Abstract
The Wells-Riley model invokes human physiological and engineering parameters to successfully treat airborne transmission of infectious diseases. Applications of this model would have high potentiality on evaluating policy actions and interventions intended to improve public safety efforts on preventing the spread of COVID-19 in an enclosed space. Here, we constructed the interaction relationships among basic reproduction number (R0) − exposure time − indoor population number by using the Wells-Riley model to provide a robust means to assist in planning containment efforts. We quantified SARS-CoV-2 changes in a case study of two Wuhan (Fangcang and Renmin) hospitals. We conducted similar approach to develop control measures in various hospital functional units by taking all accountable factors. We showed that inhalation rates of individuals proved crucial for influencing the transmissibility of SARS-CoV-2, followed by air supply rate and exposure time. We suggest a minimum air change per hour (ACH) of 7 h−1 would be at least appropriate with current room volume requirements in healthcare buildings when indoor population number is < 10 and exposure time is < 1 h with one infector and low activity levels being considered. However, higher ACH (> 16 h−1) with optimal arranged-exposure time/people and high-efficiency air filters would be suggested if more infectors or higher activity levels are presented. Our models lay out a practical metric for evaluating the efficacy of control measures on COVID-19 infection in built environments. Our case studies further indicate that the Wells-Riley model provides a predictive and mechanistic basis for empirical COVID-19 impact reduction planning and gives a framework to treat highly transmissible but mechanically heterogeneous airborne SARS-CoV-2.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Enclosed environments are among the most common venues that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is transmitted (Qian et al. 2021). Cumulative evidence showed that airborne transmission is associated with micron-scale aerosol droplets that could inevitably occur in confined spaces (Bazant and Bush 2021; Jayaweera et al. 2020; Mittal et al. 2020; Morawska and Milton 2020; Zhang et al. 2020). Among all kinds of built environments, increasing studies have found that hospitals could be one of the hotbeds cultivating super spreaders due to the higher risks resulting from intensive contacts of healthcare workers with infectors and congregations of inpatients, outpatients, and visitors from various places (Huang et al. 2022; Illingworth et al. 2021; Wei et al. 2020). However, in addition to source controls (e.g., social distancing and wearing of face mask), there has been limited knowledge in other mitigation measures such as applications of engineering controls (e.g., air supply rate and room volume) on disease transmissions in hospitals or healthcare facilities (Allen and Ibrahim 2021).
The main routes for SARS-CoV-2 transmission in hospitals are suggested to be direct transfer of respiratory droplets (e.g., coughing, sneezing, saliva, handling mucous membranes from mouth, nose, and eyes) (Lu et al. 2020; To et al. 2020) or indirect transfer through contaminated surfaces where virus remains for several days (Doremalen et al. 2020). Between the two transmission routes, airborne transmission through inhalation of aerosol droplets exhaled by an infected person is now thought to be the primary transmission route of SARS-CoV-2 (Bazant and Bush 2021). Therefore, effective containments on disease transmissions intraunits/interunits of hospital buildings are highly recommended. It is also of great essence to clearly understand the role or impacts of indoor settings on the transmissibility of SARS-CoV-2.
Although there have been guidelines or standards covering air exchange rates in various kinds of spaces or healthcare facilities (AIA 2001; ASHRAE 2020; TAHPI 2015), these standards may not be applicable for disease containments when more patients/visitors are present in hospitals or higher staying durations are required. Also, due to the limited knowledge in practical control measures on indoor transmissions of SARS-CoV-2, a mechanistic approach is needed to deeply evaluate influences of ventilations, exposure time, or indoor populations for better prevention of potential disease transmissions in certain aerosol microenvironments.
To address this approach, we adopted the Wells-Riley model as the mechanistic approach due to its linking with various adjustable indoor conditions and potentiality in design and indoor transmission assessments of healthcare buildings. The inhaled-exhaled air dynamics-based Wells-Riley model has successfully treated airborne transmission of infectious diseases (Guo et al. 2021; Rudnick and Milton 2003). To more straightforwardly explore the associations of various conditions of indoor setting with the basic reproduction number (R0) (the average number of secondary infections produced by an infected individual in a susceptible host population), a modified Wells–Riley equation with appropriate mathematical manipulations were applied in indoor transmission modeling (Chen et al. 2006). To take the intrinsic limitation of the model into account, we considered the most conservative scenario with one infector and lower ranges of physiological parameters in parameterizations as baseline evaluations for R0 estimations. Although there are several limitations in the Wells-Riley model, the approach along with modified ones generally make valid arguments for airborne infectious disease transmission and agree in their predictions of concentration profiles and infection risk (Cheng and Liao 2013; Foster and Kinzel 2021; Qian et al. 2009). Furtherly, we also performed a case study investigating probabilistic-based R0s with different scenarios of inhalation rates in the two Wuhan (Fangcang/Renmin) hospitals by adopting the field data of Liu et al. (2020). Apart from field estimations, functional spaces in healthcare facilities with different role delineation of levels (RDLs) were also performed for general estimations. The RDLs refer to a level of service describing the complexity of clinical activities undertaken by that service. The level is determined by the presence of medical, nursing and other healthcare personnel holding compatible with the defined level of service (TAHPI 2015). The emergency unit with typical volumes for functional rooms from RDL1 to RDL6 defined in TAHPI (2015) was exemplified as a general illustration for healthcare buildings to explore the impacts of air supply rates, indoor population numbers, or exposure time on controlled reproduction number (RC) (the average number of new individuals infected by an infector with SARS-CoV-2 given the current control measures) to provide theoretically sound prevention strategies on airborne transmissions. Finally, sensitivity analyses were performed to elucidate the most remarkable parameters contributing to space-specific airborne SARS-CoV-2 transmissions.
Materials and methods
Study data
Field data of interior designs of two Wuhan (Fangcang/Renmin) hospitals were adapted from published literature (Liu et al. 2020). Specifically, the floor plan of Fangcang shelter hospital including three zones (A, B, and C) and a mobile toilet (portable toilet that can be moved around) near the rear gate are schematized based on Liu et al. (2021) (Fig. 2). The shelter hospital was built in a large space located in the Wuhan Cultural Centre with adequate ventilations and 1400 beds in the three Zone areas, in which the Protective Apparel Removal Room (PARR) refers to a functional room to remove personal protective equipment by medical staff (Liu et al. 2021).
For general considerations of indoor settings in healthcare facilities for the following simulations of indoor transmissions, averaged room volumes in hospitals with different service levels from RDL1 to RDL6 were obtained from TAHPI (2015) (Supplementary Table S1). Among all functional units, only the emergency unit was exemplified for simulations of indoor transmissions in different indoor scenarios (e.g., exposure time, indoor population number, or air supply rate).
Indoor transmission model and study design
The Wells-Riley model was used to describe airborne transmission and assess potential infection risks in enclosed environments. The infection risk can be evaluated with the Wells-Riley mathematical equation as follows,
where D is the number of infected ones, S is the number susceptible subjects, i is the number of infectors, q is the quantum generation rate by an infectious individual (quanta h−1), p is the inhalation rate per person (m3 h−1), t is the total exposure time (staying duration) (h), Q is the fresh air supply rate to remove infectious aerosol particles in an enclosed space (m3 h−1), and V is the room volume (m3).
