons. This outcome of the negative association between the scope of morbidity (mortality) and population density at a global level supports Hamidi et al. (2020). This may be explained on the grounds that the positive agglomeration effects in denser cities (higher prospects of observing health safety measures and calling emergency services; better medical infrastructure in denser cities) overcome the negative effects (more interactions between people, which, in turn, reinforces infections).
Appendix Tables 4 and 5 rank the optimal countries in terms of the predicted likelihood of COVID-19 infection and mortality. The lowest likelihood of infection is obtained in Niger (3684 anticipated cases per 1 million persons) and Mali (3830 anticipated cases per 1 million persons). As Appendix Table 4 indicates, both countries are at the lowest scale of the median age, namely 15.1–16.4 years, which, in turn, yields the lowest COVID-19 infection rates. Yet, in terms of population density and the number of hospital beds per thousand persons, both countries are at the lowest 5–10 percentiles with a population density of 15.196–16.955 persons per square kilometer and 0.1–0.3 beds per thousand persons. Unlike the median age, the numerical values of both of these variables predict higher than the optimal COVID-19 infection rates.
Appendix Table 5 shows that the lowest likelihood of mortality is obtained in Singapore (2.35 anticipated deaths per 1 million persons) and Burundi (104.6 anticipated deaths per 1 million persons – \(\frac{104.6}{2.35}=\) 44.51 times more than the optimal country). As Appendix Table 5 indicates, Singapore has the highest population density (7915 persons per square kilometer), while Burundi has the lowest median age variable (17.5 years). This, in turn, yields the lowest COVID-19 mortality rates. Yet, in terms of median age, Singapore is located at the 75–90% percentile with 42.4 years, and, in terms of the number of hospital beds, slightly above the median percentile with 2.4 beds per thousand persons. Unlike the population density, the numerical values of both of these variables predict higher than the optimal COVID-19 mortality rates.
An interesting outcome obtained from this analysis is the fact that the advantages of denser countries (e.g., better infrastructure, better accessibility to medical centers and facilities, and higher prospects of getting health treatment much faster compared to more sparsely populated countries) might outweigh the disadvantages (more interactions with people, which, in turn, increase the prospects of infections, crime, traffic jams, pollution). Given the more limited possibility to control the median age, and the less constrained possibility to control population density by choice of residence in the short run, this outcome might prove to be important.Footnote 5
Robustness tests
One concern that should be addressed is the skewness of the dependent variables’ total COVID-19 cases (deaths) per 1 million persons and the symmetry of the random disturbance terms. The relevant statistical tests clearly indicate the rejection of the null hypothesis of zero skewness. Figure 4 provides histograms of these dependent variables. Both clearly exhibit right-tailed distributions. Infection rates among 53% of the world countries are only 6322.8 cases per 1 million persons, and among less than 1% of the world countries are 350,000 cases per 1 million persons. The mortality rates among 50% of the world countries are 115.325 deaths per 1 million persons, and among less than 1% of the world countries are 6200 deaths per 1 million persons.
Histograms of COVID-19 cases and deaths per 1 million persons. Notes: The graph refers to information regarding 162 countries around the world provided by the World Health Organization (WHO), and spans from January 22, 2020, to January 21, 2022. Infection rates among 53% of the world countries is only 6,322.8 cases per 1 million persons and among less than 1 percent of the world countries is 350,000 cases per 1 million persons. Mortality rates among 50% of the world countries are 115.325 deaths per 1 million persons and among less than 1% of the world countries are 6200 deaths per 1 million persons
These concerns may be addressed by using the Poisson regression (Greene 2012: 842–855; Msemburi et al. 2023). This methodology is particularly suitable for the counts of events, such as the total COVID-19 cases and deaths per 1 million persons and the number of hospital beds. Riphahn et al. (2003), for instance, employed this methodology by investigating count data variables (the number of hospital and doctor visits). Greene (2012: 851) provides the histogram of the latter variable and demonstrate a clear right-tailed distribution, very similar to those reported in Fig. 4.