With appropriate mathematical manipulations from Eq. (1) based on previous studies (Chen et al. 2006; Rudnick and Milton 2003), indoor R0 for an airborne infection could be estimated by the Wells-Riley model based on characteristics of building settings along with population physiology,
where n is the number of total populations indoors, n − 1 stands for the assumption that there are 1 infector, and thus, n − 1 susceptible individuals at an initial respiratory infection condition.
Since the modified Wells–Riley model assumes that there would be one infector indoors, we considered a relatively safe indoor exposure scenario as the most conservative evaluation for R0 with one infector, normal quanta generation rate (< 100 quanta h−1), and resting as the activity level with the basic requirements for room volumes and ventilations in healthcare buildings based on previous literature (ASHRAE 2020; TAHPI 2015). The consideration for using the most conservative scenario could give a general realization for the baseline of R0 if only one infector is considered in the indoor environments, and higher R0 would be expected if more infectors, higher quanta generation numbers, or inhalation rates are applied with the same indoor conditions.
Mode parameterizations and implementations
Specifically, the Vs were derived by adopting the basic requirements for room spaces from RDL1 to RDL6 in healthcare facilities (TAHPI 2015) (Supplementary Table S1). Qs was probabilistically derived based on the basic requirements of air change per hour (ACH) in health care facilities (ASHRAE 2020) (Supplementary Tables S2-S4), where the ACHs were estimated in three space categories of inpatient, outpatient, and residential health or care, and support-specific (Supplementary Fig. S1a-c; Supplementary Table S5). Basic requirements of ACH corresponding to each functional areas in the two Wuhan (Fangcang/Renmin) hospitals were compiled (Supplementary Table S6). For the exemplified emergency unit in healthcare facilities, derived requirements for room volumes corresponding to basic ACH rates were also listed (Supplementary Table S7).
The q was probabilistically estimated based on results derived from a reproductive number-based fitting approach (Dai and Zhao 2020), by assuming that occurrence of high quanta emission rate (> 100 quanta h−1) is relatively unlikely in healthcare facilities (Buonanno et al. 2020) (Supplementary Fig. S1d). For inhalation rate, since there are high variabilities among the five different activity levels (0.49, 0.54, 1.38. 2.35, and 3.30 m3 h−1 for resting, standing, light exercise, moderate exercise, and heavy exercise, respectively) averaged between males and females (Adams 1993; Buonanno et al. 2020), the probability distribution of p was derived by considering all activity levels (Supplementary Fig. S1e).
The R0 estimates were evaluated in the three inpatient areas (Zones A, B, and C workstations) of two Wuhan (Fangcang/Renmin) hospitals with basic requirements of ACHs and assumed indoor populations and exposure time referred from Liu et al. (2021) (Supplementary Tables S6). There were two scenarios implemented for R0 estimations in the three inpatient areas of two Wuhan hospitals by considering: (i) variabilities in inhalation rates with inclusions of the five different activity levels (Supplementary Figs. S1e) and (ii) the inhalation rate in resting scenario as a baseline evaluation for R0 estimates. For the R0 simulations in different functional spaces of the two Wuhan hospitals and the exemplified emergency unit, space-specific R0s were dynamically estimated with different exposure time and indoor population numbers based on the basic requirements of room volumes and ACHs (Supplementary Table S6). Interactions of R0 − exposure time (t) − population number (n) were constructed by using the inhalation rate in resting scenario as a baseline evaluation to provide the most conservative estimations of R0 in planning COVID-19 control measures when applying the scenario of one infector and the lowest inhalation rate in indoor spaces in control models.
COVID-19 control models
Here, we proposed three RC-control models that only require data on basic requirements of ACHs and room volumes and any designated indoor population numbers or exposure time. The emergency unit in general health care buildings from RDL1–RDL6 was used to explore associations of RC changes with different control measures by using the basic design requirements for room volumes and ACHs in the 8 categorized functional areas (entry/reception/waiting, triage, resuscitation/treatment area, fast track-primary care/consulting, support areas, paediatric assessment/short stay, mental health/behavioural assessment, and staff areas) (Supplementary Table S7).
The first controlled model was intuitively based on the Wells-Riley model as follows,
where nc is the increments of controlled number of persons, and tc is the controlled total exposure time. The constructed control lines of nc − tc lay out a practical metric for examining qualitatively and quantitatively the efficacy of containment on the spread of COVID-19 based on area under the contour lines of RC estimates: RC < 1, the outbreak will be contained eventually; RC > 1, however, additional interventions should be intervened.
In the second model, we aimed to offer a strategy to adjust both ACH and indoor population number simultaneously for COVID-19 containment. The RCs were evaluated by adjusting various controlled ACHs (ACHC) and tc with a threshold indoor population number (nc,t) that was estimated when R0 = 1 and tc = 1 h with basic requirements of ACHs and room volumes as the following equation (ASHRAE 2020; TAHPI 2015),
Moreover, to adapt to the scenario that several buildings have limited resources to adjust air supply systems, we established the third model to estimate RC in the condition that controlled exposure time (tc) is higher than 1 h and controlled indoor populations (nc) are higher than the second control model-derived nc,t estimates with the basic requirements of ACHs (Supplementary Tables S6-S7) as follow,
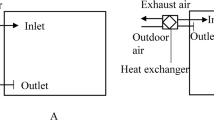
Therefore, to investigate airborne transmissions of SARS-CoV-2 and propose practical strategies for COVID-19 containments in two Wuhan hospitals and general healthcare facilities, the study framework was designed as (i) data collections of interior settings of two Wuhan hospitals with basic requirements for ACH and room volumes in healthcare facilities (Fig. 1a); (ii) applications of the Wells-Riley model based on conservative parameterizations of quantum generation number, inhalation rate, room volume, air supply rate, and indoor population number (Fig. 1b); (iii) model implementations of dynamic R0 estimates with various exposure time and peoples and explorations of the most sensitive parameters by performing sensitivity analyses (Fig. 1c); and (iv) provisions of strategies for COVID-19 containments based on three RC-control models constructed by the relationships among population number, exposure time, and ACH (Fig. 1d).
Uncertainty and sensitivity analyses
Uncertainty analyses performed for estimating key human physiological/engineering parameters including room volumes, ACH, quantum generation number, and inhalation rate in the Wells-Riley model were implemented with 100,000 Monte Carlo (MC) simulations to obtain geometric means (gms), and geometric standard deviations (gsds) in lognormal (LN) functions (LN(gm, gsd)) with the Crystal Ball software (Version 11.1.2.4, Oracle Corporation, Redwood Shores, CA, USA). Data visualizations such as 3-dimensional scatter, contour, and bubble plots were generated by using the language R (Version 4.1.3, The R Foundation for Statistical Computing). Sensitivity analyses were performed by adjusting each parameter with 0.1 × or 10 × ranges to evaluate the overall contributions of each physiological or engineering parameter to R0 in each functional room of the two Wuhan hospitals or the emergency unit in healthcare facilities as: (R0 (Rc) estimated from 0.1 × or 10 × -adjusted parameter − R0 (Rc) estimated from 1 × parameter)/0.1 × or 10 × -adjusted parameter.
Results
Parameterizations in the Wells-Riley model
Essential physiological or engineering parameters applied in the indoor transmission model were probabilistically pre-estimated and derived before R0 estimations. Specifically, distributions of ACH were estimated with LN functions as LN (7.05, 3.04), LN (7.90, 4.40), and LN (7.27, 3.75) in for inpatient, outpatient, and residential health or care, and support-specific spaces, respectively (Supplementary Figs.S1a-c). The distribution of q (14 − 48 quanta h−1) adopted from Dai and Zhao (2020) was estimated as LN (25.90, 1.45) (Supplementary Fig. S1d). The inhalation rate was probabilistically estimated as LN (1.29, 1.95) by applying high uncertainties in the five activity levels (Supplementary Fig. S1e).
R0 in patient areas of Fangcang hospital
We estimated R0 in Zones A, B, and C of Fangcang hospital with two scenarios by taking variabilities of inhalation rate (Supplementary Fig. S1e) and the inhalation rate in resting level based on conditions of 100 or 200 persons and exposure time of 20 h indoors (Supplementary Table S7). The estimated ranges of ACH of patient care areas and clinical support spaces (LN(7.05 h−1, 3.04) – LN(7.90 h−1, 4.40)) were applied in R0 estimations (Supplementary Fig. S1a, b, c). Results showed that the R0 estimates are consistently higher when applying the inhalation rate with variabilities (Fig. 1a, c, e, g, i, k). Among the three zones, Zone B with the smallest volume (V = 2000 m3) exhibited the highest R0s of LN (5.21, 2.74) and LN (1.85, 2.67) when 100 people indoors with higher (considering activity variabilities) and lower (resting scenario) inhalation rates, respectively (Fig. 2c, d). Also, the R0 estimations in Zone A and C (V = 5000 m3) have closed results in the same conditions of inhalation rate or indoor population numbers (Fig. 2a, b, e, f, g, h, k, l).
Basic reproduction numbers (R0s) estimates as the lognormal (LN) distribution (LN(gm, gsd)) in Zones A, B, and C of patient areas of the Fangcang hospital under conditions of total exposure time of 20 h and indoor population of 100 when a, c, e taking variabilities in inhalation rate for consideration and b, d, f using the inhalation rate in resting level or indoor population of 200 when g, i, k taking variabilities in inhalation rate for consideration and h, j, l using the inhalation rate in resting level
R0 estimations with dynamic exposure time and indoor population number
Our results showed that among the three patient areas, Zone B still exhibited the highest R0s when compared to those of Zones A and C in the same indoor conditions, in that R0s exceed 1 when there are 400 people staying over 3 h and 500 people over 6 h in Zones B and A/C, respectively (Fig. 3a, b, c). Additionally, the passageway for medical staff (Renmin hospital) had the highest R0s (Fig. 3k), followed by medical staff’s office (Fig. 3f),; intensive/coronary care unit and Ward Zone 16 (Fig. 3j); PARR of Zones A, B, and C (Fig. 3d); dining room for medical staff (Fig. 3l) or university office doorside (Fig. 3m); warehouse (Fig. 3h); Fangcang hospital pharmacy (Fig. 3i); university hospital outpatient hall (Fig. 3n); staff change room (Fig. 3e); and meeting room (Fig. 3g). Generally, the smaller the room volume, the higher the R0s (Supplementary Table S7).
R0 − exposure time (t) − indoor population numbers (n) interactions in a Zone A, b Zone B, and c Zone C workstations; d Protective Apparel Removal Room (PARR) of Zone A/B/C, e staff change room, f medical staff’s office, g meeting room, h warehouse, and i pharmacy of the Fangcang hospital. And j Intensive Care Unit (ICU), Coronary Care Unit (CCU), and Ward Zone 16, and k Passageway for Medical Staff, l Dining Room for Medical Staff, m University Office Doorside, and n University Hospital Outpatient Hall of the Renmin hospital
For sensitivity analyses, results indicated that inhalation rate (p) has the most significant effect on R0s in all room types, followed by air supply rate (Q), exposure time (t), q, numbers of population (n), and room volume (V) (Supplementary Fig. S2). Results also revealed that the smaller the V, the higher the effects of each physiological/engineering parameter on R0 (Supplementary Fig. S2).
RC simulations with dynamic exposure time and indoor population number in emergency unit
In the first RC-control model, we used representative functional rooms to explore associations of changes of ACHs and indoor population numbers with RC estimates in different functional rooms of the emergency unit (Supplementary Fig. S3). Overall, the top three areas with the highest standards of indoor population number (nc) based on the same condition of exposure time (tc = 2 h) at RC < 1 were bay-handwashing (support areas) (nc = 5) (Fig. 4D), triage-nurse (triage) (nc = 7) areas (Fig. 4e), and reception (entry/reception/waiting) (nc = 14) (Fig. 4a). In contrast, area with the loosest standard was patient bay-resuscitation area (resuscitation trauma) (nc = 80) (Fig. 4b).
Contour plots describing RCs with various controlled total exposure time (tc, h) and controlled population number (nc) under basic requirements of ventilation rate and room volume in functional room of a reception (entry/reception/waiting), b patient bay-resuscitation (resuscitation/treatment area), c procedure room (resuscitation/treatment area), d bay-handwashing (support areas), e triage-nurse (triage), f consult room (fast track-primary care/consulting), g staff room (staff areas), and h patient bay-non acute treatment (paediatric assessment/short stay) in the emergency unit. Red arrows indicate path of travel. Only representative functional rooms were selected to present the simulation results for the control measure as described in (Supplementary Table S7)
On the other hand, our simulated functional space-specific RC dynamics showed that rooms with the most rigorous standard on COVID-19 containment in entry/reception/waiting, triage, resuscitation/treatment area, fast track-primary care/consulting, support areas, paediatric assessment/short stay, and staff areas were bay-wheelchair park, nurse triage, shower-patient, bay-handwashing, bay-pathology, store-equipment/general, and toilet-staff, respectively (Supplementary Fig. S3).
Fixed nc,t-based control measure in emergency unit
The functional room-specific nc,ts were derived with the condition of RCs = 1 and tc = 1 h with basic requirement of room volumes. Our results showed that bay-handwashing (support area) had the lowest nc,t given a minimum requirement of room volume (Vm) (nc,t = 10, Vm = 12 m3) (Fig. 5d), followed by triage-nurse (triage) (nc,t = 15, Vm = 20 m3) (Fig. 5e), reception area (entry/reception/waiting) (nc,t = 30, Vm = 44 m3) (Fig. 5a), staff room (offices meeting rooms/staff support) (nc,t = 40, Vm = 54 m3) (Fig. 5f), procedure room (procedures) (nc,t = 55, Vm = 81 m3) (Fig. 5c), consult room (adult fast track) (nc,t = 80, Vm = 113 m3) (Fig. 5g), patient bay-non acute treatment (paediatric assessment or acute/non-acute observation) (nc,t = 90, Vm = 135 m3) (Fig. 5h), and patient bay-resuscitation area (resuscitation trauma) (nc,t = 120, Vm = 180 m3) (Fig. 5b).