According to Greene (2012), the Poisson model specifies that each \({y}_{i}\) (\({y}_{i}=\mathrm{0,1},\mathrm{2,3},\cdots\)) is drawn from a Poisson population with \({\lambda }_{i}\) parameters related to \({x}_{i}\) regressors in the following manner:
\(Prob\left({y}_{i}|{x}_{i}\right)=\frac{{e}^{{-\lambda }_{i}}{{\lambda }_{i}}^{{y}_{i}}}{{y}_{i}!}\) where \(ln{\lambda }_{i}={x}_{i}^{^{\prime}}\beta\). The corresponding log-likelihood function to be maximized is:\(lnL=\sum_{i=1}^{n}\left[-{\lambda }_{i}+{y}_{i}{x}_{i}^{^{\prime}}\beta -ln\left({y}_{i}!\right)\right]\) and the first order conditions are:
A well-known criticism of the Poisson regression is the assumed equality of the conditional mean and variance functions. This problem may be addressed by the negative binomial regression model. The introduction of an individual unobserved effect \(\left({\epsilon }_{i}\right)\) to the conditional mean yields:\(ln{\mu }_{i}={x}_{i}^{^{\prime}}\beta +{\epsilon }_{i}=ln{\lambda }_{i}+ln{u}_{i}\) and the corresponding density function is:
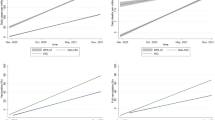
The estimation results of the Poisson and negative binomial regressions are given in Table 3. Based on the Poisson regressions given in column 1 (columns 2) in Table 3, Fig. 5 (Fig. 6) provides the predicted number of COVID-19 cases (deaths) per 1 million persons as a function of the number of hospital beds per 1000 persons per country. Results are robust to previous outcomes and show a rise from 20,000 to a maximum of 32,000 predicted cases (400 to a maximum of 560 predicted deaths) and a drop from 32,000 to 2000 predicted cases (560 to 100 predicted deaths) per 1 million persons with the number of hospital beds.
Predicted number of COVID-19 mortality events per 1 million persons. Notes: Based on Columns (1) and (2) in Table 3, where the dependent variable is total COVID-19 cases/deaths per 1 million persons. The Poisson procedure is applied to information regarding 162 countries around the world provided by the World Health Organization (WHO) and spans from January 22, 2020, to January 21, 2022
Conclusions
During the past 2 years, the COVID-19 global pandemic affected countries around the world in different ways (e.g., Alperovich 1984; Newman 2005; Nitsch 2005; Blasius 2020; Arbel et al. 2022). The magnitude and severity of the spread vary based on different characteristics. The current study tests three important features, identified in the literature, namely median age (e.g., Hägg 2020; O’Driscoll et al. 2021; Petrilli et al. 2020), population density (e.g., Hamidi et al. 2020; Souris and Gonzalez 2020), and per capita hospital beds (Souris and Gonzalez 2020; Docherty et al. 2021; Grosso et al. 2021).
Following the evolvement of distinct variants, the pandemic included several waves. Coping with each variant is slightly different. However, given the contagious nature of the pandemic, a conventional measure is the avoidance or, at least reduction, of interactions among people and keeping a safe distance from one another. According to the World Health Organization (WHO) coronavirus (COVID-19) dashboard, as of March 25, 2022, the scope of morbidity is 476,374,234 cases (\(\frac{\mathrm{476,374,234}}{\mathrm{7,900,000,000}}=6.03\%\) of the world population) and the extent of mortality is 6,108,976 persons (\(\frac{\mathrm{6,108,976}}{\mathrm{7,900,000,000}}=0.0733\%\) of the world population).
In coping with the disease, every country has its own advantages and disadvantages. This raises the question of what the optimal country with respect to the scope of morbidity and mortality from the SARS-CoV2 is (the virus responsible for the COVID-19 pandemic). Differently put, for uninfected persons, which country has the lowest prospects for COVID-19 morbidity? Having become infected with the SARS-CoV2 virus, which country has the lowest prospects of COVID-19 mortality?
Findings suggest that for individuals who were not infected by the SAR-COV2 virus, the optimal country would be Niger or Mali, the countries with the lowest prospects of morbidity per million persons. Yet, to reduce the prospects of mortality for individuals who were already infected by the SAR-COV2 virus, the optimal country would be Singapore.