Bubble plots showing control measures on controlled ACH (ACHc) with various controlled total exposure time (tc) based on estimated threshold indoor population number (nc,t) in a reception (entry/reception/waiting), b patient bay-resuscitation (resuscitation/treatment area), c procedure room (resuscitation/treatment area), d bay-handwashing (support areas), e triage-nurse (triage), f consult room (fast track-primary care/consulting), g staff room (staff areas), and h patient bay-non acute treatment (paediatric assessment/short stay) of the emergency unit. Red arrows indicate path of travel. Only representative functional rooms were selected to present the simulation results for the control measure as described in (Supplementary Table S7)
In the second RC-control approach, not surprisingly, we found an overall trend that the higher the ACH, the lower the RC estimate. Results also indicated that COVID-19 could be reduced by adjusting ACH, to higher than 7 h−1 of all functional rooms in the emergency unit with nc,t ≤ 10 and tc = 1 h (Fig. 5). However, when tc increased to an extreme level of 8 h (in this study), ACH should also be increased to a much higher value as follows: bay-handwashing (support area, 40 h−1), triage- nurse (triage, 68 h−1), reception area (entry/reception/waiting, 66 h−1), staff room (offices meeting rooms/staff support, 62 h−1), procedure room (procedures, 48 h−1), consult room (adult fast track, 66 h−1), patient bay-non acute treatment (paediatric assessment or acute/non-acute observation, 54 h−1), and patient bay-resuscitation area (resuscitation trauma, 67 h−1) (Fig. 5).
Fixed air supply rate-based control measure in emergency unit
In the third RC-control model (Fig. 6), RCs were estimated in the condition of tc > 1 h and nc > nc,t with basic air supply rate (Qc) in each functional room. Results showed that in the most extreme scenario of exposure time in this study (tc = 8 h), RCs could be as high as 33 in bay-handwashing (support area) (Fig. 6d), followed by 18 in triage-nurse (triage) (Fig. 6e), 13 in reception area (reception/administration) (Fig. 6a), 11 in staff room (offices meeting rooms/staff support) (Fig. 6f), 8 in procedure room (procedures) (Fig. 6c), 6 in consult room (adult fast track) (Fig. 6g), and 4 in both patient bay-non acute treatment (paediatric assessment or acute/non-acute observation) (Fig. 6h) and patient bay-resuscitation area (resuscitation trauma) (Fig. 6b) when nc = 50.
Bubble plots showing control measures on controlled population number (nc) with various controlled total exposure time (tc) based on basic requirements of ventilation rate and room volume in a reception (entry/reception/waiting), b patient bay-resuscitation (resuscitation/treatment area), c procedure room (resuscitation/treatment area), d bay-handwashing (support areas), e triage-nurse (triage), f consult room (fast track-primary care/consulting), g staff room (staff areas), and h patient bay-non acute treatment (paediatric assessment/short stay) of the emergency unit. Red arrows indicate path of travel. Only representative functional rooms were selected to present the simulation results for the control measure as described in (Supplementary Table S7)
Similar to the results from two Wuhan hospitals, sensitivities of each physiological/engineering parameter on RCs in the emergency unit depend significantly on room volumes (Supplementary Fig. S4). Among all parameters, inhalation rate p also has the most significant effects on room type-specific RC, followed by tc, Vc, Qc, nc, and q (Supplementary Fig. S4).
Discussion
Role of indoor transmission in COVID-19 pandemics
There has been a growing body of evidence that airborne transmission is associated with the spread of COVID-19, especially in poorly ventilated built environments (Buonanno et al. 2020; CDC 2021; Morawska 2006; Morawska and Cao 2020; Oswin et al. 2022). Aerosols (< 100 μm) generated from human expiratory activities such as breathing, speaking, singing, sneezing, or coughing can linger in the air for hours and travel 1–2 m away from the infected person who exhaled them, causing new infections over short and long distances (Wang et al. 2021). Ventilation airflows, people traffic, and convective flows can influence the movements of aerosols before being inhaled (Tang et al. 2021). Although SARS-CoV-2 virion is a nanoparticle, it is usually carried by larger particles (especially PM2.5), and can be mostly contained by masks (N95, filtering facepiece respirator, or surgical mask) (Romano-Bertrand et al. 2021). Therefore, “droplets” precaution also remains as an efficient means of protecting healthcare workers caring for COVID-19 patients (Romano-Bertrand et al. 2021).
Not limited to COVID-19 pandemics, numerous studies have evidenced that buildings are closely associated with spreading of infectious diseases. Higher risks of aerosol transmission are more likely to take place in clinic settings of older/repurposed buildings with older heating, ventilation and air conditioning (HVAC) systems (Kohanski et al. 2020). Moreover, viral infectious diseases could be transmitted across distances by aerosols, leading to large clusters of infection in short periods (Fineberg 2020; WHO 2009; Xiao et al. 2017). Therefore, resolutions for mitigating airborne transmission of SARS-CoV-2 have become imminent since exhaled viruses could accumulate with increments of staying time or number of persons, making confined spaces much more dangerous than in outdoors (Lewis 2021). In addition, aerosol transmission produced by asymptomatic individuals is also one of the major causes of SARS-CoV-2 transmission, especially in spaces with poor ventilations, longer staying duration, or large gatherings (Anderson et al. 2020).
Control measures for indoor transmission of SARS-CoV-2
Generally, the suggested precautions against indoor aerosol transmission include using natural ventilation, increasing ventilation rates, avoiding air recirculation, staying in front of the airflow, or minimizing number of people indoors (Qian and Zheng 2018). For ventilation rates, it was recommended that minimum air change per hour (ACH) standards should be 0.35 h−1 in most households, 2 − 3 h−1 in offices, 5–6 h−1 in school classrooms, 7–17 h−1 in airplane cabins, and 4–20 h−1 in different functional rooms of hospitals (ASHRAE 2020). However, large uncertainties were found in reducing indoor infection risks by only adjusting ventilation rates (Katal et al. 2021). Therefore, multiple interventions are suggested to be practiced together in measures such as adjusting room settings, numbers of total population or infected people indoors, and activity levels. Moreover, mobile air purifiers or filters in HVAC systems could be an efficient tool to save extra energy in heating/cooling systems by cleaning recirculated air accompanied with the strategy of controlling ventilation rates. It was found that the most efficient filter, known as minimum efficiency reporting value (MERV) 16, could remove > 95% particles with diameters ranging from 0.3 to 10 μm (Leung et al. 2020; Sublett et al. 2010). In addition, the portable air cleaners such as stand-alone high-efficiency particulate air (HEPA) filters that could supply effective flow rates of particle-free air can be another efficient strategy for old buildings with limited ventilation efficiencies (Shaughnessy and Sextro 2006; Waring et al. 2008).
Previous studies suggested that combinations of (i) increasing outdoor ventilation, (ii) application of high-efficiency filtration (MERV 13), and (iii) portable HEPA filters could increase ACHs from 0.32–3 h−1 to 4–6 h−1 in small-volume enclosed spaces (Allen and Marr 2020; Allen and Ibrahi 2021). Ventilators at the upper level of walls would also be more effective in air movements and ventilations (Farooq et al. 2020). Moreover, dominant flow pattern also plays a crucial role in removing contagions and cross-contamination between persons. Compared with mixing ventilation that occupants are likely to be surrounded by mixed air with uniform properties, displacement ventilations were recommended to minimize further spread of COVID-19. Displacement ventilations are capable of making occupants surrounded by newly arrived air and lifting contagions generated by infected individuals-induced towards ceiling with rising warm air (Bhagat and Linden 2020).
Preventive strategies for disease outbreaks in hospitals
There has been increasing evidence showing high potentials for viral transmissions either through air- or surface-borne SARS-CoV-2 contact in healthcare facilities (Richterman et al. 2020). It was reported that 44% of 179 cases of COVID-19 infections were acquired from hospitals (Zhou et al. 2020). The WHO also suggested that health care workers account for up to 1 in 7 cases of COVID-19 worldwide. Based on a prospective cohort study conducted in general communities of the UK and USA, higher risk for reporting positive COVID-19 test (adjusted hazard ratio of 3.40) in front-line health-care workers was found, implicating a dire situation of higher infectability of health workers even with universal masking protocols (Nguyen et al. 2020).
Primary suggestions for prevention of hospital-acquired infections were provided previously (Ducel et al. 2002). Location of outdoor air inlets is suggested to be as high and remote away from ventilation discharge outlets, incinerators, or boiler stacks as possible. In this way, clean air can move downward toward the contaminated floor to keep enclosed spaces clean with low exhausts. Also, high-efficiency filters should be essentially provided in ventilation systems of serving areas to prevent patients from potential infections or in functional rooms with clinical procedures to avoid unusual hazards such during surgical procedures. In addition, at least a velocity of 0.25 m s−1 airflow through a HEPA filter circulated into the room was suggested to reach ultra-clean air. Produced ultra-clean air could be furtherly applied in areas such as microbiology laboratories, pharmacies, special intensive care units, and operating rooms. Moreover, negative air pressure could be applied in contaminated areas or rooms for isolation of patients infected by airborne-transmitted diseases to restrict the movements of contaminated air from leaking out of the rooms (Ducel et al. 2002).
Generally, the Centers for Disease Control and Prevention (CDC) suggested that hospital-based clinic rooms require minimum ventilations of 6 ACH, operating rooms of 15 ACH, and outpatient facilities of ~ 2 ACH (CDC 2019). However, although many hospital facilities have provided adequate ventilations in a routine measure, it is highly likely that spaces where more patients are admitted or densely clustered do not have sufficient ventilation rates for infection preventions (Morawska and Milton 2020). Negative pressure ventilation alone in several functional rooms of hospitals is also not thought to be sufficient to provide protection to patients or staff (Ribaric et al. 2022).
Minimal surface-borne and non-airborne SARS-CoV-2 RNA in hospital areas utilizing HEPA filters were observed regardless room type, ventilation system, and number of ACH, indicating the importance of utilizing HEPA filters in ventilation systems (Ribaric et al. 2022). Furthermore, very low viral concentrations with significant reductions of air- and surface-borne SARS-CoV-2 were observed when ACH was above 16 h−1 (Ribaric et al. 2022). Reassessing this empirical result by using our constructed model, however, revealed no inconsistency. Namely, we confirmed that COVID-19 containment could be achieved with an ACH of 16 h−1 under certain conditions of the most stringent (bay-handwashing: tc ≤ 3 h with nc = 10) or loosest indoor setting scenario (patient bay-resuscitation: tc ≤ 1 h with nc = 120) based on basic requirements of room volumes and ventilation rates of the emergency unit in healthcare facilities.
On the other hand, it was evidenced that viable SARS-CoV-2 was isolated from air samples collected 2–4.8 m away from patients staying in a hospital room (Lednicky et al. 2020), indicating that there may be an airborne transmission with super-spreading phenomena even in a 6 ACH ward. A multivariate analysis also provided a crucial information that the odds to detect SARS-CoV-2 in rooms with negative pressure but without laminar airflow or HEPA filtration were not significantly lower than those without any mechanical ventilation, suggesting a pivotal role of effective filtration systems in ventilation facilities (Beaussier et al. 2022). Also, from a different perspective, application of additional cold air on sunny side of hospital rooms during seasonal changes is also suggested, since solar radiations-induced temperature differences were associated with contaminated air transportation from rooms to other public areas (Beaussier et al. 2022). Taken together, in addition to the existing ventilation system, adding effective HEPA filters or seasonal control of indoor airflow could be effective tools to enhance the effectiveness of ventilation systems in enclosed areas of healthcare facilities.
Limitations and implications
In this study, we adopted the Wells-Riley model to parsimoniously estimate R0 values with the most conservative exposure scenario as a baseline evaluation for R0 estimations in various functional units in two Wuhan hospitals or basic Rc considerations for the exemplified emergency unit. In our approach, we aimed to derive baseline evaluations of R0 and Rc with basic requirements of indoor settings and baseline values of physiological parameters in the condition of no intervention of control measures (e.g., masking, social-distancing) applied (Gupta et al. 2012). The reasons for choosing this scenario are to derive the baseline values of R0 with the simplest exposure scenario and to exclude the uncertainties of policy implementations such as universal masking indoors in different countries or areas. If the same indoor conditions (e.g., activity level, quantum generation number, indoor population, room volume, and ventilation) are applied, lower R0 values are expected with implementation of control measures (e.g., wearing mask), whereas higher R0 could occur if higher physiological parameters or indoor population are applied.
On the other hand, we found that parameter impacts/sensitivities on R0 are influenced by other parameter values (e.g., sensitivity of air supply rate on R0 is affected by room volume), indicating that parameter sensitivities substantially depend on exposure scenarios and indoor settings. However, the Wells-Riley model with certain assumptions and limitations (e.g., well-mixed air and uniform concentrations of aerosols) may has limitations since heterogeneous distributions of airborne SARS-CoV-2 could result in different exposure probabilities on subjects indoors.
Based on the conservative parameterizations applied in this study, higher R0 estimations are expected with the same indoor conditions when (i) more than 1 infector were in the same room or (ii) higher inhalation rates or quantum generation numbers were applied to different subjects. Notably, Buonanno et al. (2020) suggested that high quanta emission rates (> 100 quanta h−1) could be reached by an asymptomatic infectious SARS-CoV-2 subject performing vocalization during light activities, yet low quanta emission rate (< 1 quantum h−1) occurred in resting conditions. Since it would be more unlikely that vocalization performed by subjects occurs in hospitals and there is high variability in quanta emission numbers, we thus estimated this parameter ranging from 14 to 48 quanta h−1 in a relatively conservative perspective based on a previous study (Dai and Zhao 2020).