Another important finding is the drop in morbidity and mortality rates with an increased number of hospital beds where the median age and population density of the country are controlled. This is an important outcome which is in line with Coccia (2021). The author derives four strategic ways to address future pandemics. Those include the following: (1) Increasing health expenditure above 7.6% of the GDP, (2) increasing government health expenditure above $2000 per capita, (3) policies aimed to reduce air pollution to a maximum of 50 days per annum, (4) rather than extensive quarantine and lockdowns policies, timely applications of containment policy in susceptible places in terms of morbidity and mortality, (5) vaccination plans. Given that the number of hospital beds is a proxy for the extent of health expenditures, the empirical evidence we provide is consistent with four of Coccia’s recommendations regarding the required increase in health expenditure, timely applications of the containment policy, and vaccination plans. Referring to vaccination plans, for instance, those require additional health budgets for the good deployment of the health system facilities and vaccine acquirements. Moreover, Hradsky and Komarek (2021) concluded that in particular countries, the number of people who will die from COVID-19 is largely given by factors that cannot be drastically changed as an immediate reaction to the pandemic and authorities should focus on modifiable variables, such as the number of hospital beds.
Referring to our findings, the outcomes consistently show an initial attenuated increase in projected morbidity and mortality rates with more hospital beds per thousand persons followed by a steep decrease starting from the fifth hospital bed per thousand persons. The initial rise may be explained by Pablos-Méndez et al. (2022). The authors compared western and eastern countries. The west experiences a much higher COVID-19 mortality than the east. Despite structural advantages in the west, such as better health infrastructure, delays in national responses early on resulted in a loss of control over the spread of SARS-CoV-2. Although the early success of the East was sustained in the second half of 2020, the region remains extremely vulnerable to COVID-19 until enough people are immunized. Given that the study data timeframe spans from January 2000 to January 2022, the initial projected morbidity and mortality rise reflects the deterioration in the morbidity and mortality data of the Eastern countries with time. Compared to the western countries, the health infrastructure in these countries is worse. This is reflected in lower numbers of hospital beds per thousand persons.
The contribution of this article lies in the possibility to generate a new policy tool in the face of future global pandemics based on real-life data. In that respect, we can rank the optimal countries and attempt to study from their experience in an effort to address future pandemics. One of the important lessons that emanate from the empirical evidence might be the need to extend budget spending on health and cooperation across states in emergency situations. In light of the related limitations, it is difficult to prevent the spread of future pandemics. However, coordination between countries and the establishment of international medical professional teams for the management of the crisis—such as the treatment of earthquakes—the establishment of field hospitals, testing laboratories, isolation of areas, humanitarian aid in infected areas, and international studies with prioritization and incentives for the same issue might be considered as an effective public policy.
A potential limitation of our study is the fact that the investigation is carried out throughout the COVID-19 pandemic. In light of the different nature of each wave, it is possible that the optimal ranking would vary following different COVID-19 waves. This is, however, a subject for future research.
Another limitation of our study is the lack of control on the extent of COVID-19 testing. It is possible that compared to less developed countries, COVID-19 detection in European countries is higher due to the widespread testing. This limitation, however, may be addressed as follows:
-
The world today is exposed to satellite detection and other technological means. It would either be impossible or very difficult to hide data about epidemics. In that context, and based on satellite images obtained via search engines, Nsoesie et al. (2020) were able to indicate early disease activity in the Fall of 2019 in Wuhan China, which is considered the source of the COVID-19 outbreak.
-
This point may indeed be considered one of the limitations of the current study. Indeed, the lack of a testing system may create a distortion. Yet, given the spread of the pandemic, which cannot be avoided, a reasonable assumption is the small magnitude of this distortion. Differently put, people have a pretty good evaluation of how many patients are there.
-
A study at the beginning of the pandemic (Sambridge and Jackson 2020) supports the credibility of early global data on COVID-19 morbidity and mortality events. The Benford’s law states that for numbers that consist of at least three digits, the theoretical probability of appearance of \(n=\mathrm{1,2},\mathrm{3,4},\mathrm{5,6},\mathrm{7,8},9\) as the first digit from the left is \({\mathrm{log}}_{10}\left[\frac{n+1}{n}\right]\). The implication is that the modal digit is one (approximate theoretical probability of appearance of 30%).Footnote 6 This law may be employed to reveal data anomalies and frauds. For instance, Fig. 3 in Sambridge and Jackson (2020) demonstrates that the appearance of the digit 9 in the Czech Republics’ COVID-19 mortality reports is unproportionate. Yet a global level analysis given in Fig. 4 demonstrates a Pearson correlation of 100% between the theoretical and actual Benford distribution.