Not limited to hospitals, mitigation strategies for allowing clinics to remain operational when regional surges in cases occur are also important. Staff without patient contacts are also likely to be infected if they spend prolonged times in corridors and nurses’ stations (Azuma et al. 2020; Buising et al. 2022). Although the ability of virus transmitted from patient room into other spaces was not considered in our study, we found that exposure time is one of the most sensitive parameters for functional rooms of emergency unit. Thus, to reduce acquisition risk of respiratory viruses, portable air cleaners were suggested for medical staffs to clean the air locally and provide protections equivalent to be as much as 30 ACH (Buising et al. 2022). However, in the circumstances of building using central ventilation systems, it was found that higher air exchange rates lead to increasing concentrations of respiratory droplets at short times, longer times are on the opposite (Vlachokostas et al. 2022). Noakes and Sleigh (2009) also had consistent findings derived from the Wells-Riley equation that the number and rate of new infections between connected spaces is strongly dependent on the airflow, indicating that buildings using centralized HVAC systems may have higher probabilities in indoor transmission than buildings without using the system.
In light of the importance of protecting healthcare staff, patients, and visitors against COVID-19, our study has implications for implementation of administrative interventions including triaging procedures, limiting number of people in hospital, and cohorting patients and staffs to reduce nosocomial spread of COVID-19 (Ahmad and Osei 2021). The R0-based air supply rates could provide useful information in combination with engineering controls in parallel with effective applications of other strategies (Morawska et al. 2020).
Taken together, our analyses represent a comprehensive estimate of the minimum ACH that requires attention for COVID-19 containment to safeguard intervention policies. Moreover, changing room volumes is not much impactful on R0 than other parameters, and is also not a practical strategy for most healthcare facilities. Among these R0- or RC-associated parameters, we found inhalation rate to be highly influential in reducing the relative spread potential of COVID-19. Much higher impacts of inhalation rate were also found in smaller rooms than spacious ones, indicating the importance of controlling activity levels in healthcare facilities. We thus provide the following suggestions for preventive measures on SARS-CoV-2 transmission: (i) to prevent higher inhalation rates resulting from running, exercising, or any forms of labouring, (ii) to enhance ventilation rate to be higher than 7 h−1 if there are more than 10 people staying indoors over 1 h (yet, higher ACHs are required if more than 1 infector or higher activity level applies), and (iii) using HEPA filters to ensure appropriate dilutions of airborne SARS-CoV-2 especially in buildings with centralized HVAC system to prevent nosocomial COVID-19 infections when there is a surge of cases.
Conclusions
We offer a practical approach by using a modified Wells-Riley model to reflect the most conservative R0s in the two Wuhan hospitals and the emergency unit in healthcare buildings as a general illustration. We highlight that inhalation rates of individuals prove crucial for influencing the transmissibility of SARS-CoV-2, followed by exposure time, room volume, and air supply rate. We suggest that control measures mainly focus on the awareness of appropriately controlling activity levels, optimizing exposure time/number of people indoors, and enhancing air purifiers in an enclosed space. With the difficulties in altering room volumes of hospitals or any healthcare buildings during case surging periods, the most practical and flexible mitigation strategies would be adjustments of air supply rates or adding the HEPA systems. Critically, we also provided simulations to evaluate the success of policy actions and interventions intended to improve public safety efforts on preventing spread of COVID-19 in built environments. Our approach reconsidered from the Wells-Riley model as presented here may help provide an efficient means of impact assessment for SARS-CoV-2 transmission and assist in future interventions planning, early COVID-19 infection detection, and mitigation efforts.
Data availability
The results of this study are reproducible and extensible by use of the cited data sources and other information in the supplementary materials.
References
Adams WC (1993) Measurement of breathing rate and volume in routinely performed daily activities. Final Report. Human Performance Laboratory, Physical Education Department, University of California, Davis. Human Performance Laboratory, Physical Education Department, University of California, Davis. Prepared for the California Air Resources Board, Contract No. A033–205
Ahmad IA, Osei E (2021) Occupational health and safety measures in healthcare settings during COVID-19: strategies for protecting staff, patients and visitors. Disaster Med Public Health Prep 14:1–9
AIA (American Institute of Architects), Guidelines for design and construction of hospital and health care facilities, Washington, DC: American Institute of Architects Press, 2001
Allen JG, Marr LC (2020) Recognizing and controlling airborne transmission of SARS-CoV-2 in indoor environments. Indoor Air 30:557–558
Allen JG, Ibrahim AM (2021) Indoor air changes and potential implications for SARS-CoV-2 transmission. JAMA -J Am Med Assoc 325(20):2112–2113
Anderson EL, Turnham P, Griggin JR, Clarke CC (2020) Consideration of the aerosol 23 transmission for COVID-19 and public health. Risk Anal 40(5):902–907
ASHRAE (the American Society of Heating, Refrigerating and Air-Conditioning Engineers) (2020) Addendum a for ANSI/ASHRAE/ASHE Standard 170–2017, Ventilation of Health Care Facilities. American Society of Heating, Refrigerating and Air-Conditioning Engineers, Inc, Atlanta. Available at: https://www.ashrae.org/technical-resources/standards-and-guidelines/standards-addenda/ansi-ashrae-ashe-standard-170-2017-ventilation-of-health-care-facilities. Accessed 18 Nov 2021
Azuma K, Yanagi U, Kagi N, Kim H, Ogata M, Hayashi M (2020) Environmental factors involved in SARS-CoV-2 transmission: effect and role of indoor environmental quality in the strategy for COVID-19 infection control. Environ Health Prev Med 25(1):66
Bazant MZ, Bush JWM (2021) A guideline to limit indoor airborne transmission of COVID-19. Proc Natl Acad Sci USA 118(17):e2018995118