-
As Arbel et al. (2022, 2023) and Pablos-Méndez et al. (2022) indicate, in addition to median age, significant correlates of COVID-19 infection and mortality in countries with at least 1 million population was the democracy index. In autocratic countries, there is more compliance with the COVID-19 restrictions due to a fear of the regime. This approach is also supported in the UN report from April 2021 regarding LDC (less-developed countries). The report stresses the fact that while LDC accounts for 14% of the world population, they account for only 2% of the COVID-19 cases. The report stresses that an overlooked reason for this outcome is the immediate implementation of lockdowns and travel restrictions by governments in less developed countries (page 2).
-
According to the UN report from April 2021, one hypothesis referring to the low COVID-19 infection rates in less developed countries is the lower availability of tests. Referring to this claim, on the one hand, indeed, this is true in a large portion of LDC. On the other hand, in the few less developed countries that implemented extensive testing policies (e.g., Bhutan and Rwanda), COVID-19 infection rates still remained low. Moreover, overall policy responses have been found to be a stronger explanatory factor than low testing, poor health systems, or underreporting of COVID-19 cases (Chitungo et al. 2020).
-
Referring specifically to Singapore, which is ranked first in our study in terms of the projected number of COVID-19 infected per 1 million persons, according to the US freedom house measures of democracies, it is considered only partly free, or more autocratic compared to Western countries (e.g., Arbel et al. 2022). As previously noted, in addition to other factors, the regime type might also explain the low COVID-19 mortality rates in Singapore (if the system is sufficiently effective to impose high compliance levels to social distancing rules).
Data availability
This research is based on information downloaded from the World Health Organization website. After acceptance of the manuscript, full information and replication instructions in Stata software package will be given upon request.
Notes
The source of this dataset is the World Heath Organization (WHO) available at https://ourworldindata.org/coronavirus#coronavirus-country-profiles
The database is obtained from the World Health Organization (WHO) website at https://ourworldindata.org/coronavirus#coronavirus-country-profiles. A full list of countries and their rankings are given at Appendix Tables 4 and 5.
See, for example Chiang and Wainwright (2005). On page226, the authors ask to find the relative extremum of the function, \(AC\left(Q\right)=f\left(Q\right)=a{Q}^{2}+bQ+c\) where \(a=1,b=-5\) and \(c=8\). Setting the first derivative to zero gives \({f}^{^{\prime}}\left(Q\right)=2aQ+b=0\), which has the single root \({Q}^{*}=-\frac{b}{2a}=-\frac{-5}{2\times 1}=2.5\) and a minimum cost of \(f\left(Q=2.5\right)={2.5}^{2}-5\times 2.5+8=1.75\). Substitution of \(Q=2.4\) and \(Q=2.6\) (the neighborhood of \({Q}^{*}=2.5\)) in the first derivative yields \({f}^{^{\prime}}\left(Q=2.4\right)=-0.2<0\) and \({f}^{^{\prime}}\left(Q=2.6\right)=0.2>0\). This demonstrates a local minimum. Moreover, on page 231, the authors demonstrate that while \(a>0\) give rise to a U-shaped curve, namely an absolute minimum, \(a<0\) give rise to an inverted U-shaped curve, namely an absolute maximum, Consequently, the point \(\left(\mathrm{2.5,1.75}\right)\) is a global minimum.
Note also that the same anticipated scope of morbidity (mortality) is achieved for 1 and 8.21 hospital beds per thousand persons (1 and 7.74 hospital beds per thousand persons).
In the long run, median age may be controlled by natural reproduction or immigration of younger populations.
As an intuitive example, consider, for instance a street where the addresses are numbered at consecutive digits \(\mathrm{1,2},\mathrm{3,4},\cdots ,19\). While the probability of appearance of the digit one as the most left digit is \(\frac{11}{19}\) (street numbers \(\mathrm{1,11,12,13,14,15},\cdots ,19\)), the probability of appearance of every other of the eight remaining digits is \(\frac{1}{19}\).
References
Alperovich G (1984) The size distribution of cities: on the empirical validity of the rank-size rule. J Urban Econ 16:232–239
Arbel Y, Fialkoff C, Kerner A, Kerner M (2022) Do population density, socio-economic ranking and Gini Index of cities influence infection rates from coronavirus? Israel as a case study. Annals of Regional Science 68,181–206. https://doi.org/10.1007/s00168-021-01073-y
Arbel Y, Arbel Y, Kerner A, Kerner M, Can the Regime type (democracy versus autocracy) explain the COVID 19 recovery rates? Chinese Political Science Review, Accepted on January 31, 2022
Arbel Y, Arbel Y, Kerner A, Kerner M (2023) To obey or not to obey? Can game theory explain human behavior in the context of coronavirus disease? Rev Dev Econ:1–14. https://doi.org/10.1111/rode.12979
Benati I, Coccia M (2022) Global analysis of timely COVID-19 vaccinations: Improving governance to reinforce response policies for pandemic crises. Int J Health Gov. https://doi.org/10.2139/ssrn.4124257
Blasius B (2020) Power-law distribution in the number of confirmed COVID-19 cases. Available at: https://arxiv.org/pdf/2004.00940.pdf. Accessed 24 Mar 2023
Bontempi E, Coccia M (2021) International trade as critical parameter of COVID-19 spread that outclasses demographic, economic, environmental, and pollution factors. Environ Res 201:111514. https://doi.org/10.1016/j.envres.2021.111514
Bontempi E, Coccia M, Vergalli S, Zanoletti A (2021) Can commercial trade represent the main indicator of the COVID-19 diffusion due to human-to-human interactions? A comparative analysis between Italy, France, and Spain. Environ Res 201:111529. https://doi.org/10.1016/j.envres.2021.111529
Chiang A, Wainwright K (2005) Fundamental methods of mathematical economics. McGraw Hills International Edition, Printed in Singapore
Chitungo I, Dzobo M, Hlongwa M, Dzinamarira T (2020) COVID-19: Unpacking the low number of cases in Africa. Public Health Pract (Oxf) 1:100038 https://doi.org/10.1016/j.puhip.2020.100038
Coccia M (2020) Comparative critical decisions in management. In: Farazmand A (ed) Global encyclopedia of public administration, public policy, and governance. Springer, Cham. https://doi.org/10.1007/978-3-319-31816-5_3969-1
Coccia M (2021) Pandemic prevention: lessons from COVID-19. Encyclopedia 1(2):433–444. https://doi.org/10.3390/encyclopedia1020036
Coccia M (2022a) Preparedness of countries to face COVID-19 pandemic crisis: strategic positioning and underlying structural factors to support strategies of prevention of pandemic threats. Environ Res 203:111678. https://doi.org/10.1016/j.envres.2021.111678
Coccia M (2022b) Optimal levels of vaccination to reduce COVID-19 infected individuals and deaths: a global analysis. Environ Res 204(Part C):112314. https://doi.org/10.1016/j.envres.2021.112314
Coccia M (2022c) Improving preparedness for next pandemics: Max level of COVID-19 vaccinations without social impositions to design effective health policy and avoid flawed democracies. Environ Res 213:113566. https://doi.org/10.1016/j.envres.2022.113566
Coccia M (2022d) COVID-19 Vaccination is not a sufficient public policy to face crisis management of next pandemic threats. Public Organiz Rev 1–15. https://doi.org/10.1007/s11115-022-00661-6
Coccia M (2023) Effects of strict containment policies on COVID-19 pandemic crisis: lessons to cope with next pandemic impacts. Environ Sci Pollut Res Int 30(1):2020–2028. https://doi.org/10.1007/s11356-022-22024-w
Diao Y, Kodera S, Anzai D, Gomez-Tames J, Rashed EA, Hirata A (2020) Influence of population density, temperature, and absolute humidity on spread and decay durations of COVID-19: A comparative study of scenarios in China, England, Germany, and Japan. One Health 12:100203. https://doi.org/10.1016/j.onehlt.2020.100203