Beaussier M, Vanoli E, Zadegan F, Peray H, Bezian E, Jilesen J, Gandveau G, Gayraud JM (2022) Aerodynamic analysis of hospital ventilation according to seasonal variations. A simulation approach to prevent airborne viral transmission pathway during Covid-19 pandemic. Environ Int 158:106872
Bhagat RK, Linden PF (2020) Displacement ventilation: a viable ventilation strategy for makeshift hospitals and public buildings to contain COVID-19 and other airborne diseases. R Soc Open Sci 7(9):200680
Buising KL, Schofield R, Irving L, Keywood M, Stevens A, Keogh N, Skidmore G, Wadlow I, Kevin K, Rismanchi B, Wheeler AJ, Humphries RS, Kainer M, Monty J, McGain F, Marshall C (2022) Use of portable air cleaners to reduce aerosol transmission on a hospital coronavirus disease 2019 (COVID-19) ward. Infect Control Hosp Epidemiol 43(8):987–992
Buonanno G, Stabile L, Morawska L (2020) Estimation of airborne viral emission: Quanta emission rate of SARS-CoV-2 for infection risk assessment. Environ Int 141:105794
CDC (Centers for Disease Control and Prevention) (2019) Division of healthcare quality promotion. Environmental Infection Control Guidelines: Appendix B (2019) Available at: https://www.cdc.gov/infectioncontrol/guidelines/environmental/appendix/air.html. Accessed 18 Nov 2021
CDC (Centers for Disease Control and Prevention) (2021) Prevention strategies for seasonal influenza in healthcare settings, guidelines and recommendations. Available at: https://www.cdc.gov/flu/professionals/infectioncontrol/healthcaresettings.htm . Accessed 18 Nov 2021
Chen SC, Chang CF, Liao CM (2006) Predictive models of control strategies involved in containing indoor airborne infection. Indoor Air 16(6):469–481
Cheng YH, Liao CM (2013) Modeling control measure effects to reduce indoor transmission of pandemic H1N1 2009 virus. Build Environ 63:11–19
Dai H, Zhao B (2020) Association of the infection probability of COVID-19 with ventilation rates in confined spaces. Build Simul 13(6):1321–1327
Ducel JF, Nicolle L, Nicolle L (2002) Prevention of hospital-acquired infections: a practical guide, 2nd edn. WHO, Geneva
Farooq S, Zubair F, Kamal MA (2020) Evaluation of ventilation system efficiency with reference to ceiling height in warm-humid climate of Pakistan. Civ Eng Archit 8(5):824–831
Fineberg HV (2020) Rapid expert consultation on the possibility of bioaerosol spread of SARSCoV-2 for the COVID-19 pandemic (April 1, 2020). In: The National Academies Press N.R.C., ed. Washington, DC: The National Academies Press, National Research Council 2020
Foster A, Kinzel M (2021) Estimating COVID-19 exposure in a classroom setting: a comparison between mathematical and numerical models. Phys Fluids 33(2):021904
Guo Y, Qian H, Sun Z, Cao J, Liu F, Luo X, Ling R, Weschler LB, Mo J, Zhang Y (2021) Assessing and controlling infection risk with Wells-Riley model and spatial flow impact factor (SFIF). Sustain Cities Soc 67:102719
Gupta JK, Lin CH, Chen Q (2012) Risk assessment of airborne infectious diseases in aircraft cabins. Indoor Air 22(5):388–395
Huang PY, Wu TS, Cheng CW, Chen CJ, Huang CG, Tsao KC, Lin CS, Chung TY, Lai CC, Yang CT, Chen YC, Chiu CH (2022) Infection Control Working Group. A hospital cluster of COVID-19 associated with a SARS-CoV-2 superspreading event. J Microbiol Immunol Infect 55(3):436–444
Illingworth CJ, Hamilton WL, Warne B, Routledge M, Popay A, Jackson C, Fieldman T, Meredith LW, Houldcroft CJ, Hosmillo M, Jahun AS, Caller LG, Caddy SL, Yakovleva A, Hall G, Khokhar FA, Feltwell T, Pinckert ML, Georgana I, Chaudhry Y, Curran MD, Parmar S, Sparkes D, Rivett L, Jones NK, Sridhar S, Forrest S, Dymond T, Grainger K, Workman C, Ferris M, Gkrania-Klotsas E, Brown NM, Weekes MP, Baker S, Peacock SJ, Goodfellow IG, Gouliouris T, de Angelis D, Török ME (2021) Superspreaders drive the largest outbreaks of hospital onset COVID-19 infections. Elife 10:e67308
Jayaweera M, Perera H, Gunawardana B, Manatunge J (2020) Transmission of COVID-19 virus by droplets and aerosols: a critical review on the unresolved dichotomy. Environ Res 188:109819
Katal A, Albettar M, Wang L (2021) City reduced probability of infection (CityRPI) for indoor airborne transmission of SARS-CoV-2 and urban building energy impacts. medRxiv (preprint)
Kohanski MA, Lo LJ, Waring MS (2020) Review of indoor aerosol generation, transport, and control in the context of COVID-19. Int Forum Allergy Rhinol 10(10):1173–1179
Lednicky JA, Lauzard M, Fan ZH, Jutla A, Tilly TB, Gangwar M, Usmani M, Shankar SN, Mohamed K, Eiguren-Fernandez A, Stephenson CJ, Alam MM, Elbadry MA, Loeb JC, Subramaniam K, Waltzek TB, Cherabuddi K, Morris JG Jr, Wu CY (2020) Viable SARS-CoV-2 in the air of a hospital room with COVID-19 patients. Int J Infect Dis 100:476–482
Leung NHL, Chu DKW, Shiu EYC, Chan KH, McDevitt JJ, Hau BJP, Yen HL, Li Y, Ip DKM, Peiris JSM, Seto WH, Leung GM, Milton DK, Cowling BJ (2020) Respiratory virus shedding in exhaled breath and efficacy of face masks. Nat Med 26(5):676–680
Lewis D (2021) Why indoor spaces are still prime COVID hotspots. Nature 592(7852):22–25
Liu P, Zhang H, Long X, Wang W, Zhan D, Meng X, Li D, Wang L, Chen R (2021) Management of COVID-19 patients in Fangcang shelter hospital: clinical practice and effectiveness analysis. Clin Respir J 15(3):280–286
Liu Y, Ning Z, Chen Y, Guo M, Liu Y, Gali NK, Sun L, Duan Y, Cai J, Westerdahl D, Liu X, Xu K, Ho KF, Kan H, Fu Q, Lan K (2020) Aerodynamic analysis of SARS-CoV-2 in two Wuhan hospitals. Nature 582(7813):557–560
Lu CW, Liu XF, Jia ZF (2020) 2019-nCOV transmission through the ocular surface must not be ignored. Lancet 395(10224):e39
Mittal R, Ni R, Seo J (2020) The flow physics of COVID-19. J Fluid Mech 894:F2
Morawska L (2006) Droplet fate in indoor environments, or can we prevent the spread of infection? Indoor Air 16(5):335–347
Morawska L, Cao JJ (2020) Airborne transmission of SARS-CoV-2: The world should face the reality. Environ Int 139:105730
Morawska L, Milton DK (2020) It is time to address airborne transmission of Coronavirus Disease 2019 (COVID-19). Clin Infect Dis 71(9):2311–2313
Morawska L, Tang JW, Bahnfleth W, Bluyssen PM, Boerstra A, Buonanno G, Cao J, Dancer S, Floto A, Franchimon F, Haworth C, Hogeling J, Isaxon C, Jimenez JL, Kurnitski J, Li Y, Loomans M, Marks G, Marr LC, Mazzarella L, Melikov AK, Miller S, Milton DK, Nazaroff W, Nielsen PV, Noakes C, Peccia J, Querol X, Sekhar C, Seppänen O, Tanabe SI, Tellier R, Tham KW, Wargocki P, Wierzbicka A, Yao M (2020) How can airborne transmission of COVID-19 indoors be minimised? Environ Int 142:105832