Docherty AB, Mulholland RH, Lone NI, Cheyne CP, De Angelis D, Diaz-Ordaz K, Donegan C, Drake TM, Dunning J, Funk S, García-Fiñana M, Girvan M, Hardwick HE, Harrison J, Ho A, Hughes DM, Keogh RH, Kirwan PD, Leeming G, Nguyen Van-Tam JS (2021) Changes in in-hospital mortality in the first wave of COVID-19: a multicentre prospective observational cohort study using the WHO Clinical Characterisation Protocol UK. Lancet Respir Med 9(7):773–785. https://doi.org/10.1016/S2213-2600(21)00175-2
Dowd JB, Andriano L, Brazel DM, Rotondi V, Block P, Ding X, Liu Y, Mills MC (2020) Demographic science aids in understanding the spread and fatality rates of COVID-19. Proc Natl Acad Sci USA 117(18):9696–9698
Flaxman S, Mishra S, Gandy A et al (2020) Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature 584:257–261. https://doi.org/10.1038/s41586-020-2405-7
García YE, Mery G, Vásquez P, Calvo JG, Barboza LA, Rivas T, Sanchez F (2022) Projecting the impact of COVID-19 variants and vaccination strategies in disease transmission using a multilayer network model in Costa Rica. Sci Rep 12(1):1–9. https://doi.org/10.1038/s41598-022-06236-1
Greene WH (2012) Econometric analysis, Seventh Edition. Pearson Education Limited: 842–855
Grosso FM, Presanis AM, Kunzmann K, Jackson C, Corbella A, Grasselli G, Andreassi A, Bodina A, Gramegna M, Castaldi S, Cereda D, Angelis DD, Covid-19 Lombardy Working Group, Castrofino A, Del Castillo G, Crottogini L, Tirani M, Zanella A, Salmoiraghi M (2021) Decreasing hospital burden of COVID-19 during the first wave in Regione Lombardia: an emergency measures context. BMC Public Health 21(1):1–9. https://doi.org/10.1186/s12889-021-11669-w
Hägg S, Jylhävä J, Wang Y, Xu H, Metzner C, Annetorp M, Garcia-Ptacek S, Khedri M, Boström A-M, Kadir A, Johansson A, Kivipelto M, Eriksdotter M, Cederholm T, Religa D (2020) Age, frailty, and comorbidity as prognostic factors for short-term outcomes in patients with coronavirus disease 2019 in geriatric care. J Am Med Dir Assoc 21(11):1555–1559
Hamidi S, Ewing R, Sabouri S (2020) Longitudinal analyses of the relationship between development density and the COVID-19 morbidity and mortality rates: Early evidence from 1,165 metropolitan counties in the United States. Health Place 64:102378. https://doi.org/10.1016/j.healthplace.2020.102378
Hradsky O, Komarek A (2021) Demographic and public health characteristics explain large part of variability in COVID-19 mortality across countries. Eur J Public Health 31(1):12–16. https://doi.org/10.1093/eurpub/ckaa226
Jayaweera JAAS, Reyes M (2019) Childhood nosocomial viral acute respiratory tract infections in teaching hospital Anuradhapura, Sri Lanka. BMC Res Notes 12(1):1–5. https://doi.org/10.1186/s13104-019-4624-2
Kim YC, Dema B, Reyes-Sandoval A (2020) COVID-19 vaccines: breaking record times to first-in-human trials. NPJ Vaccines 5:34. https://doi.org/10.1038/s41541-020-0188-3
Martinez-Bravo M, Gerard PIM, Qian N, Yao Y (2012) The effects of democratization on public goods and redistribution: evidence from China. http://www.nber.org/papers/w18101.pdf. Accessed 24 Mar 2023
Msemburi W, Karlinsky A, Knutson V, Aleshin- Guendel S, Chatterji S, Wakefield J (2023) The WHO estimates of excess mortality associated with the COVID-19 pandemic. Nature 613(7942):130–137. https://doi.org/10.1038/s41586-022-05522-2
Newman MEJ (2005) Power laws, Pareto distributions and Zipf’s law. Contemp Phys 46(5):323–351
Nitsch V (2005) Zipf zipped. J Urban Econ 57(2005):86–100
Ngandu NK, Mmotsa TM, Dassaye R, Thabetha A, Odendaal W, Langdown N, Ndwandwe D (2022) Hospital acquired COVID-19 infections amongst patients before the rollout of COVID-19 vaccinations, a scoping review. BMC Infect Dis 22(1):140. https://doi.org/10.1186/s12879-022-07128-5
Nsoesie EO, Rader B, Barnoon YL, Goodwin L, Brownstein JS (2020) Analysis of hospital traffic and search engine data in Wuhan China indicates early disease activity in the Fall of 2019. Retrieved from: https://dash.harvard.edu/handle/1/42669767. Accessed 24 Mar 2023
Núñez-Delgado A, Bontempi E, Coccia M, Kumar M, Farkas K, Domingo JL (2021) SARS-CoV-2 and other pathogenic microorganisms in the environment. Environ Res 201:111606. https://doi.org/10.1016/j.envres.2021.111606
O’Driscoll M, Ribeiro Dos Santos G, Wang L, Cummings DAT, Azman AS, Paireau J, Fontanet A, Cauchemez S, Salje H (2021) Age-specific mortality and immunity patterns of SARS-CoV-2. Nature 590(7844):140–145. https://doi.org/10.1038/s41586-020-2918-0
Pablos-Méndez A, Villa S, Monti MC, Raviglione MC, Tabish HB, Evans TG, Cash RA (2022) Global ecological analysis of COVID-19 mortality and comparison between “the East” and “the West.” Sci Rep 12(1):5272. https://doi.org/10.1038/s41598-022-09286-7
Papke LE, Wooldridge JM (1996) Econometric methods for fractional response variables with an application to 401(k) plan participation rates. J Appl Economet 11:619–632
Petrilli CM, Jones SA, Yang J, Rajagopalan H, O'Donnell L, Chernyak Y, Tobin KA, Cerfolio RJ, Francois F, Horwitz LI (2020) Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ 369:m1966. https://doi.org/10.1136/bmj.m1966
Riphahn RT, Wambach A, Million A (2003) Incentive effects in the demand for health care: a bivariate panel count data estimation. J Appl Economet 18(4):387–405
Sambridge M, Jackson A (2020) National COVID numbers — Benford’s law looks for errors. Nature: International Weekly Journal of Science 581(7809):384
Souris M, Gonzalez J-P (2020) COVID-19: Spatial analysis of hospital case-fatality rate in France. PLoS ONE 15(12):e0243606. https://doi.org/10.1371/journal.pone.0243606
Tomer V, Gupta S, Manwal M, Singh DP (2021) How statistics of world health index react against COVID-19. Mater Today Proceed 46:11267–11273. https://doi.org/10.1016/j.matpr.2021.03.486
United Nation Committee for Development Policy (2021) Comprehensive study on the impact of COVID19 on the least developed country category. Available at: https://www.un.org/development/desa/dpad/wp-content/uploads/sites/45/publication/CDP_Comprehensive_Study_2021.pdf (Last Accessed on March 2, 2023)
Wooldridge JM (2010) Econometric analysis of cross section and panel data, 2nd edn. MIT Press, Cambridge
World Health Organization (WHO) Coronavirus (COVID-19) dashboard, available at: https://covid19.who.int/ (last accessed on March 26, 2022)
World Health Organization (WHO) (n.d.) Coronavirus pandemic. Available at: https://ourworldindata.org/coronavirus#coronavirus-country-profiles
Yuan J, Li M, Lv G, Lu ZK (2020) Monitoring transmissibility and mortality of COVID-19 in Europe. Int J Infect Dis 95:311–315. https://doi.org/10.1016/j.ijid.2020.03.050
Acknowledgements
The authors are grateful to Chaim Fialkoff for his helpful comments.
Author information
Authors and Affiliations
Contributions
Yuval Arbel contributed to the study conception and design, data collection and analysis, the first draft, and comments on previous versions of the manuscript. Yifat Arbel contributed to the study conception and design, data collection and analysis, the first draft, and comments on previous versions of the manuscript. Amichai Kerner contributed to the study conception and design, data collection and analysis, the first draft, and comments on previous versions of the manuscript. Miryam Kerner contributed to the study conception and design, data collection and analysis, the first draft, and comments on previous versions of the manuscript. All authors read and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval
Not applicable. This research does not require an IRB approval since it does not involve any experiment or manipulation of subjects.
Consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Arbel, Y., Arbel, Y., Kerner, A. et al. What is the optimal country for minimum COVID-19 morbidity and mortality rates?. Environ Sci Pollut Res 30, 59212–59232 (2023). https://doi.org/10.1007/s11356-023-26632-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-023-26632-y