Nguyen LH, Drew DA, Graham MS, Joshi AD, Guo CG, Ma W, Mehta RS, Warner ET, Sikavi DR, Lo CH, Kwon S, Song M, Mucci LA, Stampfer MJ, Willett WC, Eliassen AH, Hart JE, Chavarro JE, Rich-Edwards JW, Davies R, Capdevila J, Lee KA, Lochlainn MN, Varsavsky T, Sudre CH, Cardoso MJ, Wolf J, Spector TD, Ourselin S, Steves CJ, Chan AT (2020) COronavirus Pandemic Epidemiology Consortium. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health 5(9):e475-e483
Noakes CJ, Sleigh PA (2009) Mathematical models for assessing the role of airflow on the risk of airborne infection in hospital wards. J R Soc Interface 6 Suppl 6(Suppl 6):S791-S800
Oswin HP, Haddrell AE, Otero-Fernandez M, Mann JFS, Cogan TA, Hilditch TG, Tian J, Hardy DA, Hill DJ, Finn A, Davidson AD, Reid JP (2022) The dynamics of SARS-CoV-2 infectivity with changes in aerosol microenvironment. Proc Natl Acad Sci USA 119(27):e2200109119
Qian H, Li Y, Nielsen PV, Huang X (2009) Spatial distribution of infection risk of SARS transmission in a hospital ward. Build Environ 44(8):1651–1658
Qian H, Zheng X (2018) Ventilation control for airborne transmission of human exhaled bio-aerosols in buildings. J Thorac Dis 10(Suppl 19):S2295–S2304
Qian H, Miao T, Liu L, Zheng X, Luo D, Li Y (2021) Indoor transmission of SARS-CoV-2. Indoor Air 31(3):639–645
Ribaric NL, Vincent C, Jonitz G, Hellinger A, Ribaric G (2022) Hidden hazards of SARS-CoV-2 transmission in hospitals: a systematic review. Indoor Air 32(1):e12968
Richterman A, Meyerowitz EA, Cevik M (2020) Hospital-acquired SARS-CoV-2 infection: lessons for public health. JAMA-J Am Med Assoc 324(21):2155–2156
Romano-Bertrand S, Carré Y, Aho Glélé LS, Lepelletier D (2021) Scientific Committee of the French Society for Hospital Hygiene. How to address SARS-CoV-2 airborne transmission to ensure effective protection of healthcare workers? A review of the literature. Infect Dis Now 51:410–417
Rudnick SN, Milton DK (2003) Risk of indoor airborne infection transmission estimated from carbon dioxide concentration. Indoor Air 13(3):237–245
Shaughnessy RJ, Sextro RG (2006) What is an effective portable air cleaning device? A review. J Occup Environ Hyg 3(4):169–181
Sublett JL, Seltzer J, Burkhead R, Williams PB, Wedner HJ, Phipatanakul W (2010) American Academy of Allergy, Asthma & Immunology Indoor Allergen Committee. Air filters and air cleaners: rostrum by the American Academy of Allergy, Asthma & Immunology Indoor Allergen Committee. J Allergy Clin Immunol 125(1):32–38
TAHPI (Tactical Athlete Health & Performance Institute) (2015) International health facility guidelines: Part B — health facility briefing and design, Version 5. https://healthfacilityguidelines.com/ViewPDF/ViewIndexPDF/iHFG_part_b_complete, and Part C – Access, Mobility, OH&S, Version 4. Available at: https://healthfacilityguidelines.com/ViewPDF/ViewIndexPDF/iHFG_part_c_complete . Accessed 18 Nov 2021
Tang JW, Bahnfleth WP, Bluyssen PM, Buonanno G, Jimenez JL, Kurnitski J, Li Y, Miller S, Sekhar C, Morawska L, Marr LC, Melikov AK, Nazaroff WW, Nielsen PV, Tellier R, Wargocki P, Dancer SJ (2021) Dismantling myths on the airborne transmission of severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2). J Hosp Infect 110:89–96
To KK, Tsang OT, Yip CC, Chan KH, Wu TC, Chan JM, Leung WS, Chik TS, Choi CY, Kandamby DH, Lung DC, Tam AR, Poon RW, Fung AY, Hung IF, Cheng VC, Chan JF, Yuen KY (2020) Consistent detection of 2019 novel coronavirus in saliva. Clin Infect Dis 71(15):841–843
van Doremalen N, Bushmaker T, Morris DH, Holbrook MG, Gamble A, Williamson BN, Tamin A, Harcourt JL, Thornburg NJ, Gerber SI, Lloyd-Smith JO, de Wit E, Munster VJ (2020) Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. N Engl J Med 382(16):1564–1567
Vlachokostas A, Burns CA, Salsbury TI, Daniel RC, James DP, Flaherty JE, Wang N, Underhill RM, Kulkarni G, Pease LF. Experimental evaluation of respiratory droplet spread to rooms connected by a central ventilation system (2022) Indoor Air 32(1):e12940
Wang CC, Prather KA, Sznitman J, Jimenez JL, Lakdawala SS, Tufekci Z, Marr LC (2021) Airborne transmission of respiratory viruses. Science 373(6558):eabd9149.
Waring MS, Siegel JA, Corsi RL (2008) Ultrafine particle removal and generation by portable air cleaners. Atmos Environ 42(20):5003–5014
Wei C, Yuan Y, Cheng Z (2020) A super-spreader of SARS-CoV-2 in incubation period among health-care workers. Respir Res 21(1):327
WHO (2009) Natural ventilation for infection control in health-care settings, World Health Organization. Available at: https://apps.who.int/iris/handle/10665/44167 . Accessed 18 Nov 2021
Xiao S, Li Y, Wong TW, Hui DSC (2017) Role of fomites in SARS transmission during the largest hospital outbreak in Hong Kong. PLoS ONE 12(7):e0181558
Zhang RY, Li YX, Zhang AL, Wang Y, Molina MJ (2020) Identifying airborne transmission as the dominant route for the spread of COVID-19. Proc Natl Acad Sci USA 117(26):14857–14863
Zhou Q, Gao Y, Wang X, Liu R, Du P, Wang X, Zhang X, Lu S, Wang Z, Shi Q, Li W, Ma Y, Luo X, Fukuoka T, Ahn HS, Lee MS, Liu E, Chen Y, Luo Z, Yang K, COVID-19 Evidence and Recommendations Working Group (2020) Nosocomial infections among patients with COVID-19, SARS and MERS: a rapid review and meta-analysis. Ann Transl Med 8(10):629
Acknowledgements
We thank all members in our Biosystems Modelling and Control Lab for their active contributions to this study.
Funding
This study was supported by the National Science and Technology Council of the Republic of China under Grant 111–2221-E-002–039.
Author information
Authors and Affiliations
Contributions
Ying-Fei Yang: methodology, data curation, software, formal analysis, writing — original draft. Yi-Jun Lin: methodology, formal analysis, writing — review and editing. Shu-Han You: methodology, formal analysis, writing — review and editing. Tien-Hsuan Lu: methodology, data curation, formal analysis, writing — review. Chi-Yun Chen: methodology, data curation, formal analysis, writing — review and editing. Wei-Min Wang: methodology, formal analysis, writing — review and editing. Chung-Min Liao: conceptualization, writing — review and editing, Supervision. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent to publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Responsible Editor: Lotfi Aleya
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yang, YF., Lin, YJ., You, SH. et al. Control measure implications of COVID-19 infection in healthcare facilities reconsidered from human physiological and engineering aspects. Environ Sci Pollut Res 30, 36228–36243 (2023). https://doi.org/10.1007/s11356-022-24815-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11356-022-24815-7